What’s the Right Way to Regulate Gene-Edited Crops?

A cornfield in summer.
In the next few decades, humanity faces its biggest food crisis since the invention of the plow. The planet's population, currently 7.6 billion, is expected to reach 10 billion by 2050; to avoid mass famine, according to the World Resource Institute, we'll need to produce 70 percent more calories than we do today.
Imagine that a cheap, easy-to-use, and rapidly deployable technology could make crops more fertile and strengthen their resistance to threats.
Meanwhile, climate change will bring intensifying assaults by heat, drought, storms, pests, and weeds, depressing farm yields around the globe. Epidemics of plant disease—already laying waste to wheat, citrus, bananas, coffee, and cacao in many regions—will spread ever further through the vectors of modern trade and transportation.
So here's a thought experiment: Imagine that a cheap, easy-to-use, and rapidly deployable technology could make crops more fertile and strengthen their resistance to these looming threats. Imagine that it could also render them more nutritious and tastier, with longer shelf lives and less vulnerability to damage in shipping—adding enhancements to human health and enjoyment, as well as reduced food waste, to the possible benefits.
Finally, imagine that crops bred with the aid of this tool might carry dangers. Some could contain unsuspected allergens or toxins. Others might disrupt ecosystems, affecting the behavior or very survival of other species, or infecting wild relatives with their altered DNA.
Now ask yourself: If such a technology existed, should policymakers encourage its adoption, or ban it due to the risks? And if you chose the former alternative, how should crops developed by this method be regulated?
In fact, this technology does exist, though its use remains mostly experimental. It's called gene editing, and in the past five years it has emerged as a potentially revolutionary force in many areas—among them, treating cancer and genetic disorders; growing transplantable human organs in pigs; controlling malaria-spreading mosquitoes; and, yes, transforming agriculture. Several versions are currently available, the newest and nimblest of which goes by the acronym CRISPR.
Gene editing is far simpler and more efficient than older methods used to produce genetically modified organisms (GMOs). Unlike those methods, moreover, it can be used in ways that leave no foreign genes in the target organism—an advantage that proponents argue should comfort anyone leery of consuming so-called "Frankenfoods." But debate persists over what precautions must be taken before these crops come to market.
Recently, two of the world's most powerful regulatory bodies offered very different answers to that question. The United States Department of Agriculture (USDA) declared in March 2018 that it "does not currently regulate, or have any plans to regulate" plants that are developed through most existing methods of gene editing. The Court of Justice of the European Union (ECJ), by contrast, ruled in July that such crops should be governed by the same stringent regulations as conventional GMOs.
Some experts suggest that the broadly permissive American approach and the broadly restrictive EU policy are equally flawed.
Each announcement drew protests, for opposite reasons. Anti-GMO activists assailed the USDA's statement, arguing that all gene-edited crops should be tested and approved before marketing. "You don't know what those mutations or rearrangements might do in a plant," warned Michael Hansen, a senior scientist with the advocacy group Consumers Union. Biotech boosters griped that the ECJ's decision would stifle innovation and investment. "By any sensible standard, this judgment is illogical and absurd," wrote the British newspaper The Observer.
Yet some experts suggest that the broadly permissive American approach and the broadly restrictive EU policy are equally flawed. "What's behind these regulatory decisions is not science," says Jennifer Kuzma, co-director of the Genetic Engineering and Society Center at North Carolina State University, a former advisor to the World Economic Forum, who has researched and written extensively on governance issues in biotechnology. "It's politics, economics, and culture."
The U.S. Welcomes Gene-Edited Food
Humans have been modifying the genomes of plants and animals for 10,000 years, using selective breeding—a hit-or-miss method that can take decades or more to deliver rewards. In the mid-20th century, we learned to speed up the process by exposing organisms to radiation or mutagenic chemicals. But it wasn't until the 1980s that scientists began modifying plants by altering specific stretches of their DNA.
Today, about 90 percent of the corn, cotton and soybeans planted in the U.S. are GMOs; such crops cover nearly 4 million square miles (10 million square kilometers) of land in 29 countries. Most of these plants are transgenic, meaning they contain genes from an unrelated species—often as biologically alien as a virus or a fish. Their modifications are designed primarily to boost profit margins for mechanized agribusiness: allowing crops to withstand herbicides so that weeds can be controlled by mass spraying, for example, or to produce their own pesticides to lessen the need for chemical inputs.
