The Shiny–and Potentially Dangerous—New Tool for Predicting Human Behavior

Studies of twins have played an important role in determining that genetic differences play a role in the development of differences in behavior.
[Editor's Note: This essay is in response to our current Big Question, which we posed to experts with different perspectives: "How should DNA tests for intelligence be used, if at all, by parents and educators?"]
Imagine a world in which pregnant women could go to the doctor and obtain a simple inexpensive genetic test of their unborn child that would allow them to predict how tall he or she would eventually be. The test might also tell them the child's risk for high blood pressure or heart disease.
Can we use DNA not to understand, but to predict who is going to be intelligent or extraverted or mentally ill?
Even more remarkable -- and more dangerous -- the test might predict how intelligent the child would be, or how far he or she could be expected to go in school. Or heading further out, it might predict whether he or she will be an alcoholic or a teetotaler, or straight or gay, or… you get the idea. Is this really possible? If it is, would it be a good idea? Answering these questions requires some background in a scientific field called behavior genetics.
Differences in human behavior -- intelligence, personality, mental illness, pretty much everything -- are related to genetic differences among people. Scientists have known this for 150 years, ever since Darwin's half-cousin Francis Galton first applied Shakespeare's phrase, "Nature and Nurture" to the scientific investigation of human differences. We knew about the heritability of behavior before Mendel's laws of genetics had been re-discovered at the end of the last century, and long before the structure of DNA was discovered in the 1950s. How could discoveries about genetics be made before a science of genetics even existed?
The answer is that scientists developed clever research designs that allowed them to make inferences about genetics in the absence of biological knowledge about DNA. The best-known is the twin study: identical twins are essentially clones, sharing 100 percent of their DNA, while fraternal twins are essentially siblings, sharing half. To the extent that identical twins are more similar for some trait than fraternal twins, one can infer that heredity is playing a role. Adoption studies are even more straightforward. Is the personality of an adopted child more like the biological parents she has never seen, or the adoptive parents who raised her?
Twin and adoption studies played an important role in establishing beyond any reasonable doubt that genetic differences play a role in the development of differences in behavior, but they told us very little about how the genetics of behavior actually worked. When the human genome was finally sequenced in the early 2000s, and it became easier and cheaper to obtain actual DNA from large samples of people, scientists anticipated that we would soon find the genes for intelligence, mental illness, and all the other behaviors that were known to be "heritable" in a general way.
But to everyone's amazement, the genes weren't there. It turned out that there are thousands of genes related to any given behavior, so many that they can't be counted, and each one of them has such a tiny effect that it can't be tied to meaningful biological processes. The whole scientific enterprise of understanding the genetics of behavior seemed ready to collapse, until it was rescued -- sort of -- by a new method called polygenic scores, PGS for short. Polygenic scores abandon the old task of finding the genes for complex human behavior, replacing it with black-box prediction: can we use DNA not to understand, but to predict who is going to be intelligent or extraverted or mentally ill?
Prediction from observing parents works better, and is far easier and cheaper, than anything we can do with DNA.
PGS are the shiny new toy of human genetics. From a technological standpoint they are truly amazing, and they are useful for some scientific applications that don't involve making decisions about individual people. We can obtain DNA from thousands of people, estimate the tiny relationships between individual bits of DNA and any outcome we want — height or weight or cardiac disease or IQ — and then add all those tiny effects together into a single bell-shaped score that can predict the outcome of interest. In theory, we could do this from the moment of conception.
Polygenic scores for height already work pretty well. Physicians are debating whether the PGS for heart disease are robust enough to be used in the clinic. For some behavioral traits-- the most data exist for educational attainment -- they work well enough to be scientifically interesting, if not practically useful. For traits like personality or sexual orientation, the prediction is statistically significant but nowhere close to practically meaningful. No one knows how much better any of these predictions are likely to get.
Without a doubt, PGS are an amazing feat of genomic technology, but the task they accomplish is something scientists have been able to do for a long time, and in fact it is something that our grandparents could have done pretty well. PGS are basically a new way to predict a trait in an individual by using the same trait in the individual's parents — a way of observing that the acorn doesn't fall far from the tree.
The children of tall people tend to be tall. Children of excellent athletes are athletic; children of smart people are smart; children of people with heart disease are at risk, themselves. Not every time, of course, but that is how imperfect prediction works: children of tall parents vary in their height like anyone else, but on average they are taller than the rest of us. Prediction from observing parents works better, and is far easier and cheaper, than anything we can do with DNA.
