Alzheimer’s prevention may be less about new drugs, more about income, zip code and education

(Left to right) Vickie Naylor, Bernadine Clay, and Donna Maxey read a memory prompt as they take part in the Sharing History through Active Reminiscence and Photo-Imagery (SHARP) study, September 20, 2017.
That your risk of Alzheimer’s disease depends on your salary, what you ate as a child, or the block where you live may seem implausible. But researchers are discovering that social determinants of health (SDOH) play an outsized role in Alzheimer’s disease and related dementias, possibly more than age, and new strategies are emerging for how to address these factors.
At the 2022 Alzheimer’s Association International Conference, a series of presentations offered evidence that a string of socioeconomic factors—such as employment status, social support networks, education and home ownership—significantly affected dementia risk, even when adjusting data for genetic risk. What’s more, memory declined more rapidly in people who earned lower wages and slower in people who had parents of higher socioeconomic status.
In 2020, a first-of-its kind study in JAMA linked Alzheimer’s incidence to “neighborhood disadvantage,” which is based on SDOH indicators. Through autopsies, researchers analyzed brain tissue markers related to Alzheimer’s and found an association with these indicators. In 2022, Ryan Powell, the lead author of that study, published further findings that neighborhood disadvantage was connected with having more neurofibrillary tangles and amyloid plaques, the main pathological features of Alzheimer's disease.
As of yet, little is known about the biological processes behind this, says Powell, director of data science at the Center for Health Disparities Research at the University of Wisconsin School of Medicine and Public Health. “We know the association but not the direct causal pathway.”
The corroborative findings keep coming. In a Nature study published a few months after Powell’s study, every social determinant investigated affected Alzheimer’s risk except for marital status. The links were highest for income, education, and occupational status.
Clinical trials on new Alzheimer’s medications get all the headlines but preventing dementia through policy and public health interventions should not be underestimated.
The potential for prevention is significant. One in three older adults dies with Alzheimer's or another dementia—more than breast and prostate cancers combined. Further, a 2020 report from the Lancet Commission determined that about 40 percent of dementia cases could theoretically be prevented or delayed by managing the risk factors that people can modify.
Take inactivity. Older adults who took 9,800 steps daily were half as likely to develop dementia over the next 7 years, in a 2022 JAMA study. Hearing loss, another risk factor that can be managed, accounts for about 9 percent of dementia cases.
Clinical trials on new Alzheimer’s medications get all the headlines but preventing dementia through policy and public health interventions should not be underestimated. Simply slowing the course of Alzheimer’s or delaying its onset by five years would cut the incidence in half, according to the Global Council on Brain Health.
Minorities Hit the Hardest
The World Health Organization defines SDOH as “conditions in which people are born, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life.”
Anyone who exists on processed food, smokes cigarettes, or skimps on sleep has heightened risks for dementia. But minority groups get hit harder. Older Black Americans are twice as likely to have Alzheimer’s or another form of dementia as white Americans; older Hispanics are about one and a half times more likely.
This is due in part to higher rates of diabetes, obesity, and high blood pressure within these communities. These diseases are linked to Alzheimer’s, and SDOH factors multiply the risks. Blacks and Hispanics earn less income on average than white people. This means they are more likely to live in neighborhoods with limited access to healthy food, medical care, and good schools, and suffer greater exposure to noise (which impairs hearing) and air pollution—additional risk factors for dementia.
Related Reading: The Toxic Effects of Noise and What We're Not Doing About it
Plus, when Black people are diagnosed with dementia, their cognitive impairment and neuropsychiatric symptom are more advanced than in white patients. Why? Some African-Americans delay seeing a doctor because of perceived discrimination and a sense they will not be heard, says Carl V. Hill, chief diversity, equity, and inclusion officer at the Alzheimer’s Association.
Misinformation about dementia is another issue in Black communities. The thinking is that Alzheimer’s is genetic or age-related, not realizing that diet and physical activity can improve brain health, Hill says.
African Americans are severely underrepresented in clinical trials for Alzheimer’s, too. So, researchers miss the opportunity to learn more about health disparities. “It’s a bioethical issue,” Hill says. “The people most likely to have Alzheimer’s aren’t included in the trials.”
The Cure: Systemic Change
People think of lifestyle as a choice but there are limitations, says Muniza Anum Majoka, a geriatric psychiatrist and assistant professor of psychiatry at Yale University, who published an overview of SDOH factors that impact dementia. “For a lot of people, those choices [to improve brain health] are not available,” she says. If you don’t live in a safe neighborhood, for example, walking for exercise is not an option.
