The Top Five Mysteries of the Human Gut Microbiome

A man surrounded by a cloud of bacteria, viruses, and microbes.
A scholar of science, circa 2218, might look back on this era and wonder why, all of a sudden, scientists became so obsessed with human stool. Or more accurately, the microorganisms therein.
Although every human is nearly identical genetically, each person carries around a massively different variety of microbial genes from bacteria, fungi, viruses, and archaea.
This scholar might find, for example, the seven-fold increase in PubMed articles on "gut microbiome" in the half-decade between 2012 and 2017; the plastic detritus of millions of fecal sample collection kits, and evidence that freezers in research labs worldwide had filled up with fecal samples. What's happened?
Human genome science has led to some important medical insights over time. Now it's moving over for the microorganisms. Because, although every human is nearly identical genetically, each person carries around a massively different variety of microbial genes from bacteria, fungi, viruses, and archaea—genes that are collectively called the microbiome.
Thinking that more knowledge about the gut microbiome is going to solve every problem in medicine is pure hubris. And yet these microorganisms seem to be at the nexus of humans and our environment, capable of changing us metabolically and adjusting our immune systems. What might they have the power to do?
Here are five of the most important questions that lie ahead for microbiome science.
1) What makes a gut microbiome 'healthy'?
The words "healthy microbiome" should raise a red flag. Because, currently, if scientists examine the gut microbial community of a single individual they have no way of knowing whether or not it qualifies as healthy—nor even what parameter to look at in order to find out. Is it only the names of the bugs that matter, or is it their diversity? Alternatively, is it function—what they're genetically equipped to do?
The words "healthy microbiome" should raise a red flag.
The focused efforts of the Human Microbiome Project were supposed to accomplish the apparently simple task of defining a healthy microbiome, but no clear answers emerged. If researchers could identify the parameters of a healthy microbiota per se, they might have a way to know whether manipulations—from probiotics to fecal transplant—were making a difference that could lead to a good health outcome.
2) Diet can manipulate gut microbes. How does this affect health?
"Many kinds of bacteria in our gut, they're changeable by changing our diet," says Liping Zhao of Shanghai Jiao Tong University in China, citing two large population studies from 2016. What's murkier is how this effects a change in health status.
Zhao's research focuses on making the three-way link between diet, gut microbiota, and health outcome. Meanwhile, researchers like Genelle Healey at the University of British Columbia (UBC) are working to track how the gut microbiome and health respond to a dietary intervention in a personalized way.
Knowing how the diet-induced changes in gut microbes affected health in the long term would allow every individual to toss out the diet books and figure out a dietary pattern—probably as personal as their gut microbes—that would result in their best health down the line.
If scientists could find how to harness one or more microorganisms to have specific effects on the immune system, they might be able to crack a new class of therapeutics.
3) How can gut microorganisms be used to fine-tune the immune system?
Many chronic diseases—autoimmune conditions but also, according to the latest research, obesity and cardiovascular disease—are immune mediated. Kenya Honda of Keio University School of Medicine in Tokyo, Yasmine Belkaid of the US National Institutes of Health (NIH), June Round at University of Utah, and many other researchers are chasing the ways in which gut microbes 'talk' to the immune system. But it's more than just studying certain bugs.
"It's an incredibly complex situation and we can't just label bugs as pro-inflammatory or anti-inflammatory. It's very context-dependent," says Justin Sonnenburg of Stanford. But if scientists could find how to harness a microorganism or group of them to have specific effects on the immune system, they might be able to crack a new class of therapeutics that could change the course of immune-mediated diseases.
4) How can a person's gut microbiome be reconfigured in a lasting way?
Measures of the adult microbiome over time show it has a high degree of stability—in fact, it can be downright stubborn. But a new, stable gut microbial ecology can be achieved when someone receives a fecal transplant for recurrent C. difficile infection. Work by Eric Alm of Massachusetts Institute of Technology (MIT) and others have shown the recipient's gut microbiota ends up looking more like the donor's, with engraftment of particular strains.
