Is Carbon Dioxide the New Black? Yes, If These Fabric-Designing Scientists Have Their Way

The entrepreneurs Tawfiq Nasr Allah (left, standing) and Benoit Illy (right, sitting down) at Fairbrics' lab in Clichy, France.
Each year the world releases around 33 billion tons of carbon dioxide into the atmosphere. What if we could use this waste carbon dioxide to make shirts, dresses and hats? It sounds unbelievable. But two innovators are trying to tackle climate change in this truly unique way.
Chemist Tawfiq Nasr Allah set up Fairbrics with material scientist Benoît Illy in 2019. They're using waste carbon dioxide from industrial fumes as a raw material to create polyester, identical to the everyday polyester we use now. They want to take a new and very different approach to make the fashion industry more sustainable.
The Dark Side of Fast Fashion
The fashion industry is responsible for around 4% of global emissions. In a 2015 report, the MIT Materials Systems Laboratory predicted that the global impact of polyester fabric will grow from around 880 billion kg of CO2 in 2015 to 1.5 trillion kg of CO2 by 2030.
Professor Greg Peters, an expert in environmental science and sustainability, highlights the wide-ranging difficulties caused by the production of polyester. "Because it is made from petrochemical crude oil there is no real limit on how much polyester can be produced...You have to consider the ecological damage (oil spills, fracking etc.) caused by the oil and gas industry."
Many big-name brands have pledged to become carbon neutral by 2050. But nothing has really changed in the way polyester is produced.
Some companies are recycling plastic bottles into polyester. The plastic is melted into ultra-fine strands and then spun to create polyester. However, only a limited number of bottles are available. New materials must be added because of the amount of plastic degradation that takes place. Ultimately, recycling accounts for only a small percentage of the total amount of polyester produced.
Nasr Allah and Illy hope they can offer the solution the fashion industry is looking for. They are not just reducing the carbon emissions that are conventionally produced by making polyester. Their process actually goes much further. It's carbon negative and works by using up emissions from other industries.
"In a sense we imitate what nature does so well: plants capture CO2 and turn it into natural fibers using sunlight, we capture CO2 and turn it into synthetic fibers using electricity."
Experts in the field see a lot of promise. Dr Phil de Luna is an expert in carbon valorization -- the process of converting carbon dioxide into high-value chemicals. He leads a $57-million research program developing the technology to decarbonize Canada.
"I think the approach is great," he says. "Being able to take CO2 and then convert it into polymers or polyester is an excellent way to think about utilizing waste emissions and replacing fossil fuel-based materials. That is overall a net negative as compared to making polyester from fossil fuels."
From Harmful Waste to Useful Raw Material
It all started with Nasr Allah's academic research, primarily at the French Alternative Energies and Atomic Energy Commission (CEA). He spent almost 5 years investigating CO2 valorization. In essence, this involves breaking the bonds between the carbon and oxygen atoms in CO2 to create bonds with other elements.
Recycling carbon dioxide in this way requires extremely high temperatures and pressures. Catalysts are needed to break the strong bonds between the atoms. However, these are toxic, volatile and quickly lose their effectiveness over time. So, directly converting carbon dioxide into the raw material for making polyester fibers is very difficult.
Nasr Allah developed a process involving multiple simpler stages. His innovative approach involves converting carbon dioxide to intermediate chemicals. These chemicals can then be transformed into the raw material which is used in the production of polyester. After many experiments, Nasr Allah developed new processes and new catalysts that worked more effectively.
"We use a catalyst to transform CO2 into the chemicals that are used for polyester manufacturing," Illy says. "In a sense we imitate what nature does so well: plants capture CO2 and turn it into natural fibers using sunlight, we capture CO2 and turn it into synthetic fibers using electricity."
The Challenges Ahead
Nasr Allah met material scientist Illy through Entrepreneur First, a programme which pairs individuals looking to form technical start-ups. Together they set up Fairbrics and worked on converting Nasr Allah's lab findings into commercial applications and industrial success.
"The main challenge we faced was to scale up the process," Illy reveals. "[It had to be] consistent and safe to be carried out by a trained technician, not a specialist PhD as was the case in the beginning."
They recruited a team of scientists to help them develop a more effective and robust manufacturing process. Together, the team gained a more detailed theoretical understanding about what was happening at each stage of the chemical reactions. Eventually, they were able to fine tune the process and produce consistent batches of polyester.
