Debates over transgender athletes rage on, with new state bans and rules for Olympians, NCAA sports

Some argue that transgender females should be banned from competing with women in sports, while others think such bans are unfair, as the NCAA and other organizations try to keep up with research on how testosterone affects performance.
Ashley O’Connor, who was biologically male at birth but identifies as female, decided to compete in badminton as a girl during her senior year of high school in Downers Grove, Illinois. There was no team for boys, and a female friend and badminton player “practically bullied me into joining” the girls’ team. O’Connor, who is 18 and taking hormone replacement therapy for her gender transition, recalled that “it was easily one of the best decisions I have ever made.”
She believes there are many reasons why it’s important for transgender people to have the option of playing sports on the team of their choice. “It provides a sense of community,” said O’Connor, now a first-year student concentrating in psychology at the College of DuPage in Glen Ellyn, Illinois.
“It’s a great way to get a workout, which is good for physical and mental health,” she added. She also enjoyed the opportunity to be competitive, learn about her strengths and weaknesses, and just be normal. “Trans people have friends and trans people want to play sports with their friends, especially in adolescence,” she said.
However, in 18 states, many of which are politically conservative, laws prohibit transgender students from participating in sports consistent with their gender identity, according to the Movement Advancement Project, an independent, nonprofit think tank based in Boulder, Colo., that focuses on the rights of LGBTQ people. The first ban was passed in Idaho in 2020, although federal district judges have halted this legislation and a similar law in West Virginia from taking effect.
Proponents of the bans caution that transgender females would have an unfair biological advantage in competitive school sports with other girls or women as a result of being born as stronger males, potentially usurping the athletic accomplishments of other athletes.
“The future of women’s sports is at risk, and the equal rights of female athletes is being infringed,” said Penny Nance, CEO and president of Concerned Women for America, a legislative action committee in D.C. that seeks to impact culture to promote religious values.
“As the tidal wave of gender activism consumes sports from the Olympics on down, a backlash is being felt as parents are furious about the disregard for their daughters who have worked very hard to achieve success as athletes,” Nance added. “Former athletes, whose records are being shattered, are demanding answers.”
Meanwhile, opponents of the bans contend that they bar transgender athletes from playing sports with friends and learning the value of teamwork and other life lessons. These laws target transgender girls most often in kindergarten through high school but sometimes in college as well. Many local schools and state athletic associations already have their own guidelines “to both protect transgender people and ensure a level playing field for all athletes,” according to the Movement Advancement Project’s website. But statewide bans take precedence over these policies.
"It’s easy to sympathize on some level with arguments on both sides, and it’s likely going to be impossible to make everyone happy,” said Liz Joy, a past president of the American College of Sports Medicine.
In January, the National Collegiate Athletic Association (NCAA), based in Indianapolis, tried to sort out the controversy by implementing a new policy. It requires transgender students participating in female sports to prove that they’ve been taking treatments to suppress testosterone for at least one year before competition, as well as demonstrating that their testosterone level is sufficiently low, depending on the sport, through a blood test.
Then, in August, the NCAA clarified that these athletes also must take another blood test six months after their season has started that shows their testosterone levels aren’t too high. Additional guidelines will take effect next August.
Even with these requirements, “there is no plan that is going to be considered equitable and fair to all,” said Bradley Anawalt, an endocrinologist at the University of Washington School of Medicine. Biologically, he noted, there is still some evidence that a transgender female who initiates hormone therapy with estrogen and drops her testosterone to very low levels may have some advantage over other females, based on characteristics such as hand and foot size, height and perhaps strength.
Liz Joy, a past president of the American College of Sports Medicine, agrees that allowing transgender athletes to compete on teams of their self-identifying gender poses challenges. “It’s easy to sympathize on some level with arguments on both sides, and it’s likely going to be impossible to make everyone happy,” said Joy, a physician and senior medical director of wellness and nutrition at Intermountain Healthcare in Salt Lake City, Utah. While advocating for inclusion, she added that “sport was incredibly important in my life. I just want everyone to be able to benefit from it.”
One solution may be to allow transgender youth to play sports in a way that aligns with their gender identity until a certain age and before an elite level. “There are minimal or no potential financial stakes for most youth sports before age 13 or 14, and you do not have a lot of separation in athlete performance between most boys and girls until about age 13,” said Anwalt, who was a reviewer of the Endocrine Society’s national guidelines on transgender care.
Myron Genel, a professor emeritus and former chief of pediatric endocrinology at Yale School of Medicine, said it’s difficult to argue that height gives transgender females an edge because in some sports tall women already dominate over their shorter counterparts.