But what are the microorganisms' 'rules of engraftment'? Knowing this, it might be possible to intervene in a number of disease-associated microbiome states, changing them in a way that changed the course of the disease.
Is the infant microbiome, as shaped by birth mode and diet, responsible for health issues later in life?
5) How do early-life shapers of the gut microbiome affect health status later on?
Researchers have found two main factors that appear to shape the gut microbiome in early life, at least temporarily: mode of birth (whether vaginal or Cesarean section), and early life diet (whether formula or breast milk). These same factors are associated with an increased risk of immune and metabolic diseases. So is the infant microbiome, as shaped by birth mode and diet, responsible for health issues later in life?
Brett Finlay of the University of British Columbia has made these 'hygiene hypothesis' compatible links between the absence of certain bacteria in early life and asthma later on. "I think the bugs are shaping and pushing how our immune system develops, and if very early in life you don't have those things, it goes to a more allergic-type immune system. If you do have those bugs it gets pushed towards more normal," he says. The work could lead to targeted manipulation of the microbiome in early life to offset negative health effects.
DNA- and RNA-based electronic implants may revolutionize healthcare
The test tubes contain tiny DNA/enzyme-based circuits, which comprise TRUMPET, a new type of electronic device, smaller than a cell.
Implantable electronic devices can significantly improve patients’ quality of life. A pacemaker can encourage the heart to beat more regularly. A neural implant, usually placed at the back of the skull, can help brain function and encourage higher neural activity. Current research on neural implants finds them helpful to patients with Parkinson’s disease, vision loss, hearing loss, and other nerve damage problems. Several of these implants, such as Elon Musk’s Neuralink, have already been approved by the FDA for human use.
Yet, pacemakers, neural implants, and other such electronic devices are not without problems. They require constant electricity, limited through batteries that need replacements. They also cause scarring. “The problem with doing this with electronics is that scar tissue forms,” explains Kate Adamala, an assistant professor of cell biology at the University of Minnesota Twin Cities. “Anytime you have something hard interacting with something soft [like muscle, skin, or tissue], the soft thing will scar. That's why there are no long-term neural implants right now.” To overcome these challenges, scientists are turning to biocomputing processes that use organic materials like DNA and RNA. Other promised benefits include “diagnostics and possibly therapeutic action, operating as nanorobots in living organisms,” writes Evgeny Katz, a professor of bioelectronics at Clarkson University, in his book DNA- And RNA-Based Computing Systems.
While a computer gives these inputs in binary code or "bits," such as a 0 or 1, biocomputing uses DNA strands as inputs, whether double or single-stranded, and often uses fluorescent RNA as an output.
Adamala’s research focuses on developing such biocomputing systems using DNA, RNA, proteins, and lipids. Using these molecules in the biocomputing systems allows the latter to be biocompatible with the human body, resulting in a natural healing process. In a recent Nature Communications study, Adamala and her team created a new biocomputing platform called TRUMPET (Transcriptional RNA Universal Multi-Purpose GatE PlaTform) which acts like a DNA-powered computer chip. “These biological systems can heal if you design them correctly,” adds Adamala. “So you can imagine a computer that will eventually heal itself.”
The basics of biocomputing
Biocomputing and regular computing have many similarities. Like regular computing, biocomputing works by running information through a series of gates, usually logic gates. A logic gate works as a fork in the road for an electronic circuit. The input will travel one way or another, giving two different outputs. An example logic gate is the AND gate, which has two inputs (A and B) and two different results. If both A and B are 1, the AND gate output will be 1. If only A is 1 and B is 0, the output will be 0 and vice versa. If both A and B are 0, the result will be 0. While a computer gives these inputs in binary code or "bits," such as a 0 or 1, biocomputing uses DNA strands as inputs, whether double or single-stranded, and often uses fluorescent RNA as an output. In this case, the DNA enters the logic gate as a single or double strand.