They're making significant progress. They've produced their first samples and signed their first commercial contract to make polyester, which will then be both fabricated into clothes and sold by partner companies.
Currently, one of the largest challenges is financial. "We need to raise a fair amount to buy the equipment we need to produce at a large scale," Illy explains.
How to Power the Process?
At the moment, their main scientific focus is getting the process working reliably so they can begin commercialization. In order to remain sustainable and economically viable once they start producing polyester on a large scale, they need to consider the amount of energy they use for carbon valorization and the emissions they produce.
The more they optimize the way their catalyst works, the easier it will be to transform the CO2. The whole process can then become more cost effective and energy efficient.
De Luna explains: "My concern is...whether their process will be economical at scale. The problem is the energy cost to take carbon dioxide and transform it into these other products and that's where the science and innovation has to happen. [Whether they can scale up economically] depends on the performance of their catalyst."
They don't just need to think about the amount of energy they use to produce polyester; they also have to consider where this energy comes from.
"They need access to cheap renewable energy," De Luna says, "...so they're not using or emitting CO2 to do the conversion." If the energy they use to transform CO2 into polyester actually ends up producing more CO2, this will end up cancelling out their positive environmental impact.
Based in France, they're well located to address this issue. France has a clean electricity system, with only about 10% of their electric power coming from fossil fuels due to their reliance on nuclear energy and renewables.
Where Do They Get the Carbon Dioxide?
As they scale up, they also need to be able to access a source of CO2. They intend to obtain this from the steel industry, the cement industry, and hydrogen production.
The technology to purify and capture waste carbon dioxide from these industries is available on a large scale. However, there are only around 20 commercial operations in the world. The high cost of carbon capture means that development continues to be slow. There are a growing number of startups capturing carbon dioxide straight from the air, but this is even more costly.
One major problem is that storing captured carbon dioxide is expensive. "There are somewhat limited options for permanently storing captured CO2, so innovations like this are important,'' says T. Reed Miller, a researcher at the Yale University Center for Industrial Ecology.
Illy says: "The challenge is now to decrease the cost [of carbon capture]. By using CO2 as a raw material, we can try to increase the number of industries that capture CO2. Our goal is to turn CO2 from a waste into a valuable product."
Beyond Fashion
For Nasr Allah and Illy, fashion is just the beginning. There are many markets they can potentially break into. Next, they hope to use the polyester they've created in the packaging industry. Today, a lot of polyester is consumed to make bottles and jars. Illy believes that eventually they can produce many different chemicals from CO2. These chemicals could then be used to make paints, adhesives, and even plastics.
The Fairbrics scientists are providing a vital alternative to fossil fuels and showcasing the real potential of carbon dioxide to become a worthy resource instead of a harmful polluter.
Illy believes they can make a real difference through innovation: "We can have a significant impact in reducing climate change."
How a Deadly Fire Gave Birth to Modern Medicine
The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
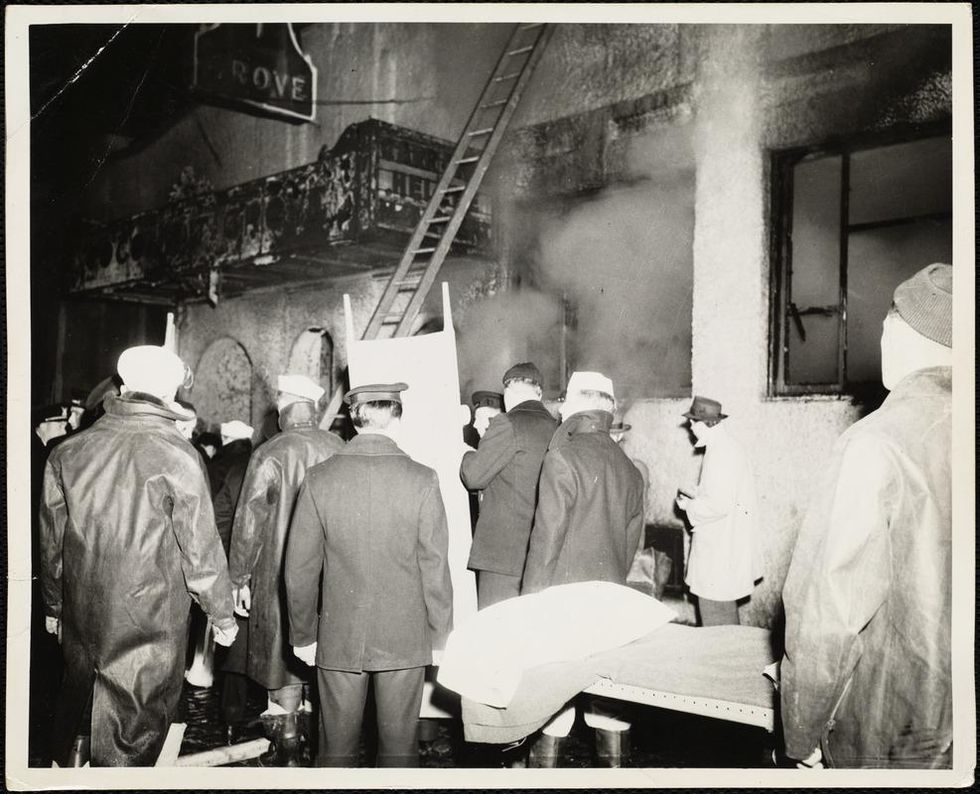
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
This Boy Struggled to Walk Before Gene Therapy. Now, Such Treatments Are Poised to Explode.