Hill wants to see the focus of prevention shift from individual behavior change to ensuring everyone has access to the same resources. Advice about healthy eating only goes so far if someone lives in a food desert. Systemic change also means increasing the number of minority physicians and recruiting minorities in clinical drug trials so studies will be relevant to these communities, Hill says.
Based on SDOH impact research, raising education levels has the most potential to prevent dementia. One theory is that highly educated people have a greater brain reserve that enables them to tolerate pathological changes in the brain, thus delaying dementia, says Majoka. Being curious, learning new things and problem-solving also contribute to brain health, she adds. Plus, having more education may be associated with higher socioeconomic status, more access to accurate information and healthier lifestyle choices.
New Strategies
The chasm between what researchers know about brain health and how the knowledge is being applied is huge. “There’s an explosion of interest in this area. We’re just in the first steps,” says Powell. One day, he predicts that physicians will manage Alzheimer’s through precision medicine customized to the patient’s specific risk factors and needs.
Raina Croff, assistant professor of neurology at Oregon Health & Science University School of Medicine, created the SHARP (Sharing History through Active Reminiscence and Photo-imagery) walking program to forestall memory loss in African Americans with mild cognitive impairment or early dementia.
Participants and their caregivers walk in historically black neighborhoods three times a week over six months. A smart tablet provides information about “Memory Markers” they pass, such as the route of a civil rights march. People celebrate their community and culture while “brain health is running in the background,” Croff says.

Photos and memory prompts engage participants in the SHARP program.
OHSU/Kristyna Wentz-Graff
The project began in 2015 as a pilot study in Croff’s hometown of Portland, Ore., expanded to Seattle, and will soon start in Oakland, Calif. “Walking is good for slowing [brain] decline,” she says. A post-study assessment of 40 participants in 2017 showed that half had higher cognitive scores after the program; 78 percent had lower blood pressure; and 44 percent lost weight. Those with mild cognitive impairment showed the most gains. The walkers also reported improved mood and energy along with increased involvement in other activities.
It’s never too late to reap the benefits of working your brain and being socially engaged, Majoka says.
In Milwaukee, the Wisconsin Alzheimer’s Institute launched the The Amazing Grace Chorus® to stave off cognitive decline in seniors. People in early stages of Alzheimer’s practice and perform six concerts each year. The activity provides opportunities for social engagement, mental stimulation, and a support network. Among the benefits, 55 percent reported better communication at home and nearly half of participants said they got involved with more activities after participating in the chorus.
Private companies are offering intervention services to healthcare providers and insurers to manage SDOH, too. One such service, MyHello, makes calls to at-risk people to assess their needs—be it food, transportation or simply a friendly voice. Having a social support network is critical for seniors, says Majoka, noting there was a steep decline in cognitive function among isolated elders during Covid lockdowns.
About 1 in 9 Americans age 65 or older live with Alzheimer’s today. With a surge in people with the disease predicted, public health professionals have to think more broadly about resource targets and effective intervention points, Powell says.
Beyond breakthrough pills, that is. Like Dorothy in Kansas discovering happiness was always in her own backyard, we are beginning to learn that preventing Alzheimer’s is in our reach if only we recognized it.
DNA- and RNA-based electronic implants may revolutionize healthcare
The test tubes contain tiny DNA/enzyme-based circuits, which comprise TRUMPET, a new type of electronic device, smaller than a cell.
Implantable electronic devices can significantly improve patients’ quality of life. A pacemaker can encourage the heart to beat more regularly. A neural implant, usually placed at the back of the skull, can help brain function and encourage higher neural activity. Current research on neural implants finds them helpful to patients with Parkinson’s disease, vision loss, hearing loss, and other nerve damage problems. Several of these implants, such as Elon Musk’s Neuralink, have already been approved by the FDA for human use.
Yet, pacemakers, neural implants, and other such electronic devices are not without problems. They require constant electricity, limited through batteries that need replacements. They also cause scarring. “The problem with doing this with electronics is that scar tissue forms,” explains Kate Adamala, an assistant professor of cell biology at the University of Minnesota Twin Cities. “Anytime you have something hard interacting with something soft [like muscle, skin, or tissue], the soft thing will scar. That's why there are no long-term neural implants right now.” To overcome these challenges, scientists are turning to biocomputing processes that use organic materials like DNA and RNA. Other promised benefits include “diagnostics and possibly therapeutic action, operating as nanorobots in living organisms,” writes Evgeny Katz, a professor of bioelectronics at Clarkson University, in his book DNA- And RNA-Based Computing Systems.
