“Virtual Biopsies” May Soon Make Some Invasive Tests Unnecessary

Patient Dan Chessin met recently in Dr. Lee Ponsky's office at University Hospitals, discussing Chessin's history with prostate cancer.
At his son's college graduation in 2017, Dan Chessin felt "terribly uncomfortable" sitting in the stadium. The bouts of pain persisted, and after months of monitoring, a urologist took biopsies of suspicious areas in his prostate.
This innovation may enhance diagnostic precision and promptness, but it also brings ethical concerns to the forefront.
"In my case, the biopsies came out cancerous," says Chessin, 60, who underwent robotic surgery for intermediate-grade prostate cancer at University Hospitals Cleveland Medical Center.
Although he needed a biopsy, as most patients today do, advances in radiologic technology may make such invasive measures unnecessary in the future. Researchers are developing better imaging techniques and algorithms—a form of computer science called artificial intelligence, in which machines learn and execute tasks that typically require human brain power.
This innovation may enhance diagnostic precision and promptness. But it also brings ethical concerns to the forefront of the conversation, highlighting the potential for invasion of privacy, unequal patient access, and less physician involvement in patient care.
A National Academy of Medicine Special Publication, released in December, emphasizes that setting industry-wide standards for use in patient care is essential to AI's responsible and transparent implementation as the industry grapples with voluminous quantities of data. The technology should be viewed as a tool to supplement decision-making by highly trained professionals, not to replace it.
MRI--a test that uses powerful magnets, radio waves, and a computer to take detailed images inside the body--has become highly accurate in detecting aggressive prostate cancer, but its reliability is more limited in identifying low and intermediate grades of malignancy. That's why Chessin opted to have his prostate removed rather than take the chance of missing anything more suspicious that could develop.
His urologist, Lee Ponsky, says AI's most significant impact is yet to come. He hopes University Hospitals Cleveland Medical Center's collaboration with research scientists at its academic affiliate, Case Western Reserve University, will lead to the invention of a virtual biopsy.
A National Cancer Institute five-year grant is funding the project, launched in 2017, to develop a combined MRI and computerized tool to support more accurate detection and grading of prostate cancer. Such a tool would be "the closest to a crystal ball that we can get," says Ponsky, professor and chairman of the Urology Institute.
In situations where AI has guided diagnostics, radiologists' interpretations of breast, lung, and prostate lesions have improved as much as 25 percent, says Anant Madabhushi, a biomedical engineer and director of the Center for Computational Imaging and Personalized Diagnostics at Case Western Reserve, who is collaborating with Ponsky. "AI is very nascent," Madabhushi says, estimating that fewer than 10 percent of niche academic medical centers have used it. "We are still optimizing and validating the AI and virtual biopsy technology."
In October, several North American and European professional organizations of radiologists, imaging informaticists, and medical physicists released a joint statement on the ethics of AI. "Ultimate responsibility and accountability for AI remains with its human designers and operators for the foreseeable future," reads the statement, published in the Journal of the American College of Radiology. "The radiology community should start now to develop codes of ethics and practice for AI that promote any use that helps patients and the common good and should block use of radiology data and algorithms for financial gain without those two attributes."
Overreliance on new technology also poses concern when humans "outsource the process to a machine."
The statement's leader author, radiologist J. Raymond Geis, says "there's no question" that machines equipped with artificial intelligence "can extract more information than two human eyes" by spotting very subtle patterns in pixels. Yet, such nuances are "only part of the bigger picture of taking care of a patient," says Geis, a senior scientist with the American College of Radiology's Data Science Institute. "We have to be able to combine that with knowledge of what those pixels mean."
Setting ethical standards is high on all physicians' radar because the intricacies of each patient's medical record are factored into the computer's algorithm, which, in turn, may be used to help interpret other patients' scans, says radiologist Frank Rybicki, vice chair of operations and quality at the University of Cincinnati's department of radiology. Although obtaining patients' informed consent in writing is currently necessary, ethical dilemmas arise if and when patients have a change of heart about the use of their private health information. It is likely that removing individual data may be possible for some algorithms but not others, Rybicki says.
The information is de-identified to protect patient privacy. Using it to advance research is akin to analyzing human tissue removed in surgical procedures with the goal of discovering new medicines to fight disease, says Maryellen Giger, a University of Chicago medical physicist who studies computer-aided diagnosis in cancers of the breast, lung, and prostate, as well as bone diseases. Physicians who become adept at using AI to augment their interpretation of imaging will be ahead of the curve, she says.
As with other new discoveries, patient access and equality come into play. While AI appears to "have potential to improve over human performance in certain contexts," an algorithm's design may result in greater accuracy for certain groups of patients, says Lucia M. Rafanelli, a political theorist at The George Washington University. This "could have a disproportionately bad impact on one segment of the population."
Overreliance on new technology also poses concern when humans "outsource the process to a machine." Over time, they may cease developing and refining the skills they used before the invention became available, said Chloe Bakalar, a visiting research collaborator at Princeton University's Center for Information Technology Policy.
"AI is a paradigm shift with magic power and great potential."
Striking the right balance in the rollout of the technology is key. Rushing to integrate AI in clinical practice may cause harm, whereas holding back too long could undermine its ability to be helpful. Proper governance becomes paramount. "AI is a paradigm shift with magic power and great potential," says Ge Wang, a biomedical imaging professor at Rensselaer Polytechnic Institute in Troy, New York. "It is only ethical to develop it proactively, validate it rigorously, regulate it systematically, and optimize it as time goes by in a healthy ecosystem."
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
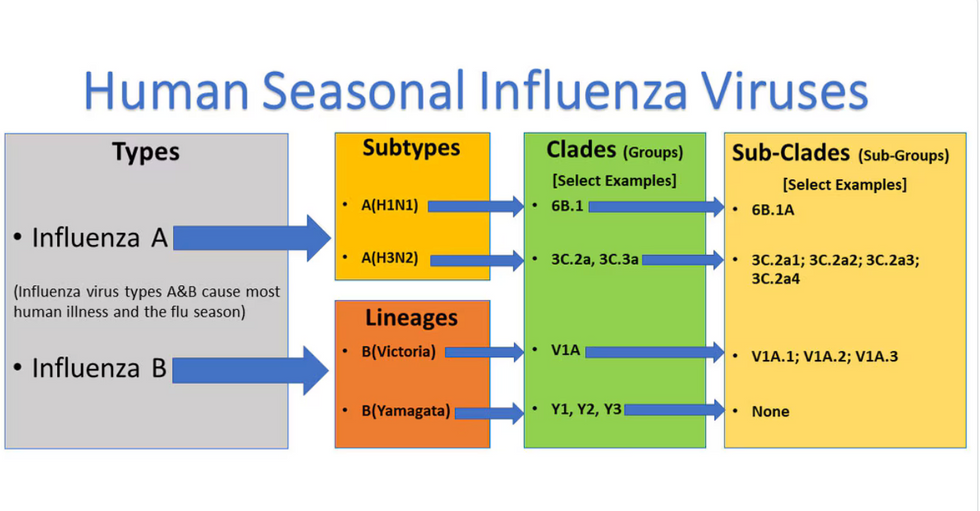
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