He added that the decision to allow transgender females to compete with other girls or women could hinge on when athletes began taking testosterone blockers. “If the process of conversion from male to female has been undertaken in the early stages of puberty, from my perspective, they have very little unique advantage,” said Genel, who advised the International Olympic Committee (IOC), based in Switzerland, on testosterone limits for transgender athletes.
Because young athletes’ bodies are still developing, “the differences in natural abilities are so massive that they would overwhelm any advantage a transgender athlete might have,” said Thomas H. Murray, president emeritus of The Hastings Center, a pioneering bioethics research institute in Garrison, New York, and author of the book “Good Sport,” which focuses on the ethics and values in the Olympics and other competitions.
“There’s no good reason to limit the participation of transgender athletes in the sports where male athletes don’t have an advantage over women,” such as sailing, archery and shooting events, Murray said. “The burden of proof rests on those who want to restrict participation by transgender athletes. They must show that in this sport, at this level of competition, transgender athletes have a conspicuous advantage.”
Last year, the IOC issued a new framework emphasizing that the Olympic rules related to transgender participation should be specific to each sport. “This is an evolving topic and there has been—as it will continue to be—new research coming out and new developments informing our approach,” and there’s currently no consensus on how testosterone affects performance across all sports, an IOC spokesperson told Leaps.org.
Many of the new laws prohibiting transgender people from competing in sports consistent with their gender identity specifically apply to transgender females. Yet, some experts say the issue also affects transgender males, nonbinary and intersex athletes.
“There has been quite a bit of attention paid to transgender females and their participation in biological female sports and almost minimal focus on transgender male competition in male sports or in any sports,” said Katherine Drabiak, associate professor of public health law and medical ethics at University of South Florida in Tampa. In fact, “transgender men, because they were born female, would be at a disadvantage of having less lean body mass, less strength and less muscular area as a general category compared to a biological male.”
While discussing transgender students’ participation in sports, it’s important to call attention to the toll that anti-transgender legislation can take on these young people’s well-being, said Jonah DeChants, a research scientist at The Trevor Project, a suicide prevention and mental health organization for LGBTQ youth. Recent polling found that 85 percent of transgender and nonbinary youth said that debates around anti-transgender laws had a negative impact on their mental health.
“The reality is simple: Most transgender girls want to play sports for the same reasons as any student—to benefit their health, to have fun, and to build connection with friends,” DeChants said. According to a new peer-reviewed qualitative study by researchers at The Trevor Project, many trans girls who participated in sports experienced harassment and stigma based on their gender identity, which can contribute to poor mental health outcomes and suicide risk.

In addition to badminton, O'Connor played other sports such as volleyball, and she plans to become an assistant coach or manager of her old high school's badminton team.
Ashley O'Connor
However, DeChants added, research also shows that young people who reported living in an accepting community, had access to LGBTQ-affirming spaces, or had social support from family and friends reported significantly lower rates of attempting suicide in the past year. “We urge coaches, educators and school administrators to seek LGBTQ-cultural competency training, implement zero tolerance policies for anti-trans bullying, and create safe, affirming environments for all transgender students on and off the field,” DeChants said.
O’Connor said her experiences on the athletic scene have been mostly positive. The politics of her community lean somewhat liberal, and she thinks it’s probably more supportive than some other areas of the country, though she noted the local library has received threats for hosting LGBTQ events. In addition to badminton, she also played baseball, lacrosse, volleyball, basketball and hockey. In the spring, she plans to become an assistant coach or manager for the girls’ badminton team at her old high school.
“When I played badminton, I never got any direct backlash from any coaches, competitors or teammates,” she said. “I had a few other teammates that identified as trans or nonbinary, [and] nearly all of the people I ever interacted with were super pleasant and treated me like any other normal person.” She added that transgender athletes “have aspirations. We have wants and needs. We have dreams. And at the end of the day, we just want to live our lives and be happy like everyone else.”
Scientists have known about and studied heart rate variability, or HRV, for a long time and, in recent years, monitors have come to market that can measure HRV accurately.
This episode is about a health metric you may not have heard of before: heart rate variability, or HRV. This refers to the small changes in the length of time between each of your heart beats.
Scientists have known about and studied HRV for a long time. In recent years, though, new monitors have come to market that can measure HRV accurately whenever you want.
Five months ago, I got interested in HRV as a more scientific approach to finding the lifestyle changes that work best for me as an individual. It's at the convergence of some important trends in health right now, such as health tech, precision health and the holistic approach in systems biology, which recognizes how interactions among different parts of the body are key to health.
But HRV is just one of many numbers worth paying attention to. For this episode of Making Sense of Science, I spoke with psychologist Dr. Leah Lagos; Dr. Jessilyn Dunn, assistant professor in biomedical engineering at Duke; and Jason Moore, the CEO of Spren and an app called Elite HRV. We talked about what HRV is, research on its benefits, how to measure it, whether it can be used to make improvements in health, and what researchers still need to learn about HRV.
