What’s the Right Way to Regulate Gene-Edited Crops?

A cornfield in summer.
In the next few decades, humanity faces its biggest food crisis since the invention of the plow. The planet's population, currently 7.6 billion, is expected to reach 10 billion by 2050; to avoid mass famine, according to the World Resource Institute, we'll need to produce 70 percent more calories than we do today.
Imagine that a cheap, easy-to-use, and rapidly deployable technology could make crops more fertile and strengthen their resistance to threats.
Meanwhile, climate change will bring intensifying assaults by heat, drought, storms, pests, and weeds, depressing farm yields around the globe. Epidemics of plant disease—already laying waste to wheat, citrus, bananas, coffee, and cacao in many regions—will spread ever further through the vectors of modern trade and transportation.
So here's a thought experiment: Imagine that a cheap, easy-to-use, and rapidly deployable technology could make crops more fertile and strengthen their resistance to these looming threats. Imagine that it could also render them more nutritious and tastier, with longer shelf lives and less vulnerability to damage in shipping—adding enhancements to human health and enjoyment, as well as reduced food waste, to the possible benefits.
Finally, imagine that crops bred with the aid of this tool might carry dangers. Some could contain unsuspected allergens or toxins. Others might disrupt ecosystems, affecting the behavior or very survival of other species, or infecting wild relatives with their altered DNA.
Now ask yourself: If such a technology existed, should policymakers encourage its adoption, or ban it due to the risks? And if you chose the former alternative, how should crops developed by this method be regulated?
In fact, this technology does exist, though its use remains mostly experimental. It's called gene editing, and in the past five years it has emerged as a potentially revolutionary force in many areas—among them, treating cancer and genetic disorders; growing transplantable human organs in pigs; controlling malaria-spreading mosquitoes; and, yes, transforming agriculture. Several versions are currently available, the newest and nimblest of which goes by the acronym CRISPR.
Gene editing is far simpler and more efficient than older methods used to produce genetically modified organisms (GMOs). Unlike those methods, moreover, it can be used in ways that leave no foreign genes in the target organism—an advantage that proponents argue should comfort anyone leery of consuming so-called "Frankenfoods." But debate persists over what precautions must be taken before these crops come to market.
Recently, two of the world's most powerful regulatory bodies offered very different answers to that question. The United States Department of Agriculture (USDA) declared in March 2018 that it "does not currently regulate, or have any plans to regulate" plants that are developed through most existing methods of gene editing. The Court of Justice of the European Union (ECJ), by contrast, ruled in July that such crops should be governed by the same stringent regulations as conventional GMOs.
Some experts suggest that the broadly permissive American approach and the broadly restrictive EU policy are equally flawed.
Each announcement drew protests, for opposite reasons. Anti-GMO activists assailed the USDA's statement, arguing that all gene-edited crops should be tested and approved before marketing. "You don't know what those mutations or rearrangements might do in a plant," warned Michael Hansen, a senior scientist with the advocacy group Consumers Union. Biotech boosters griped that the ECJ's decision would stifle innovation and investment. "By any sensible standard, this judgment is illogical and absurd," wrote the British newspaper The Observer.
Yet some experts suggest that the broadly permissive American approach and the broadly restrictive EU policy are equally flawed. "What's behind these regulatory decisions is not science," says Jennifer Kuzma, co-director of the Genetic Engineering and Society Center at North Carolina State University, a former advisor to the World Economic Forum, who has researched and written extensively on governance issues in biotechnology. "It's politics, economics, and culture."
The U.S. Welcomes Gene-Edited Food
Humans have been modifying the genomes of plants and animals for 10,000 years, using selective breeding—a hit-or-miss method that can take decades or more to deliver rewards. In the mid-20th century, we learned to speed up the process by exposing organisms to radiation or mutagenic chemicals. But it wasn't until the 1980s that scientists began modifying plants by altering specific stretches of their DNA.
Today, about 90 percent of the corn, cotton and soybeans planted in the U.S. are GMOs; such crops cover nearly 4 million square miles (10 million square kilometers) of land in 29 countries. Most of these plants are transgenic, meaning they contain genes from an unrelated species—often as biologically alien as a virus or a fish. Their modifications are designed primarily to boost profit margins for mechanized agribusiness: allowing crops to withstand herbicides so that weeds can be controlled by mass spraying, for example, or to produce their own pesticides to lessen the need for chemical inputs.