In the early days, the majority of GM crops were created by extracting the gene for a desired trait from a donor organism, multiplying it, and attaching it to other snippets of DNA—usually from a microbe called an agrobacterium—that could help it infiltrate the cells of the target plant. Biotechnologists injected these particles into the target, hoping at least one would land in a place where it would perform its intended function; if not, they kept trying. The process was quicker than conventional breeding, but still complex, scattershot, and costly.
Because agrobacteria can cause plant tumors, Kuzma explains, policymakers in the U.S. decided to regulate GMO crops under an existing law, the Plant Pest Act of 1957, which addressed dangers like imported trees infested with invasive bugs. Every GMO containing the DNA of agrobacterium or another plant pest had to be tested to see whether it behaved like a pest, and undergo a lengthy approval process. By 2010, however, new methods had been developed for creating GMOs without agrobacteria; such plants could typically be marketed without pre-approval.
Soon after that, the first gene-edited crops began appearing. If old-school genetic engineering was a shotgun, techniques like TALEN and CRISPR were a scalpel—or the search-and-replace function on a computer program. With CRISPR/Cas9, for example, an enzyme that bacteria use to recognize and chop up hostile viruses is reprogrammed to find and snip out a desired bit of a plant or other organism's DNA. The enzyme can also be used to insert a substitute gene. If a DNA sequence is simply removed, or the new gene comes from a similar species, the changes in the target plant's genotype and phenotype (its general characteristics) may be no different from those that could be produced through selective breeding. If a foreign gene is added, the plant becomes a transgenic GMO.
Companies are already teeing up gene-edited products for the U.S. market, like a cooking oil and waxy corn.
This development, along with the emergence of non-agrobacterium GMOs, eventually prompted the USDA to propose a tiered regulatory system for all genetically engineered crops, beginning with an initial screening for potentially hazardous metaboloids or ecological impacts. (The screening was intended, in part, to guard against the "off-target effects"—stray mutations—that occasionally appear in gene-edited organisms.) If no red flags appeared, the crop would be approved; otherwise, it would be subject to further review, and possible regulation.
The plan was unveiled in January 2017, during the last week of the Obama presidency. Then, under the Trump administration, it was shelved. Although the USDA continues to promise a new set of regulations, the only hint of what they might contain has been Secretary of Agriculture Sonny Perdue's statement last March that gene-edited plants would remain unregulated if they "could otherwise have been developed through traditional breeding techniques, as long as they are not plant pests or developed using plant pests."
Because transgenic plants could not be "developed through traditional breeding techniques," this statement could be taken to mean that gene editing in which foreign DNA is introduced might actually be regulated. But because the USDA regulates conventional transgenic GMOs only if they trigger the plant-pest stipulation, experts assume gene-edited crops will face similarly limited oversight.
Meanwhile, companies are already teeing up gene-edited products for the U.S. market. An herbicide-resistant oilseed rape, developed using a proprietary technique, has been available since 2016. A cooking oil made from TALEN-tweaked soybeans, designed to have a healthier fatty-acid profile, is slated for release within the next few months. A CRISPR-edited "waxy" corn, designed with a starch profile ideal for processed foods, should be ready by 2021.
In all likelihood, none of these products will have to be tested for safety.
In the E.U., Stricter Rules Apply
Now let's look at the European Union. Since the late 1990s, explains Gregory Jaffe, director of the Project on Biotechnology at the Center for Science in the Public Interest, the EU has had a "process-based trigger" for genetically engineered products: "If you use recombinant DNA, you are going to be regulated." All foods and animal feeds must be approved and labeled if they consist of or contain more than 0.9 percent GM ingredients. (In the U.S., "disclosure" of GM ingredients is mandatory, if someone asks, but labeling is not required.) The only GM crop that can be commercially grown in EU member nations is a type of insect-resistant corn, though some countries allow imports.
European scientists helped develop gene editing, and they—along with the continent's biotech entrepreneurs—have been busy developing applications for crops. But European farmers seem more divided over the technology than their American counterparts. The main French agricultural trades union, for example, supports research into non-transgenic gene editing and its exemption from GMO regulation. But it was the country's small-farmers' union, the Confédération Paysanne, along with several allied groups, that in 2015 submitted a complaint to the ECJ, asking that all plants produced via mutagenesis—including gene-editing—be regulated as GMOs.