While a computer gives these inputs in binary code or "bits," such as a 0 or 1, biocomputing uses DNA strands as inputs, whether double or single-stranded, and often uses fluorescent RNA as an output.
Adamala’s research focuses on developing such biocomputing systems using DNA, RNA, proteins, and lipids. Using these molecules in the biocomputing systems allows the latter to be biocompatible with the human body, resulting in a natural healing process. In a recent Nature Communications study, Adamala and her team created a new biocomputing platform called TRUMPET (Transcriptional RNA Universal Multi-Purpose GatE PlaTform) which acts like a DNA-powered computer chip. “These biological systems can heal if you design them correctly,” adds Adamala. “So you can imagine a computer that will eventually heal itself.”
The basics of biocomputing
Biocomputing and regular computing have many similarities. Like regular computing, biocomputing works by running information through a series of gates, usually logic gates. A logic gate works as a fork in the road for an electronic circuit. The input will travel one way or another, giving two different outputs. An example logic gate is the AND gate, which has two inputs (A and B) and two different results. If both A and B are 1, the AND gate output will be 1. If only A is 1 and B is 0, the output will be 0 and vice versa. If both A and B are 0, the result will be 0. While a computer gives these inputs in binary code or "bits," such as a 0 or 1, biocomputing uses DNA strands as inputs, whether double or single-stranded, and often uses fluorescent RNA as an output. In this case, the DNA enters the logic gate as a single or double strand.
If the DNA is double-stranded, the system “digests” the DNA or destroys it, which results in non-fluorescence or “0” output. Conversely, if the DNA is single-stranded, it won’t be digested and instead will be copied by several enzymes in the biocomputing system, resulting in fluorescent RNA or a “1” output. And the output for this type of binary system can be expanded beyond fluorescence or not. For example, a “1” output might be the production of the enzyme insulin, while a “0” may be that no insulin is produced. “This kind of synergy between biology and computation is the essence of biocomputing,” says Stephanie Forrest, a professor and the director of the Biodesign Center for Biocomputing, Security and Society at Arizona State University.
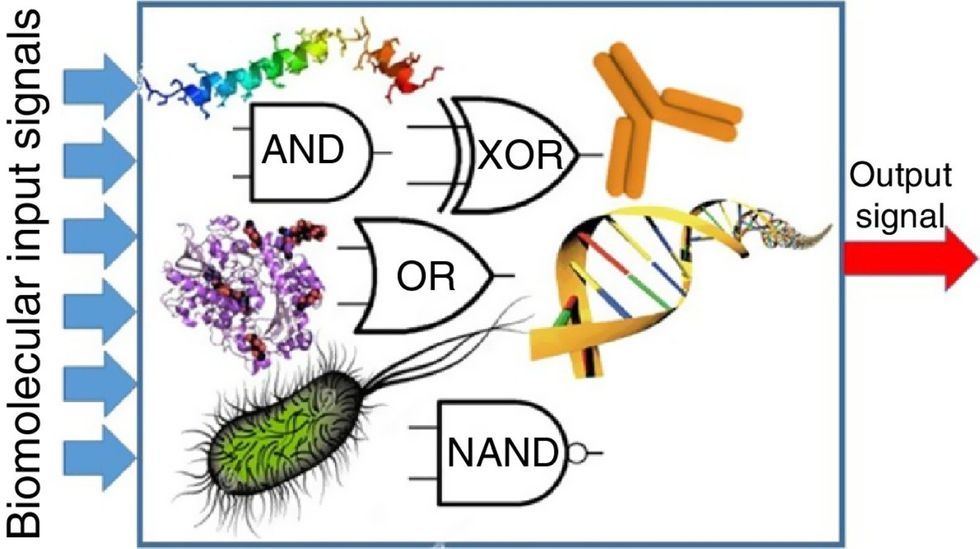
Biocomputing circles are made of DNA, RNA, proteins and even bacteria.
Evgeny Katz
The TRUMPET’s promise
Depending on whether the biocomputing system is placed directly inside a cell within the human body, or run in a test-tube, different environmental factors play a role. When an output is produced inside a cell, the cell's natural processes can amplify this output (for example, a specific protein or DNA strand), creating a solid signal. However, these cells can also be very leaky. “You want the cells to do the thing you ask them to do before they finish whatever their businesses, which is to grow, replicate, metabolize,” Adamala explains. “However, often the gate may be triggered without the right inputs, creating a false positive signal. So that's why natural logic gates are often leaky." While biocomputing outside a cell in a test tube can allow for tighter control over the logic gates, the outputs or signals cannot be amplified by a cell and are less potent.