In the early days, the majority of GM crops were created by extracting the gene for a desired trait from a donor organism, multiplying it, and attaching it to other snippets of DNA—usually from a microbe called an agrobacterium—that could help it infiltrate the cells of the target plant. Biotechnologists injected these particles into the target, hoping at least one would land in a place where it would perform its intended function; if not, they kept trying. The process was quicker than conventional breeding, but still complex, scattershot, and costly.
Because agrobacteria can cause plant tumors, Kuzma explains, policymakers in the U.S. decided to regulate GMO crops under an existing law, the Plant Pest Act of 1957, which addressed dangers like imported trees infested with invasive bugs. Every GMO containing the DNA of agrobacterium or another plant pest had to be tested to see whether it behaved like a pest, and undergo a lengthy approval process. By 2010, however, new methods had been developed for creating GMOs without agrobacteria; such plants could typically be marketed without pre-approval.
Soon after that, the first gene-edited crops began appearing. If old-school genetic engineering was a shotgun, techniques like TALEN and CRISPR were a scalpel—or the search-and-replace function on a computer program. With CRISPR/Cas9, for example, an enzyme that bacteria use to recognize and chop up hostile viruses is reprogrammed to find and snip out a desired bit of a plant or other organism's DNA. The enzyme can also be used to insert a substitute gene. If a DNA sequence is simply removed, or the new gene comes from a similar species, the changes in the target plant's genotype and phenotype (its general characteristics) may be no different from those that could be produced through selective breeding. If a foreign gene is added, the plant becomes a transgenic GMO.
Companies are already teeing up gene-edited products for the U.S. market, like a cooking oil and waxy corn.
This development, along with the emergence of non-agrobacterium GMOs, eventually prompted the USDA to propose a tiered regulatory system for all genetically engineered crops, beginning with an initial screening for potentially hazardous metaboloids or ecological impacts. (The screening was intended, in part, to guard against the "off-target effects"—stray mutations—that occasionally appear in gene-edited organisms.) If no red flags appeared, the crop would be approved; otherwise, it would be subject to further review, and possible regulation.
The plan was unveiled in January 2017, during the last week of the Obama presidency. Then, under the Trump administration, it was shelved. Although the USDA continues to promise a new set of regulations, the only hint of what they might contain has been Secretary of Agriculture Sonny Perdue's statement last March that gene-edited plants would remain unregulated if they "could otherwise have been developed through traditional breeding techniques, as long as they are not plant pests or developed using plant pests."
Because transgenic plants could not be "developed through traditional breeding techniques," this statement could be taken to mean that gene editing in which foreign DNA is introduced might actually be regulated. But because the USDA regulates conventional transgenic GMOs only if they trigger the plant-pest stipulation, experts assume gene-edited crops will face similarly limited oversight.
Meanwhile, companies are already teeing up gene-edited products for the U.S. market. An herbicide-resistant oilseed rape, developed using a proprietary technique, has been available since 2016. A cooking oil made from TALEN-tweaked soybeans, designed to have a healthier fatty-acid profile, is slated for release within the next few months. A CRISPR-edited "waxy" corn, designed with a starch profile ideal for processed foods, should be ready by 2021.
In all likelihood, none of these products will have to be tested for safety.
In the E.U., Stricter Rules Apply
Now let's look at the European Union. Since the late 1990s, explains Gregory Jaffe, director of the Project on Biotechnology at the Center for Science in the Public Interest, the EU has had a "process-based trigger" for genetically engineered products: "If you use recombinant DNA, you are going to be regulated." All foods and animal feeds must be approved and labeled if they consist of or contain more than 0.9 percent GM ingredients. (In the U.S., "disclosure" of GM ingredients is mandatory, if someone asks, but labeling is not required.) The only GM crop that can be commercially grown in EU member nations is a type of insect-resistant corn, though some countries allow imports.
European scientists helped develop gene editing, and they—along with the continent's biotech entrepreneurs—have been busy developing applications for crops. But European farmers seem more divided over the technology than their American counterparts. The main French agricultural trades union, for example, supports research into non-transgenic gene editing and its exemption from GMO regulation. But it was the country's small-farmers' union, the Confédération Paysanne, along with several allied groups, that in 2015 submitted a complaint to the ECJ, asking that all plants produced via mutagenesis—including gene-editing—be regulated as GMOs.