Conner Curran, now 10 years old, can walk more than two miles after gene therapy treatment for his Duchenne's muscular dystrophy.
Conner Curran was diagnosed with Duchenne's muscular dystrophy in 2015 when he was four years old. It's the most severe form of the genetic disease, with a nearly inevitable progression toward total paralysis. Many Duchenne's patients die in their teens; the average lifespan is 26.
But Conner, who is now 10, has experienced some astonishing improvements in recent years. He can now walk for more than two miles at a time – an impossible journey when he was younger.
In 2018, Conner became the very first patient to receive gene therapy specific to treating Duchenne's. In the initial clinical trial of nine children, nearly 80 percent reacted positively to the treatment). A larger-scale stage 3 clinical trial is currently underway, with initial results expected next year.
Gene therapy involves altering the genes in an individual's cells to stop or treat a disease. Such a procedure may be performed by adding new gene material to existing cells, or editing the defective genes to improve their functionality.
That the medical world is on the cusp of a successful treatment for a crippling and deadly disease is the culmination of more than 35 years of work by Dr. Jude Samulski, a professor of pharmacology at the University of North Carolina School of Medicine in Chapel Hill. More recently, he's become a leading gene therapy entrepreneur.
But Samulski likens this breakthrough to the frustrations of solving a Rubik's cube. "Just because one side is now all the color yellow does not mean that it is completely aligned," he says.
Although Conner's life and future have dramatically improved, he's not cured. The gene therapy tamed but did not extinguish his disorder: Conner is now suffering from the equivalent of Becker's muscular dystrophy, a milder form of the disease with symptoms that appear later in life and progress more slowly. Moreover, the loss of muscle cells Conner suffered prior to the treatment is permanent.
"It will take more time and more innovations," Samulski says of finding an even more effective gene therapy for muscular dystrophy.
Conner's family is still overjoyed with the results. "Jude's grit and determination gave Conner a chance at a new life, one that was not in his cards before gene therapy," says his mother Jessica Curran. She adds that "Conner is more confident than before and enjoys life, even though he has limitations, if compared to his brothers or peers."

Conner Curran holding a football post gene therapy treatment.
Courtesy of the Curran family
For now, the use of gene therapy as a treatment for diseases and disorders remains relatively isolated. On paper at least, progress appears glacially slow. In 2018, there were four FDA-approved gene therapies (excluding those reliant on bone marrow/stem cell transplants or implants). Today, there are 10. One therapy is solely for the cosmetic purpose of reducing facial lines and folds.
Nevertheless, experts in the space believe gene therapy is poised to expand dramatically.
"Certainly in the next three to five years you will see dozens of gene therapies and cell therapies be approved," says Dr. Pavan Cheruvu, who is CEO of Sio Gene Therapies in New York. The company is developing treatments for Parkinson's disease and Tay-Sachs, among other diseases.
Cheruvu's conclusion is supported by NEWDIGS, a think tank at the Massachusetts Institute of Technology that keeps tabs on gene therapy developments. NEWDIGS predicts there will be at least 60 gene therapies approved for use in the U.S. by the end of the decade. That number could be closer to 100 if Chinese researchers and biotech ventures decide the American market is a good fit for the therapies they develop.