TRUMPET, which is smaller than a cell, taps into both cellular and non-cellular biocomputing benefits. “At its core, it is a nonliving logic gate system,” Adamala states, “It's a DNA-based logic gate system. But because we use enzymes, and the readout is enzymatic [where an enzyme replicates the fluorescent RNA], we end up with signal amplification." This readout means that the output from the TRUMPET system, a fluorescent RNA strand, can be replicated by nearby enzymes in the platform, making the light signal stronger. "So it combines the best of both worlds,” Adamala adds.
These organic-based systems could detect cancer cells or low insulin levels inside a patient’s body.
The TRUMPET biocomputing process is relatively straightforward. “If the DNA [input] shows up as single-stranded, it will not be digested [by the logic gate], and you get this nice fluorescent output as the RNA is made from the single-stranded DNA, and that's a 1,” Adamala explains. "And if the DNA input is double-stranded, it gets digested by the enzymes in the logic gate, and there is no RNA created from the DNA, so there is no fluorescence, and the output is 0." On the story's leading image above, if the tube is "lit" with a purple color, that is a binary 1 signal for computing. If it's "off" it is a 0.
While still in research, TRUMPET and other biocomputing systems promise significant benefits to personalized healthcare and medicine. These organic-based systems could detect cancer cells or low insulin levels inside a patient’s body. The study’s lead author and graduate student Judee Sharon is already beginning to research TRUMPET's ability for earlier cancer diagnoses. Because the inputs for TRUMPET are single or double-stranded DNA, any mutated or cancerous DNA could theoretically be detected from the platform through the biocomputing process. Theoretically, devices like TRUMPET could be used to detect cancer and other diseases earlier.
Adamala sees TRUMPET not only as a detection system but also as a potential cancer drug delivery system. “Ideally, you would like the drug only to turn on when it senses the presence of a cancer cell. And that's how we use the logic gates, which work in response to inputs like cancerous DNA. Then the output can be the production of a small molecule or the release of a small molecule that can then go and kill what needs killing, in this case, a cancer cell. So we would like to develop applications that use this technology to control the logic gate response of a drug’s delivery to a cell.”
Although platforms like TRUMPET are making progress, a lot more work must be done before they can be used commercially. “The process of translating mechanisms and architecture from biology to computing and vice versa is still an art rather than a science,” says Forrest. “It requires deep computer science and biology knowledge,” she adds. “Some people have compared interdisciplinary science to fusion restaurants—not all combinations are successful, but when they are, the results are remarkable.”
Crickets are low on fat, high on protein, and can be farmed sustainably. They are also crunchy.
In today’s podcast episode, Leaps.org Deputy Editor Lina Zeldovich speaks about the health and ecological benefits of farming crickets for human consumption with Bicky Nguyen, who joins Lina from Vietnam. Bicky and her business partner Nam Dang operate an insect farm named CricketOne. Motivated by the idea of sustainable and healthy protein production, they started their unconventional endeavor a few years ago, despite numerous naysayers who didn’t believe that humans would ever consider munching on bugs.
Yet, making creepy crawlers part of our diet offers many health and planetary advantages. Food production needs to match the rise in global population, estimated to reach 10 billion by 2050. One challenge is that some of our current practices are inefficient, polluting and wasteful. According to nonprofit EarthSave.org, it takes 2,500 gallons of water, 12 pounds of grain, 35 pounds of topsoil and the energy equivalent of one gallon of gasoline to produce one pound of feedlot beef, although exact statistics vary between sources.
Meanwhile, insects are easy to grow, high on protein and low on fat. When roasted with salt, they make crunchy snacks. When chopped up, they transform into delicious pâtes, says Bicky, who invents her own cricket recipes and serves them at industry and public events. Maybe that’s why some research predicts that edible insects market may grow to almost $10 billion by 2030. Tune in for a delectable chat on this alternative and sustainable protein.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Further reading:
More info on Bicky Nguyen
https://yseali.fulbright.edu.vn/en/faculty/bicky-n...
The environmental footprint of beef production
https://www.earthsave.org/environment.htm
https://www.watercalculator.org/news/articles/beef-king-big-water-footprints/
https://www.frontiersin.org/articles/10.3389/fsufs.2019.00005/full
https://ourworldindata.org/carbon-footprint-food-methane
Insect farming as a source of sustainable protein
https://www.insectgourmet.com/insect-farming-growing-bugs-for-protein/
https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/insect-farming
Cricket flour is taking the world by storm
https://www.cricketflours.com/
https://talk-commerce.com/blog/what-brands-use-cricket-flour-and-why/

Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