At this point, it should be mentioned that in the past 30 years, large population studies have found no sign that consuming GM foods is harmful to human health. GMO critics can, however, point to evidence that herbicide-resistant crops have encouraged overuse of herbicides, giving rise to poison-proof "superweeds," polluting the environment with suspected carcinogens, and inadvertently killing beneficial plants. Those allegations were key to the French plaintiffs' argument that gene-edited crops might similarly do unexpected harm. (Disclosure: Leapsmag's parent company, Bayer, recently acquired Monsanto, a maker of herbicides and herbicide-resistant seeds. Also, Leaps by Bayer, an innovation initiative of Bayer and Leapsmag's direct founder, has funded a biotech startup called JoynBio that aims to reduce the amount of nitrogen fertilizer required to grow crops.)
The ruling was "scientifically nonsensical. It's because of things like this that I'll never go back to Europe."
In the end, the EU court found in the Confédération's favor on gene editing—though the court maintained the regulatory exemption for mutagenesis induced by chemicals or radiation, citing the 'long safety record' of those methods.
The ruling was "scientifically nonsensical," fumes Rodolphe Barrangou, a French food scientist who pioneered CRISPR while working for DuPont in Wisconsin and is now a professor at NC State. "It's because of things like this that I'll never go back to Europe."
Nonetheless, the decision was consistent with longstanding EU policy on crops made with recombinant DNA. Given the difficulty and expense of getting such products through the continent's regulatory system, many other European researchers may wind up following Barrangou to America.
Getting to the Root of the Cultural Divide
What explains the divergence between the American and European approaches to GMOs—and, by extension, gene-edited crops? In part, Jennifer Kuzma speculates, it's that Europeans have a different attitude toward eating. "They're generally more tied to where their food comes from, where it's produced," she notes. They may also share a mistrust of government assurances on food safety, borne of the region's Mad Cow scandals of the 1980s and '90s. In Catholic countries, consumers may have misgivings about tinkering with the machinery of life.
But the principal factor, Kuzma argues, is that European and American agriculture are structured differently. "GM's benefits have mostly been designed for large-scale industrial farming and commodity crops," she says. That kind of farming is dominant in the U.S., but not in Europe, leading to a different balance of political power. In the EU, there was less pressure on decisionmakers to approve GMOs or exempt gene-edited crops from regulation—and more pressure to adopt a GM-resistant stance.
Such dynamics may be operating in other regions as well. In China, for example, the government has long encouraged research in GMOs; a state-owned company recently acquired Syngenta, a Swiss-based multinational corporation that is a leading developer of GM and gene-edited crops. GM animal feed and cooking oil can be freely imported. Yet commercial cultivation of most GM plants remains forbidden, out of deference to popular suspicions of genetically altered food. "As a new item, society has debates and doubts on GMO techniques, which is normal," President Xi Jinping remarked in 2014. "We must be bold in studying it, [but] be cautious promoting it."
The proper balance between boldness and caution is still being worked out all over the world. Europe's process-based approach may prevent researchers from developing crops that, with a single DNA snip, could rescue millions from starvation. EU regulations will also make it harder for small entrepreneurs to challenge Big Ag with a technology that, as Barrangou puts it, "can be used affordably, quickly, scalably, by anyone, without even a graduate degree in genetics." America's product-based approach, conversely, may let crops with hidden genetic dangers escape detection. And by refusing to investigate such risks, regulators may wind up exacerbating consumers' doubts about GM and gene-edited products, rather than allaying them.
"Science...can't tell you what to regulate. That's a values-based decision."
Perhaps the solution lies in combining both approaches, and adding some flexibility and nuance to the mix. "I don't believe in regulation by the product or the process," says CSPI's Jaffe. "I think you need both." Deleting a DNA base pair to silence a gene, for example, might be less risky than inserting a foreign gene into a plant—unless the deletion enables the production of an allergen, and the transgene comes from spinach.
Kuzma calls for the creation of "cooperative governance networks" to oversee crop genome editing, similar to bodies that already help develop and enforce industry standards in fisheries, electronics, industrial cleaning products, and (not incidentally) organic agriculture. Such a network could include farmers, scientists, advocacy groups, private companies, and governmental agencies. "Safety isn't an all-or-nothing concept," Kuzma says. "Science can tell you what some of the issues are in terms of risk and benefit, but it can't tell you what to regulate. That's a values-based decision."
