When Are We Obligated To Edit Wild Creatures?

Cows on a pasture, who, among other mammals, could experience immense suffering from the New World screwworm.
Combining CRISPR genome editing with the natural phenomenon of gene drive allows us to rewrite the genomes of wild organisms. The benefits of saving children from malaria by editing mosquitoes are obvious and much discussed, but humans aren't the only creatures who suffer. If we gain the power to intervene in a natural world "red in tooth and claw," yet decline to use it, are we morally responsible for the animal suffering that we could have prevented?
Given the power to alter the workings of the natural world, are we morally obligated to use it?
The scenario that may redefine our relationship with the natural world begins with fine clothing. You're dressed to the nines for a formal event, but you arrived early, and it's such a beautiful day that you decided to take a stroll by the nearby lake. Suddenly, you hear the sound of splashing and screams. A child is drowning! Will you dive in to save them? Or let them die, and preserve your expensive outfit?
The philosopher Peter Singer posited this scenario to show that we are all terrible human beings. Just about everyone would save the child and ruin the outfit... leading Singer to question why so few of us give equivalent amounts of money to save children on the other side of the world. The Against Malaria Foundation averages one life saved for every $7000.
But despite having a local bias, our moral compasses aren't completely broken. You never even considered letting the child drown because the situation wasn't your fault. That's because the cause of the problem simply isn't relevant: as the one who could intervene, the consequences are on your head. We are morally responsible for intervening in situations we did not create.
There is a critical difference between Singer's original scenario and the one above: in his version, it was a muddy pond. Any adult can rescue a child from a muddy pond, but a lake is different; you can only save the child if you know how to swim. We only become morally responsible when we acquire the power to intervene.
Few would disagree with either of these moral statements, but when they are combined with increasingly powerful technologies, the implications are deeply unsettling. Given the power to alter the workings of the natural world, are we morally obligated to use it? Recent developments suggest we had best determine the answer soon because, technologically, we are learning to swim. What choices will we make?
Gene drive is a natural phenomenon that occurs when a genetic element reliably spreads through a population even though it reduces the reproductive fitness of individual organisms. Nature has evolved many different mechanisms that result in gene drive, so many that it's nearly impossible to find an organism that doesn't have at least one driving element somewhere in its genome. More than half of our own DNA comprises the broken remnants of gene drives, plus a few active copies.
Scientists have long dreamed of harnessing gene drive to block mosquito-borne disease, with little success. Then came CRISPR genome editing, which works by cutting target genes and replacing them with a new sequence. What happens if you replace the original sequence with the edited version and an encoded copy of the CRISPR system? Gene drive.

CRISPR is a molecular scalpel that we can use to cut, and therefore replace, just about any DNA sequence in any cell. Encode the instructions for the CRISPR system adjacent to the new sequence, and genome editing will occur in the reproductive cells of subsequent generations of heterozygotes, always converting the original wild-type version to the new edited version. By ensuring that offspring will all be born of one sex, or by arranging for organisms that inherit two copies of the gene drive to be sterile, it's theoretically possible to cause a population crash.
(Credit: Esvelt)
When my colleagues and I first described this technology in 2014, we initially focused on the imperative for early transparency. Gene drive research is more like civic governance than traditional technology development: you can decline a treatment recommended by your doctor, but you can’t opt out when people change the shared environment. Applying the traditional closeted model of science to gene drive actively denies people a voice in decisions intended to affect them - and reforming scientific incentives for gene drive could be the first step to making all of science faster and safer.
But open gene drive research is clearly aligned with virtually all of our values. It's when technology places our deepest moral beliefs in conflict that we struggle, and learn who we truly are.
Two of our strongest moral beliefs include our reverence for the natural world and our abhorrence of suffering. Yet some natural species inherently cause tremendous suffering. Are we morally obligated to alter or even eradicate them?
To anyone who doubts that the natural world can inflict unimaginable suffering, consider the New World screwworm.
Judging by history, the answer depends on who is doing the suffering. We view the eradication of smallpox as one of our greatest triumphs, clearly demonstrating that we value human lives over the existence of disease-causing microorganisms. The same principle holds today for malaria: few would argue against using gene drive to crash populations of malarial mosquitoes to help eradicate the disease. There are more than 3500 species of mosquitoes, only three of which would be affected, and once malaria is gone, the mosquitoes could be allowed to recover. It would be extremely surprising if African nations decided not to eradicate malaria.