But wait a minute. Prediction from parents isn't strictly genetic. Smart parents not only pass on their genes to their kids, but they also raise them. Smart families are privileged in thousands of ways — they make more money and can send their kids to better schools. The same is true for PGS.
The ability of a genetic score to predict educational attainment depends not only on examining the relationship between certain genes and how far people go in school, but also on every personal and social characteristic that helps or hinders education: wealth, status, discrimination, you name it. The bottom line is that for any kind of prediction of human behavior, separation of genetic from environmental prediction is very difficult; ultimately it isn't possible.
Still, experts are already discussing how to use PGS to make predictions for children, and even for embryos.
This is a reminder that we really have no idea why either parents or PGS predict as well or as poorly as they do. It is easy to imagine that a PGS for educational attainment works because it is summarizing genes that code for efficient neurological development, bigger brains, and swifter problem solving, but we really don't know that. PGS could work because they are associated with being rich, or being motivated, or having light skin. It's the same for predicting from parents. We just don't know.
Still, experts are already discussing how to use PGS to make predictions for children, and even for embryos.
For example, maybe couples could fertilize multiple embryos in vitro, test their DNA, and select the one with the "best" PGS on some trait. This would be a bad idea for a lot of reasons. Such scores aren't effective enough to be very useful to parents, and to the extent they are effective, it is very difficult to know what other traits might be selected for when parents try to prioritize intelligence or attractiveness. People will no doubt try it anyway, and as a matter of reproductive freedom I can't think of any way to stop them. Fortunately, the practice probably won't have any great impact one way or another.
That brings us to the ethics of PGS, particularly in the schools. Imagine that when a child enrolls in a public school, an IQ test is given to her biological parents. Children with low-IQ parents are statistically more likely to have low IQs themselves, so they could be assigned to less demanding classrooms or vocational programs. Hopefully we agree that this would be unethical, but let's think through why.
First of all, it would be unethical because we don't know why the parents have low IQs, or why their IQs predict their children's. The parents could be from a marginalized ethnic group, recognizable by their skin color and passed on genetically to their children, so discriminating based on a parent's IQ would just be a proxy for discriminating based on skin color. Such a system would be no more than a social scientific gloss on an old-fashioned program for perpetuating economic and cognitive privilege via the educational system.
People deserve to be judged on the basis of their own behavior, not a genetic test.
Assigning children to classrooms based on genetic testing would be no different, although it would have the slight ethical advantage of being less effective. The PGS for educational attainment could reflect brain-efficiency, but it could also depend on skin color, or economic advantage, or personality, or literally anything that is related in any way to economic success. Privileging kids with higher genetic scores would be no different than privileging children with smart parents. If schools really believe that a psychological trait like IQ is important for school placement, the sensible thing is to administer the children an actual IQ test – not a genetic test.
IQ testing has its own issues, of course, but at least it involves making decisions about individuals based on their own observable characteristics, rather than on characteristics of their parents or their genome. If decisions must be made, if resources must be apportioned, people deserve to be judged on the basis of their own behavior, the content of their character. Since it can't be denied that people differ in all sorts of relevant ways, this is what it means for all people to be created equal.
[Editor's Note: Read another perspective in the series here.]
Scientists have known about and studied heart rate variability, or HRV, for a long time and, in recent years, monitors have come to market that can measure HRV accurately.
This episode is about a health metric you may not have heard of before: heart rate variability, or HRV. This refers to the small changes in the length of time between each of your heart beats.
Scientists have known about and studied HRV for a long time. In recent years, though, new monitors have come to market that can measure HRV accurately whenever you want.
Five months ago, I got interested in HRV as a more scientific approach to finding the lifestyle changes that work best for me as an individual. It's at the convergence of some important trends in health right now, such as health tech, precision health and the holistic approach in systems biology, which recognizes how interactions among different parts of the body are key to health.
But HRV is just one of many numbers worth paying attention to. For this episode of Making Sense of Science, I spoke with psychologist Dr. Leah Lagos; Dr. Jessilyn Dunn, assistant professor in biomedical engineering at Duke; and Jason Moore, the CEO of Spren and an app called Elite HRV. We talked about what HRV is, research on its benefits, how to measure it, whether it can be used to make improvements in health, and what researchers still need to learn about HRV.