By drawing together a wide range of stakeholders to make such decisions, she adds, "we're more likely to anticipate future consequences, and to develop a robust approach—one that not only seems more legitimate to people, but is actually just plain old better."
Want to Motivate Vaccinations? Message Optimism, Not Doom
There is a lot to be optimistic about regarding the new safe and highly effective vaccines, which are moving society closer toward the goal of close human contact once again.
After COVID-19 was declared a worldwide pandemic by the World Health Organization on March 11, 2020, life as we knew it altered dramatically and millions went into lockdown. Since then, most of the world has had to contend with masks, distancing, ventilation and cycles of lockdowns as surges flare up. Deaths from COVID-19 infection, along with economic and mental health effects from the shutdowns, have been devastating. The need for an ultimate solution -- safe and effective vaccines -- has been paramount.
On November 9, 2020 (just 8 months after the pandemic announcement), the press release for the first effective COVID-19 vaccine from Pfizer/BioNTech was issued, followed by positive announcements regarding the safety and efficacy of five other vaccines from Moderna, University of Oxford/AztraZeneca, Novavax, Johnson and Johnson and Sputnik V. The Moderna and Pfizer vaccines have earned emergency use authorization through the FDA in the United States and are being distributed. We -- after many long months -- are seeing control of the devastating COVID-19 pandemic glimmering into sight.
To be clear, these vaccine candidates for COVID-19, both authorized and not yet authorized, are highly effective and safe. In fact, across all trials and sites, all six vaccines were 100% effective in preventing hospitalizations and death from COVID-19.
All Vaccines' Phase 3 Clinical Data
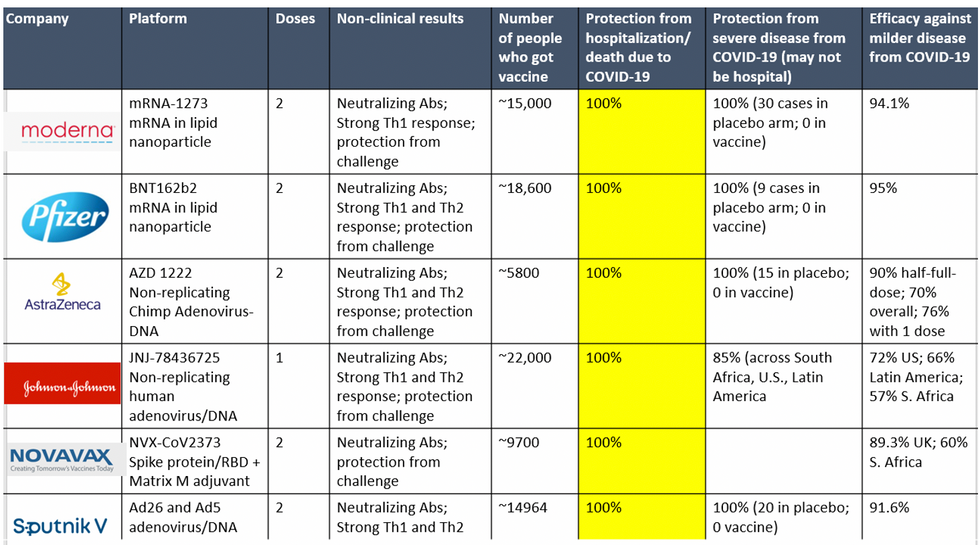
Complete protection against hospitalization and death from COVID-19 exhibited by all vaccines with phase 3 clinical trial data.
This astounding level of protection from SARS-CoV-2 from all vaccine candidates across multiple regions is likely due to robust T cell response from vaccination and will "defang" the virus from the concerns that led to COVID-19 restrictions initially: the ability of the virus to cause severe illness. This is a time of hope and optimism. After the devastating third surge of COVID-19 infections and deaths over the winter, we finally have an opportunity to stem the crisis – if only people readily accept the vaccines.
Amidst these incredible scientific advancements, however, public health officials and politicians have been pushing downright discouraging messaging. The ubiquitous talk of ongoing masks and distancing restrictions without any clear end in sight threatens to dampen uptake of the vaccines. It's imperative that we break down each concern and see if we can revitalize our public health messaging accordingly.