The more interesting question concerns our moral obligations to animals in the state of nature.
To anyone who doubts that the natural world can inflict unimaginable suffering, consider the New World screwworm, Cochyliomyia hominivorax. Female screwworm flies lay their eggs in open wounds, generating maggots that devour healthy tissue, gluttonously burrowing into the flesh of their host until they drop, engorged and sated, to metamorphose. Yet before they fall, the maggots in a wound emit a pheromone attracting new females, thereby acting as both conductors and performers in a macabre parade that consumes the host alive. The pain is utterly excruciating, so much so that infested people often require morphine before doctors can even examine the wound. Worst of all, the New World screwworm specializes in devouring complex mammals.
Every second of every day, hundreds of millions of animals suffer the excruciating agony of being eaten alive. It has been so throughout North and South America for millions of years. Until 2001, when humanity eradicated the last screwworm fly north of Panama using the “sterile insect technique�. This was not done to protect wild animals or even people, but for economic reasons: the cost of the program was small relative to the immense damage wrought by the screwworm on North American cattle, sheep, and goats. There were no obvious ecological effects. Despite being almost completely unknown even among animal rights activists, the screwworm elimination campaign may well have been one of the greatest triumphs of animal well-being.
Unfortunately, sterile insect technique isn't powerful enough to eradicate the screwworm from South America, where it is more entrenched and protected by the rougher terrain. But gene drive is.

Contrary to news hype, gene drive alone can't cause extinction, but if combined with conventional measures it might be possible to remove targeted species from the wild. For certain species that cause immense suffering, we may be morally obligated to do just that.
(Credit: Esvelt)
South Americans may well decide to eradicate screwworm for the same economic reasons that it was eradicated from North America: the fly inflicts $4 billion in annual damages on struggling rural communities that can least afford it. It need not go extinct, of course; the existence of the sterile insect facility in Panama proves that we can maintain the screwworm indefinitely in captivity on already dead meat.
Yet if for some reason humanity chooses to leave the screwworm as it is - even for upstanding moral reasons, whatever those may be - the knowledge of our responsibility should haunt us.
Tennyson wrote,
Are God and Nature then at strife,
That Nature lends such evil dreams?
So careful of the type she seems,
So careless of the single life.
Evolution by natural selection cares nothing for the single life, nor suffering, nor euphoria, save for their utility in replication. Theoretically, we do. But how much?
[Editor's Note: This story was originally published in May 2018. We are resurfacing archive hits while our staff is on vacation.]
Have You Heard of the Best Sport for Brain Health?
In this week's Friday Five, research points to this brain healthiest of sports. Plus, the natural way to reprogram cells to a younger state, the network that could underlie many different mental illnesses, and a new test could diagnose autism in newborns. Plus, scientists 3D print an ear and attach it to woman
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- Reprogram cells to a younger state
- Pick up this sport for brain health
- Do all mental illnesses have the same underlying cause?
- New test could diagnose autism in newborns
- Scientists 3D print an ear and attach it to woman
Can blockchain help solve the Henrietta Lacks problem?
Marielle Gross, a professor at the University of Pittsburgh, shows patients a new app that tracks how their samples are used during biomedical research.
Science has come a long way since Henrietta Lacks, a Black woman from Baltimore, succumbed to cervical cancer at age 31 in 1951 -- only eight months after her diagnosis. Since then, research involving her cancer cells has advanced scientific understanding of the human papilloma virus, polio vaccines, medications for HIV/AIDS and in vitro fertilization.
Today, the World Health Organization reports that those cells are essential in mounting a COVID-19 response. But they were commercialized without the awareness or permission of Lacks or her family, who have filed a lawsuit against a biotech company for profiting from these “HeLa” cells.
While obtaining an individual's informed consent has become standard procedure before the use of tissues in medical research, many patients still don’t know what happens to their samples. Now, a new phone-based app is aiming to change that.
Tissue donors can track what scientists do with their samples while safeguarding privacy, through a pilot program initiated in October by researchers at the Johns Hopkins Berman Institute of Bioethics and the University of Pittsburgh’s Institute for Precision Medicine. The program uses blockchain technology to offer patients this opportunity through the University of Pittsburgh's Breast Disease Research Repository, while assuring that their identities remain anonymous to investigators.