At this point, it should be mentioned that in the past 30 years, large population studies have found no sign that consuming GM foods is harmful to human health. GMO critics can, however, point to evidence that herbicide-resistant crops have encouraged overuse of herbicides, giving rise to poison-proof "superweeds," polluting the environment with suspected carcinogens, and inadvertently killing beneficial plants. Those allegations were key to the French plaintiffs' argument that gene-edited crops might similarly do unexpected harm. (Disclosure: Leapsmag's parent company, Bayer, recently acquired Monsanto, a maker of herbicides and herbicide-resistant seeds. Also, Leaps by Bayer, an innovation initiative of Bayer and Leapsmag's direct founder, has funded a biotech startup called JoynBio that aims to reduce the amount of nitrogen fertilizer required to grow crops.)
The ruling was "scientifically nonsensical. It's because of things like this that I'll never go back to Europe."
In the end, the EU court found in the Confédération's favor on gene editing—though the court maintained the regulatory exemption for mutagenesis induced by chemicals or radiation, citing the 'long safety record' of those methods.
The ruling was "scientifically nonsensical," fumes Rodolphe Barrangou, a French food scientist who pioneered CRISPR while working for DuPont in Wisconsin and is now a professor at NC State. "It's because of things like this that I'll never go back to Europe."
Nonetheless, the decision was consistent with longstanding EU policy on crops made with recombinant DNA. Given the difficulty and expense of getting such products through the continent's regulatory system, many other European researchers may wind up following Barrangou to America.
Getting to the Root of the Cultural Divide
What explains the divergence between the American and European approaches to GMOs—and, by extension, gene-edited crops? In part, Jennifer Kuzma speculates, it's that Europeans have a different attitude toward eating. "They're generally more tied to where their food comes from, where it's produced," she notes. They may also share a mistrust of government assurances on food safety, borne of the region's Mad Cow scandals of the 1980s and '90s. In Catholic countries, consumers may have misgivings about tinkering with the machinery of life.
But the principal factor, Kuzma argues, is that European and American agriculture are structured differently. "GM's benefits have mostly been designed for large-scale industrial farming and commodity crops," she says. That kind of farming is dominant in the U.S., but not in Europe, leading to a different balance of political power. In the EU, there was less pressure on decisionmakers to approve GMOs or exempt gene-edited crops from regulation—and more pressure to adopt a GM-resistant stance.
Such dynamics may be operating in other regions as well. In China, for example, the government has long encouraged research in GMOs; a state-owned company recently acquired Syngenta, a Swiss-based multinational corporation that is a leading developer of GM and gene-edited crops. GM animal feed and cooking oil can be freely imported. Yet commercial cultivation of most GM plants remains forbidden, out of deference to popular suspicions of genetically altered food. "As a new item, society has debates and doubts on GMO techniques, which is normal," President Xi Jinping remarked in 2014. "We must be bold in studying it, [but] be cautious promoting it."
The proper balance between boldness and caution is still being worked out all over the world. Europe's process-based approach may prevent researchers from developing crops that, with a single DNA snip, could rescue millions from starvation. EU regulations will also make it harder for small entrepreneurs to challenge Big Ag with a technology that, as Barrangou puts it, "can be used affordably, quickly, scalably, by anyone, without even a graduate degree in genetics." America's product-based approach, conversely, may let crops with hidden genetic dangers escape detection. And by refusing to investigate such risks, regulators may wind up exacerbating consumers' doubts about GM and gene-edited products, rather than allaying them.
"Science...can't tell you what to regulate. That's a values-based decision."
Perhaps the solution lies in combining both approaches, and adding some flexibility and nuance to the mix. "I don't believe in regulation by the product or the process," says CSPI's Jaffe. "I think you need both." Deleting a DNA base pair to silence a gene, for example, might be less risky than inserting a foreign gene into a plant—unless the deletion enables the production of an allergen, and the transgene comes from spinach.
Kuzma calls for the creation of "cooperative governance networks" to oversee crop genome editing, similar to bodies that already help develop and enforce industry standards in fisheries, electronics, industrial cleaning products, and (not incidentally) organic agriculture. Such a network could include farmers, scientists, advocacy groups, private companies, and governmental agencies. "Safety isn't an all-or-nothing concept," Kuzma says. "Science can tell you what some of the issues are in terms of risk and benefit, but it can't tell you what to regulate. That's a values-based decision."
By drawing together a wide range of stakeholders to make such decisions, she adds, "we're more likely to anticipate future consequences, and to develop a robust approach—one that not only seems more legitimate to people, but is actually just plain old better."
Have You Heard of the Best Sport for Brain Health?