The first concern: we currently do not know if the vaccines block asymptomatic infection as well as symptomatic disease, since none of the phase 3 vaccine trials were set up to answer this question. However, there is biological plausibility that the antibodies and T-cell responses blocking symptomatic disease will also block asymptomatic infection in the nasal passages. IgG immunoglobulins (generated and measured by the vaccine trials) enter the nasal mucosa and systemic vaccinations generate IgA antibodies at mucosal surfaces. Monoclonal antibodies given to outpatients with COVID-19 hasten viral clearance from the airways.
Although it is prudent for those who are vaccinated to wear masks around the unvaccinated in case a slight risk of transmission remains, two fully vaccinated people can comfortably abandon masking around each other.
Moreover, data from the AztraZeneca trial (including in the phase 3 trial final results manuscript), where weekly self-swabbing was done by participants, and data from the Moderna trial, where a nasal swab was performed prior to the second dose, both showed risk reductions in asymptomatic infection with even a single dose. Finally, real-world data from a large Pfizer-based vaccine campaign in Israel shows a 50% reduction in infections (asymptomatic or symptomatic) after just the first dose.
Therefore, the likelihood of these vaccines blocking asymptomatic carriage, as well as symptomatic disease, is high. Although it is prudent for those who are vaccinated to wear masks around the unvaccinated in case a slight risk of transmission remains, two fully vaccinated people can comfortably abandon masking around each other. Moreover, as the percentage of vaccinated people increases, it will be increasingly untenable to impose restrictions on this group. Once herd immunity is reached, these restrictions can and should be abandoned altogether.
The second concern translating to "doom and gloom" messaging lately is around the identification of troubling new variants due to enhanced surveillance via viral sequencing. Four major variants circulating at this point (with others described in the past) are the B.1.1.7 variant ("UK variant"), B.1.351 ("South Africa variant), P.1. ("Brazil variant"), and the L452R variant identified in California. Although the UK variant is likely to be more transmissible, as is the South Africa variant, we have no reason to believe that masks, distancing and ventilation are ineffective against these variants.
Moreover, neutralizing antibody titers with the Pfizer and Moderna vaccines do not seem to be significantly reduced against the variants. Finally, although the Novavax 2-dose and Johnson and Johnson (J&J) 1-dose vaccines had lower rates of efficacy against moderate COVID-19 disease in South Africa, their efficacy against severe disease was impressively high. In fact J&J's vaccine still prevented 100% of hospitalizations and death from COVID-19. When combining both hospitalizations/deaths and severe symptoms managed at home, the J&J 1-dose vaccine was 85% protective across all three sites of the trial: the U.S., Latin America (including Brazil), and South Africa.
In South Africa, nearly all cases of COVID-19 (95%) were due to infection with the B.1.351 SARS-CoV-2 variant. Finally, since herd immunity does not rely on maximal immune responses among all individuals in a society, the Moderna/Pfizer/J&J vaccines are all likely to achieve that goal against variants. And thankfully, all of these vaccines can be easily modified to boost specifically against a new variant if needed (indeed, Moderna and Pfizer are already working on boosters against the prominent variants).
The third concern of some public health officials is that people will abandon all restrictions once vaccinated unless overly cautious messages are drilled into them. Indeed, the false idea that if you "give people an inch, they will take a mile" has been misinforming our messaging about mitigation since the beginning of the pandemic. For example, the very phrase "stay at home" with all of its non-applicability for essential workers and single individuals is stigmatizing and unrealistic for many. Instead, the message should have focused on how people can additively reduce their risks under different circumstances.
The public will be more inclined to trust health officials if those officials communicate with nuanced messages backed up by evidence, rather than with broad brushstrokes that shame. Therefore, we should be saying that "vaccinated people can be together with other vaccinated individuals without restrictions but must protect the unvaccinated with masks and distancing." And we can say "unvaccinated individuals should adhere to all current restrictions until vaccinated" without fear of misunderstandings. Indeed, this kind of layered advice has been communicated to people living with HIV and those without HIV for a long time (if you have HIV but partner does not, take these precautions; if both have HIV, you can do this, etc.).