If the DNA is double-stranded, the system “digests” the DNA or destroys it, which results in non-fluorescence or “0” output. Conversely, if the DNA is single-stranded, it won’t be digested and instead will be copied by several enzymes in the biocomputing system, resulting in fluorescent RNA or a “1” output. And the output for this type of binary system can be expanded beyond fluorescence or not. For example, a “1” output might be the production of the enzyme insulin, while a “0” may be that no insulin is produced. “This kind of synergy between biology and computation is the essence of biocomputing,” says Stephanie Forrest, a professor and the director of the Biodesign Center for Biocomputing, Security and Society at Arizona State University.
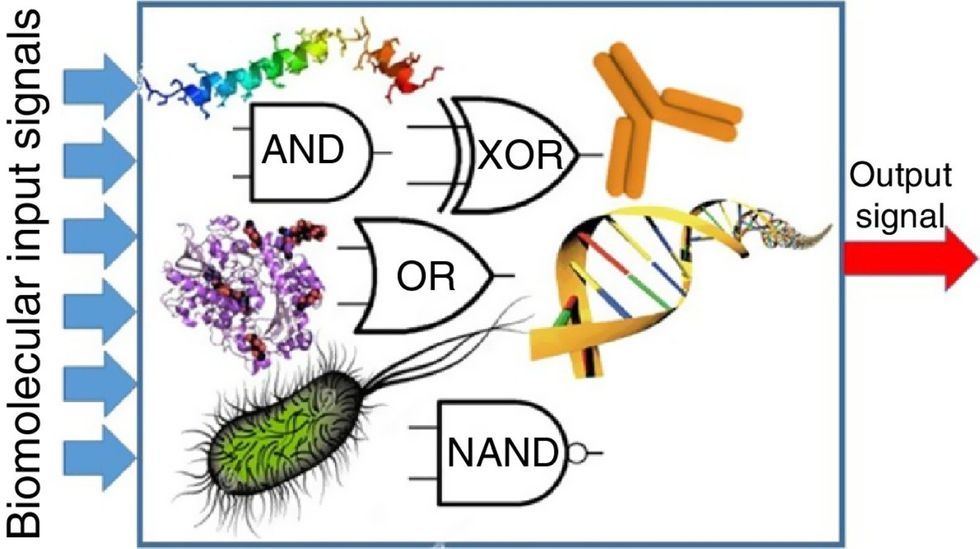
Biocomputing circles are made of DNA, RNA, proteins and even bacteria.
Evgeny Katz
The TRUMPET’s promise
Depending on whether the biocomputing system is placed directly inside a cell within the human body, or run in a test-tube, different environmental factors play a role. When an output is produced inside a cell, the cell's natural processes can amplify this output (for example, a specific protein or DNA strand), creating a solid signal. However, these cells can also be very leaky. “You want the cells to do the thing you ask them to do before they finish whatever their businesses, which is to grow, replicate, metabolize,” Adamala explains. “However, often the gate may be triggered without the right inputs, creating a false positive signal. So that's why natural logic gates are often leaky." While biocomputing outside a cell in a test tube can allow for tighter control over the logic gates, the outputs or signals cannot be amplified by a cell and are less potent.
TRUMPET, which is smaller than a cell, taps into both cellular and non-cellular biocomputing benefits. “At its core, it is a nonliving logic gate system,” Adamala states, “It's a DNA-based logic gate system. But because we use enzymes, and the readout is enzymatic [where an enzyme replicates the fluorescent RNA], we end up with signal amplification." This readout means that the output from the TRUMPET system, a fluorescent RNA strand, can be replicated by nearby enzymes in the platform, making the light signal stronger. "So it combines the best of both worlds,” Adamala adds.
These organic-based systems could detect cancer cells or low insulin levels inside a patient’s body.