In this week's Friday Five, research points to this brain healthiest of sports. Plus, the natural way to reprogram cells to a younger state, the network that could underlie many different mental illnesses, and a new test could diagnose autism in newborns. Plus, scientists 3D print an ear and attach it to woman
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- Reprogram cells to a younger state
- Pick up this sport for brain health
- Do all mental illnesses have the same underlying cause?
- New test could diagnose autism in newborns
- Scientists 3D print an ear and attach it to woman
Can blockchain help solve the Henrietta Lacks problem?
Marielle Gross, a professor at the University of Pittsburgh, shows patients a new app that tracks how their samples are used during biomedical research.
Science has come a long way since Henrietta Lacks, a Black woman from Baltimore, succumbed to cervical cancer at age 31 in 1951 -- only eight months after her diagnosis. Since then, research involving her cancer cells has advanced scientific understanding of the human papilloma virus, polio vaccines, medications for HIV/AIDS and in vitro fertilization.
Today, the World Health Organization reports that those cells are essential in mounting a COVID-19 response. But they were commercialized without the awareness or permission of Lacks or her family, who have filed a lawsuit against a biotech company for profiting from these “HeLa” cells.
While obtaining an individual's informed consent has become standard procedure before the use of tissues in medical research, many patients still don’t know what happens to their samples. Now, a new phone-based app is aiming to change that.
Tissue donors can track what scientists do with their samples while safeguarding privacy, through a pilot program initiated in October by researchers at the Johns Hopkins Berman Institute of Bioethics and the University of Pittsburgh’s Institute for Precision Medicine. The program uses blockchain technology to offer patients this opportunity through the University of Pittsburgh's Breast Disease Research Repository, while assuring that their identities remain anonymous to investigators.
A blockchain is a digital, tamper-proof ledger of transactions duplicated and distributed across a computer system network. Whenever a transaction occurs with a patient’s sample, multiple stakeholders can track it while the owner’s identity remains encrypted. Special certificates called “nonfungible tokens,” or NFTs, represent patients’ unique samples on a trusted and widely used blockchain that reinforces transparency.
Blockchain could be used to notify people if cancer researchers discover that they have certain risk factors.
“Healthcare is very data rich, but control of that data often does not lie with the patient,” said Julius Bogdan, vice president of analytics for North America at the Healthcare Information and Management Systems Society (HIMSS), a Chicago-based global technology nonprofit. “NFTs allow for the encapsulation of a patient’s data in a digital asset controlled by the patient.” He added that this technology enables a more secure and informed method of participating in clinical and research trials.
Without this technology, de-identification of patients’ samples during biomedical research had the unintended consequence of preventing them from discovering what researchers find -- even if that data could benefit their health. A solution was urgently needed, said Marielle Gross, assistant professor of obstetrics, gynecology and reproductive science and bioethics at the University of Pittsburgh School of Medicine.
“A researcher can learn something from your bio samples or medical records that could be life-saving information for you, and they have no way to let you or your doctor know,” said Gross, who is also an affiliate assistant professor at the Berman Institute. “There’s no good reason for that to stay the way that it is.”
For instance, blockchain could be used to notify people if cancer researchers discover that they have certain risk factors. Gross estimated that less than half of breast cancer patients are tested for mutations in BRCA1 and BRCA2 — tumor suppressor genes that are important in combating cancer. With normal function, these genes help prevent breast, ovarian and other cells from proliferating in an uncontrolled manner. If researchers find mutations, it’s relevant for a patient’s and family’s follow-up care — and that’s a prime example of how this newly designed app could play a life-saving role, she said.
Liz Burton was one of the first patients at the University of Pittsburgh to opt for the app -- called de-bi, which is short for decentralized biobank -- before undergoing a mastectomy for early-stage breast cancer in November, after it was diagnosed on a routine mammogram. She often takes part in medical research and looks forward to tracking her tissues.
“Anytime there’s a scientific experiment or study, I’m quick to participate -- to advance my own wellness as well as knowledge in general,” said Burton, 49, a life insurance service representative who lives in Carnegie, Pa. “It’s my way of contributing.”