*Talk to your doctor before trying anything discussed in this episode related to HRV and lifestyle changes to raise it.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Show notes
Spren - https://www.spren.com/
Elite HRV - https://elitehrv.com/
Jason Moore's Twitter - https://twitter.com/jasonmooreme?lang=en
Dr. Jessilyn Dunn's Twitter - https://twitter.com/drjessilyn?lang=en
Dr. Dunn's study on HRV, flu and common cold - https://jamanetwork.com/journals/jamanetworkopen/f...
Dr. Leah Lagos - https://drleahlagos.com/
Dr. Lagos on Star Talk - https://www.youtube.com/watch?v=jC2Q10SonV8
Research on HRV and intermittent fasting - https://pubmed.ncbi.nlm.nih.gov/33859841/
Research on HRV and Mediterranean diet - https://medicalxpress.com/news/2010-06-twin-medite...:~:text=Using%20data%20from%20the%20Emory,eating%20a%20Western%2Dtype%20diet
Devices for HRV biofeedback - https://elitehrv.com/heart-variability-monitors-an...
Benefits of HRV biofeedback - https://pubmed.ncbi.nlm.nih.gov/32385728/
HRV and cognitive performance - https://www.frontiersin.org/articles/10.3389/fnins...
HRV and emotional regulation - https://pubmed.ncbi.nlm.nih.gov/36030986/
Fortune article on HRV - https://fortune.com/well/2022/12/26/heart-rate-var...
Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
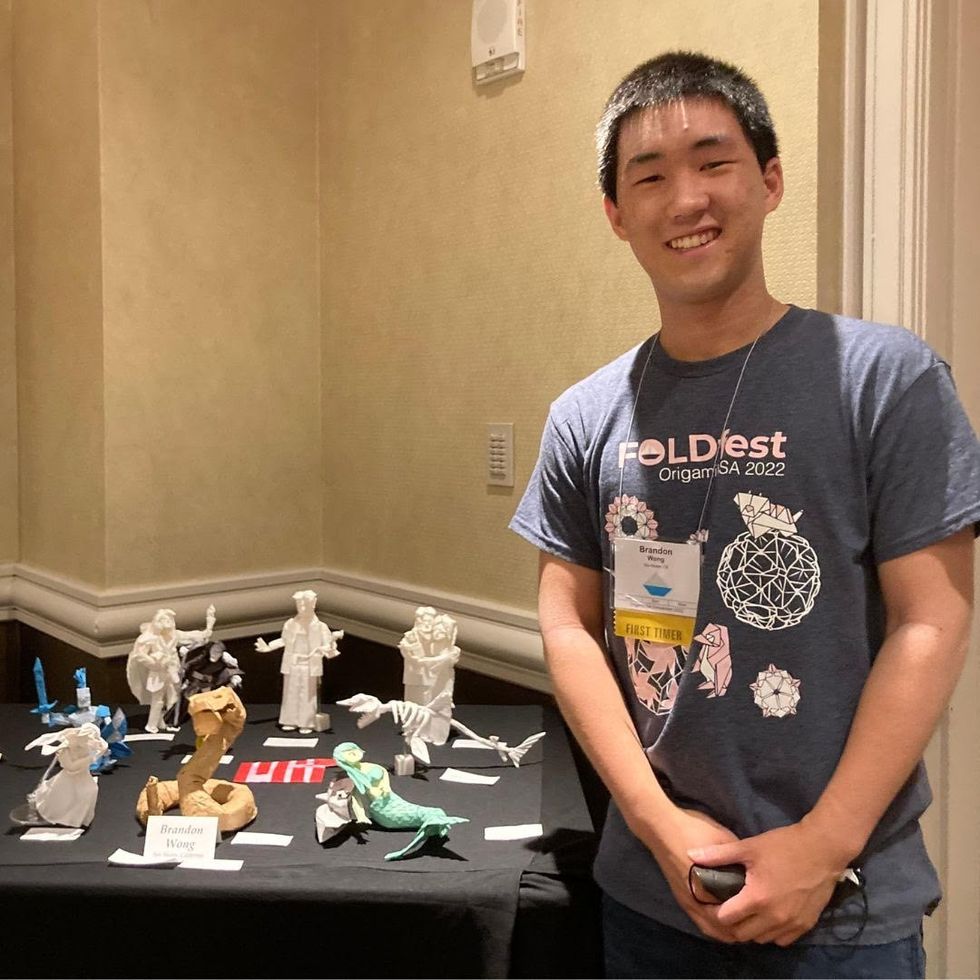
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”