"We are watching something of a conditional evolution, like a dot-com, or cellphones that were sizes of shoeboxes that have now matured to the size of wafers. Our space will follow along very similarly."
Dr. Carsten Brunn, a chemist by training and CEO of Selecta Biosciences outside of Boston, is developing ways to reduce the immune responses in patients who receive gene therapy. He observes that there are more than 300 therapies in development and thousands of clinical trials underway. "It's definitely an exciting time in the field," he says.
That's a far cry from the environment of little more than a decade ago. Research and investment in gene therapy had been brought low for years after the death of teenager Jesse Gelsinger in 1999 while he had been enrolled in a clinical trial to treat a liver disease. Gene therapy was a completely novel concept back then, and his death created existential questions about whether it was a proper pathway to pursue. Cheruvu, a cardiologist, calls the years after Gelsinger's death an "ice age" for gene therapy.
However, those dark years eventually yielded to a thaw. And while there have been some recent stumbles, they are considered part of the trial-and-error that has often accompanied medical research as opposed to an ominous "stop" sign.
The deaths of three patients last year receiving gene therapy for myotubular myopathy – a degenerative disease that causes severe muscle weakness – promptly ended the clinical trial in which they were enrolled. However, the incident caused few ripples beyond that. Researchers linked the deaths to dosage sizes that caused liver toxicity, as opposed to the gene therapy itself being an automatic death sentence; younger patients who received lower doses due to a less advanced disease state experienced improvements.
The gene sequencing and editing that helped create vaccines for COVID-19 in record time also bolstered the argument for more investment in research and development. Cheruvu notes that the field has usually been the domain of investors with significant expertise in the field; these days, more money is flowing in from generalists.
The Challenges Ahead
What will be the next step in gene therapy's evolution? Many of Samulski's earliest innovations came in the laboratory, for example. Then that led to him forming a company called AskBio in collaboration with the Muscular Dystrophy Association. AskBio sold its gene therapy to Pfizer five years ago to assure that enough could be manufactured for stage 3 clinical trials and eventually reach the market.
Cheruvu suggests that many future gene therapy innovations will be the result of what he calls "congruent innovation." That means publicly funded laboratories and privately funded companies might develop treatments separately or in collaboration. Or, university scientists may depend on private ventures to solve one of gene therapy's most vexing issues: producing enough finished material to test and treat on a large scale. "Manufacturing is a real bottleneck right now," Brunn says.
The alternative is referred to in the sector as the "valley of death": a lab has found a promising treatment, but is not far enough along in development to submit an investigational new drug application with the FDA. The promise withers away as a result. But the new abundance of venture capital for gene therapy has made this scenario less of an issue for private firms, some of which have received hundreds of millions of dollars in funding.
There are also numerous clinical challenges. Many gene therapies use what are known as adeno-associated virus vectors (AAVs) to deliver treatments. They are hollowed-out husks of viruses that can cause a variety of mostly mild maladies ranging from colds to pink eye. They are modified to deliver the genetic material used in the therapy. Most of these vectors trigger an antibody reaction that limits treatments to a single does or a handful of smaller ones. That can limit the potential progress for patients – an issue referred to as treatment "durability."
Although vectors from animals such as horses trigger far less of an antibody reaction in patients -- and there has been significant work done on using artificial vectors -- both are likely years away from being used on a large scale. "For the foreseeable future, AAV is the delivery system of choice," Brunn says.
Also, there will likely be demand for concurrent gene therapies that can lead to a complete cure – not only halting the progress of Duchenne's in kids like Conner Curran, but regenerating their lost muscle cells, perhaps through some form of stem cell therapy or another treatment that has yet to be devised.
Nevertheless, Samulski believes demand for imperfect treatments will be high – particularly with a disease such as muscular dystrophy, where many patients are mere months from spending the remainder of their lives in wheelchairs. But Samulski believes those therapies will also inevitably evolve into something far more effective.
"We are watching something of a conditional evolution, like a dot-com, or cellphones that were sizes of shoeboxes that have now matured to the size of wafers," he says. "Our space will follow along very similarly."
Jessica Curran will remain forever grateful for what her son has received: "Jude gave us new hope. He gave us something that is priceless – a chance to watch Conner grow up and live out his own dreams."