Our heady progress in vaccine development, along with the incredible efficacy results of all of them, is unprecedented. However, we are at risk of undermining such progress if people balk at the vaccine because they don't believe it will make enough of a difference. One of the most critical messages we can deliver right now is that these vaccines will eventually free us from the restrictions of this pandemic. Let's use tiered messaging and clear communication to boost vaccine optimism and uptake, and get us to the goal of close human contact once again.
Inside Scoop: How a DARPA Scientist Helped Usher in a Game-Changing Covid Treatment
Amy Jenkins is a program manager for the Defense Advanced Research Projects Agency's Biological Technologies Office, which runs a project called the Pandemic Prevention Platform.
Amy Jenkins was in her office at DARPA, a research and development agency within the Department of Defense, when she first heard about a respiratory illness plaguing the Chinese city of Wuhan. Because she's a program manager for DARPA's Biological Technologies Office, her colleagues started stopping by. "It's really unusual, isn't it?" they would say.
At the time, China had a few dozen cases of what we now call COVID-19. "We should maybe keep an eye on that," she thought.
Early in 2020, still just keeping watch, she was visiting researchers working on DARPA's Pandemic Prevention Platform (P3), a project to develop treatments for "any known or previously unknown infectious threat," within 60 days of its appearance. "We looked at each other and said, 'Should we be doing something?'" she says.
For projects like P3, groups of scientists—often at universities and private companies—compete for DARPA contracts, and program managers like Jenkins oversee the work. Those that won the P3 bid included scientists at AbCellera Biologics, Inc., AstraZeneca, Duke University, and Vanderbilt University.
At the time Jenkins was talking to the P3 performers, though, they didn't have evidence of community transmission. "We would have to cross that bar before we considered doing anything," she says.
The world soon leapt far over that bar. By the time Jenkins and her team decided P3 should be doing something—with their real work beginning in late February--it was too late to prevent this pandemic. But she could help P3 dig into the chemical foundations of COVID-19's malfeasance, and cut off its roots. That work represents, in fact, her roots.
In late February 2020, DARPA received a single blood sample from a recovered COVID-19 patient, in which P3 researchers could go fishing for antibodies. The day it arrived, Jenkins's stomach roiled. "We get one shot," she thought.
Fighting the Smallest Enemies
Jenkins, who's in her early 40s, first got into germs the way many 90s kids did: by reading The Hot Zone, a novel about a hemorrhagic fever gone rogue. It wasn't exactly the disintegrating organs that hooked her. It was the idea that "these very pathogens that we can't even see can make us so sick and bring us to our knees," she says. Reading about scientists facing down deadly disease, she wondered, "How do these things make you so sick?"
She chased that question in college, majoring in both biomolecular science and chemistry, and later became an antibody expert. Antibodies are proteins that hook to a pathogen to block it from attaching to your cells, or tag it for destruction by the rest of the immune system. Soon, she jumped on the "monoclonal antibodies" train—developing synthetic versions of these natural defenses, which doctors can give to people to help them battle an early-stage infection, and even to prevent an infection from taking root after an exposure.
Jenkins likens the antibody treatments to the old aphorism about fishing: Vaccines teach your body how to fish, but antibodies simply give your body the pesca-fare. While that, as the saying goes, won't feed you for a lifetime, it will last a few weeks or months. Monoclonal antibodies thus are a promising preventative option in the immediate short-term when a vaccine hasn't yet been given (or hasn't had time to produce an immune response), as well as an important treatment weapon in the current fight. After former president Donald Trump contracted COVID-19, he received a monoclonal antibody treatment from biotech company Regeneron.
As for Jenkins, she started working as a DARPA Biological Technologies Office contractor soon after completing her postdoc. But it was a suit job, not a labcoat job. And suit jobs, at first, left Jenkins conflicted, worried about being bored. She'd give it a year, she thought. But the year expired, and bored she was not. Around five years later, in June 2019, the agency hired her to manage several of the office's programs. A year into that gig, the world was months into a pandemic.
The Pandemic Pivot
At DARPA, Jenkins inherited five programs, including P3. P3 works by taking blood from recovered people, fishing out their antibodies, identifying the most effective ones, and then figuring out how to manufacture them fast. Back then, P3 existed to help with nebulous, future outbreaks: Pandemic X. Not this pandemic. "I did not have a crystal ball," she says, "but I will say that all of us in the infectious diseases and public-health realm knew that the next pandemic was coming."