The TRUMPET biocomputing process is relatively straightforward. “If the DNA [input] shows up as single-stranded, it will not be digested [by the logic gate], and you get this nice fluorescent output as the RNA is made from the single-stranded DNA, and that's a 1,” Adamala explains. "And if the DNA input is double-stranded, it gets digested by the enzymes in the logic gate, and there is no RNA created from the DNA, so there is no fluorescence, and the output is 0." On the story's leading image above, if the tube is "lit" with a purple color, that is a binary 1 signal for computing. If it's "off" it is a 0.
While still in research, TRUMPET and other biocomputing systems promise significant benefits to personalized healthcare and medicine. These organic-based systems could detect cancer cells or low insulin levels inside a patient’s body. The study’s lead author and graduate student Judee Sharon is already beginning to research TRUMPET's ability for earlier cancer diagnoses. Because the inputs for TRUMPET are single or double-stranded DNA, any mutated or cancerous DNA could theoretically be detected from the platform through the biocomputing process. Theoretically, devices like TRUMPET could be used to detect cancer and other diseases earlier.
Adamala sees TRUMPET not only as a detection system but also as a potential cancer drug delivery system. “Ideally, you would like the drug only to turn on when it senses the presence of a cancer cell. And that's how we use the logic gates, which work in response to inputs like cancerous DNA. Then the output can be the production of a small molecule or the release of a small molecule that can then go and kill what needs killing, in this case, a cancer cell. So we would like to develop applications that use this technology to control the logic gate response of a drug’s delivery to a cell.”
Although platforms like TRUMPET are making progress, a lot more work must be done before they can be used commercially. “The process of translating mechanisms and architecture from biology to computing and vice versa is still an art rather than a science,” says Forrest. “It requires deep computer science and biology knowledge,” she adds. “Some people have compared interdisciplinary science to fusion restaurants—not all combinations are successful, but when they are, the results are remarkable.”
Crickets are low on fat, high on protein, and can be farmed sustainably. They are also crunchy.
In today’s podcast episode, Leaps.org Deputy Editor Lina Zeldovich speaks about the health and ecological benefits of farming crickets for human consumption with Bicky Nguyen, who joins Lina from Vietnam. Bicky and her business partner Nam Dang operate an insect farm named CricketOne. Motivated by the idea of sustainable and healthy protein production, they started their unconventional endeavor a few years ago, despite numerous naysayers who didn’t believe that humans would ever consider munching on bugs.
Yet, making creepy crawlers part of our diet offers many health and planetary advantages. Food production needs to match the rise in global population, estimated to reach 10 billion by 2050. One challenge is that some of our current practices are inefficient, polluting and wasteful. According to nonprofit EarthSave.org, it takes 2,500 gallons of water, 12 pounds of grain, 35 pounds of topsoil and the energy equivalent of one gallon of gasoline to produce one pound of feedlot beef, although exact statistics vary between sources.
Meanwhile, insects are easy to grow, high on protein and low on fat. When roasted with salt, they make crunchy snacks. When chopped up, they transform into delicious pâtes, says Bicky, who invents her own cricket recipes and serves them at industry and public events. Maybe that’s why some research predicts that edible insects market may grow to almost $10 billion by 2030. Tune in for a delectable chat on this alternative and sustainable protein.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Further reading:
More info on Bicky Nguyen
https://yseali.fulbright.edu.vn/en/faculty/bicky-n...
The environmental footprint of beef production
https://www.earthsave.org/environment.htm
https://www.watercalculator.org/news/articles/beef-king-big-water-footprints/
https://www.frontiersin.org/articles/10.3389/fsufs.2019.00005/full
https://ourworldindata.org/carbon-footprint-food-methane
Insect farming as a source of sustainable protein
https://www.insectgourmet.com/insect-farming-growing-bugs-for-protein/
https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/insect-farming
Cricket flour is taking the world by storm
https://www.cricketflours.com/
https://talk-commerce.com/blog/what-brands-use-cricket-flour-and-why/

Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