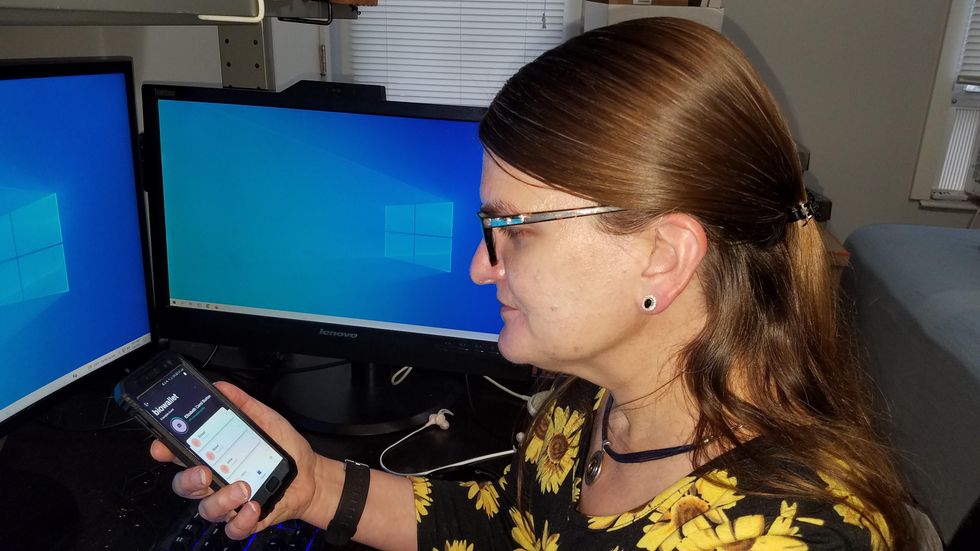
Liz Burton was one of the first patients at the University of Pittsburgh to opt for the app before undergoing a mastectomy for early-stage breast cancer.
Liz Burton
The pilot program raises the issue of what investigators may owe study participants, especially since certain populations, such as Black and indigenous peoples, historically were not treated in an ethical manner for scientific purposes. “It’s a truly laudable effort,” Tamar Schiff, a postdoctoral fellow in medical ethics at New York University’s Grossman School of Medicine, said of the endeavor. “Research participants are beautifully altruistic.”
Lauren Sankary, a bioethicist and associate director of the neuroethics program at Cleveland Clinic, agrees that the pilot program provides increased transparency for study participants regarding how scientists use their tissues while acknowledging individuals’ contributions to research.
However, she added, “it may require researchers to develop a process for ongoing communication to be responsive to additional input from research participants.”
Peter H. Schwartz, professor of medicine and director of Indiana University’s Center for Bioethics in Indianapolis, said the program is promising, but he wonders what will happen if a patient has concerns about a particular research project involving their tissues.
“I can imagine a situation where a patient objects to their sample being used for some disease they’ve never heard about, or which carries some kind of stigma like a mental illness,” Schwartz said, noting that researchers would have to evaluate how to react. “There’s no simple answer to those questions, but the technology has to be assessed with an eye to the problems it could raise.”
To truly make a difference, blockchain must enable broad consent from patients, not just de-identification.
As a result, researchers may need to factor in how much information to share with patients and how to explain it, Schiff said. There are also concerns that in tracking their samples, patients could tell others what they learned before researchers are ready to publicly release this information. However, Bogdan, the vice president of the HIMSS nonprofit, believes only a minimal study identifier would be stored in an NFT, not patient data, research results or any type of proprietary trial information.
Some patients may be confused by blockchain and reluctant to embrace it. “The complexity of NFTs may prevent the average citizen from capitalizing on their potential or vendors willing to participate in the blockchain network,” Bogdan said. “Blockchain technology is also quite costly in terms of computational power and energy consumption, contributing to greenhouse gas emissions and climate change.”
In addition, this nascent, groundbreaking technology is immature and vulnerable to data security flaws, disputes over intellectual property rights and privacy issues, though it does offer baseline protections to maintain confidentiality. To truly make a difference, blockchain must enable broad consent from patients, not just de-identification, said Robyn Shapiro, a bioethicist and founding attorney at Health Sciences Law Group near Milwaukee.
The Henrietta Lacks story is a prime example, Shapiro noted. During her treatment for cervical cancer at Johns Hopkins, Lacks’s tissue was de-identified (albeit not entirely, because her cell line, HeLa, bore her initials). After her death, those cells were replicated and distributed for important and lucrative research and product development purposes without her knowledge or consent.
Nonetheless, Shapiro thinks that the initiative by the University of Pittsburgh and Johns Hopkins has potential to solve some ethical challenges involved in research use of biospecimens. “Compared to the system that allowed Lacks’s cells to be used without her permission, Shapiro said, “blockchain technology using nonfungible tokens that allow patients to follow their samples may enhance transparency, accountability and respect for persons who contribute their tissue and clinical data for research.”
Read more about laws that have prevented people from the rights to their own cells.