Three days after a January 2020 meeting with P3 researchers, COVID-19 appeared in Seattle, then began whipping through communities. The time had come for P3 teams to swivel. "We had done this," she says. "We had practiced this before." But would their methods stand up to something unknown, racing through the global population? "The big anxiety was, 'Wow, this was real,'" says Jenkins.
While facing down that realness, Jenkins was also managing other projects. In one called PREPARE, groups develop "medical countermeasures" that modulate a person's genetic code to boost their bodies' responses to threats. Another project, NOW, envisions shipping-container-sized factories that can make thousands of vaccine doses in days. And then there's Prometheus—which means "forethought" in Greek, and is the name of the god who stole fire and gave it to humans. Wrapping up as COVID ramped up, Prometheus aimed to identify people who are contagious—with whatever—before they start coughing, and even if they never do.
All of DARPA's projects focus on developing early-stage technology, passing it off to other agencies or industry to put it into operation. The orientation toward a specific goal appealed to Jenkins, as a contrast to academia. "You go down a rabbit hole for years at a time sometimes, chasing some concept you found interesting in the lab," she says. That's good for the human pursuit of knowledge, and leads to later applications, but DARPA wants a practical prototype—stat.
"Dual-Use" Technologies
That desire, though, and the fact that DARPA is a defense agency, present philosophical complications. "Bioethics in the national-security context turns all the dials up to 10+," says Jonathan Moreno, a medical ethicist at the University of Pennsylvania.
While developing antibody treatments to stem a pandemic seems straightforwardly good, all biological research—especially that backed by military money—requires evaluating potential knock-on applications, even those that might come from outside the entity that did the developing. As Moreno put it, "Albert Einstein wasn't thinking about blowing up Hiroshima." Particularly sensitive are so-called "dual-use" technologies—those tools that could be used for both benign and nefarious purposes, or are of interest to both the civilian and military worlds.
Moreno takes Prometheus itself as an example of "dual-use" technology. "Think about somebody wearing a suicide vest. Instead of a suicide vest, make them extremely contagious with something. The flu plus Ebola," he says. "Send them someplace, a sensitive environment. We would like to be able to defend against that"—not just tell whether Uncle Fred is bringing asymptomatic COVID home for Christmas. Prometheus, Jenkins says, had safety in mind from the get-go, and required contenders to "develop a risk mitigation plan" and "detail their strategy for appropriate control of information."
To look at a different program, if you can modulate genes to help healing, you probably know something (or know someone else could infer something) about how to hinder healing. Those sorts of risks are why PREPARE researchers got their own "ethical, legal, and social implications" panel, which meets quarterly "to ensure that we are performing all research and publications in a safe and ethical manner," says Jenkins.
DARPA as a whole, Moreno says, is institutionally sensitive to bioethics. The agency has ethics panels, and funded a 2014 National Academies assessment of how to address the "ethical, legal, and societal issues" around technology that has military relevance. "In the cases of biotechnologies where some of that research brushes up against what could legitimately be considered dual-use, that in itself justifies our investment," says Jenkins. "DARPA deliberately focuses on safety and countermeasures against potentially dangerous technologies, and we structure our programs to be transparent, safe, and legal."
Going Fishing
In late February 2020, DARPA received a single blood sample from a recovered COVID-19 patient, in which P3 researchers could go fishing for antibodies. The day it arrived, Jenkins's stomach roiled. "We get one shot," she thought.
As scientists from the P3-funded AbCellera went through the processes they'd practiced, Jenkins managed their work, tracking progress and relaying results. Soon, the team had isolated a suitable protein: bamlanivimab. It attaches to and blocks off the infamous spike proteins on SARS-CoV-2—those sticky suction-cups in illustrations. Partnering with Eli Lilly in a manufacturing agreement, the biotech company brought it to clinical trials in May, just a few months after its work on the deadly pathogen began, after much of the planet became a hot zone.
On November 10—Jenkins's favorite day at the (home) office—the FDA provided Eli Lilly emergency use authorization for bamlanivimab. But she's only mutedly screaming (with joy) inside her heart. "This pandemic isn't 'one morning we're going to wake up and it's all over,'" she says. When it is over, she and her colleagues plan to celebrate their promethean work. "I'm hoping to be able to do it in person," she says. "Until then, I have not taken a breath."