*Talk to your doctor before trying anything discussed in this episode related to HRV and lifestyle changes to raise it.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Show notes
Spren - https://www.spren.com/
Elite HRV - https://elitehrv.com/
Jason Moore's Twitter - https://twitter.com/jasonmooreme?lang=en
Dr. Jessilyn Dunn's Twitter - https://twitter.com/drjessilyn?lang=en
Dr. Dunn's study on HRV, flu and common cold - https://jamanetwork.com/journals/jamanetworkopen/f...
Dr. Leah Lagos - https://drleahlagos.com/
Dr. Lagos on Star Talk - https://www.youtube.com/watch?v=jC2Q10SonV8
Research on HRV and intermittent fasting - https://pubmed.ncbi.nlm.nih.gov/33859841/
Research on HRV and Mediterranean diet - https://medicalxpress.com/news/2010-06-twin-medite...:~:text=Using%20data%20from%20the%20Emory,eating%20a%20Western%2Dtype%20diet
Devices for HRV biofeedback - https://elitehrv.com/heart-variability-monitors-an...
Benefits of HRV biofeedback - https://pubmed.ncbi.nlm.nih.gov/32385728/
HRV and cognitive performance - https://www.frontiersin.org/articles/10.3389/fnins...
HRV and emotional regulation - https://pubmed.ncbi.nlm.nih.gov/36030986/
Fortune article on HRV - https://fortune.com/well/2022/12/26/heart-rate-var...
Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
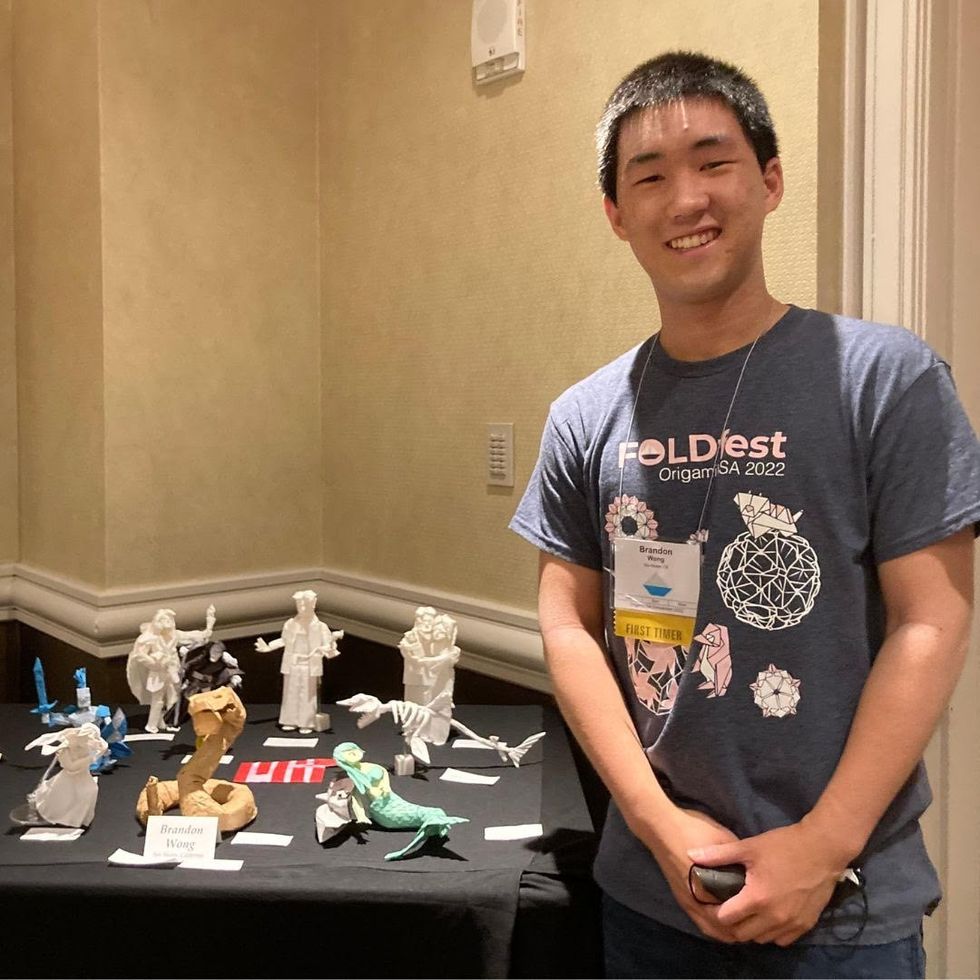
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”