A blockchain is a digital, tamper-proof ledger of transactions duplicated and distributed across a computer system network. Whenever a transaction occurs with a patient’s sample, multiple stakeholders can track it while the owner’s identity remains encrypted. Special certificates called “nonfungible tokens,” or NFTs, represent patients’ unique samples on a trusted and widely used blockchain that reinforces transparency.
Blockchain could be used to notify people if cancer researchers discover that they have certain risk factors.
“Healthcare is very data rich, but control of that data often does not lie with the patient,” said Julius Bogdan, vice president of analytics for North America at the Healthcare Information and Management Systems Society (HIMSS), a Chicago-based global technology nonprofit. “NFTs allow for the encapsulation of a patient’s data in a digital asset controlled by the patient.” He added that this technology enables a more secure and informed method of participating in clinical and research trials.
Without this technology, de-identification of patients’ samples during biomedical research had the unintended consequence of preventing them from discovering what researchers find -- even if that data could benefit their health. A solution was urgently needed, said Marielle Gross, assistant professor of obstetrics, gynecology and reproductive science and bioethics at the University of Pittsburgh School of Medicine.
“A researcher can learn something from your bio samples or medical records that could be life-saving information for you, and they have no way to let you or your doctor know,” said Gross, who is also an affiliate assistant professor at the Berman Institute. “There’s no good reason for that to stay the way that it is.”
For instance, blockchain could be used to notify people if cancer researchers discover that they have certain risk factors. Gross estimated that less than half of breast cancer patients are tested for mutations in BRCA1 and BRCA2 — tumor suppressor genes that are important in combating cancer. With normal function, these genes help prevent breast, ovarian and other cells from proliferating in an uncontrolled manner. If researchers find mutations, it’s relevant for a patient’s and family’s follow-up care — and that’s a prime example of how this newly designed app could play a life-saving role, she said.
Liz Burton was one of the first patients at the University of Pittsburgh to opt for the app -- called de-bi, which is short for decentralized biobank -- before undergoing a mastectomy for early-stage breast cancer in November, after it was diagnosed on a routine mammogram. She often takes part in medical research and looks forward to tracking her tissues.
“Anytime there’s a scientific experiment or study, I’m quick to participate -- to advance my own wellness as well as knowledge in general,” said Burton, 49, a life insurance service representative who lives in Carnegie, Pa. “It’s my way of contributing.”
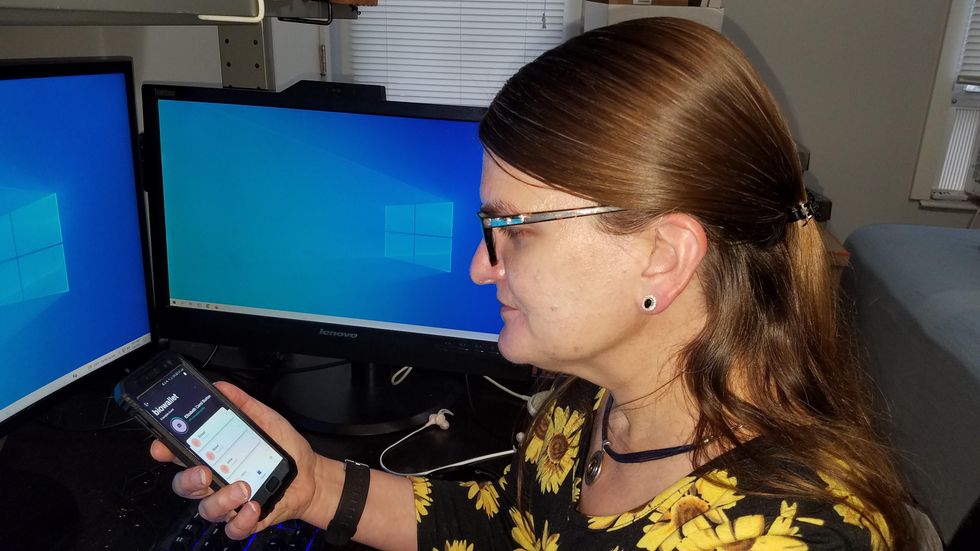
Liz Burton was one of the first patients at the University of Pittsburgh to opt for the app before undergoing a mastectomy for early-stage breast cancer.
Liz Burton
The pilot program raises the issue of what investigators may owe study participants, especially since certain populations, such as Black and indigenous peoples, historically were not treated in an ethical manner for scientific purposes. “It’s a truly laudable effort,” Tamar Schiff, a postdoctoral fellow in medical ethics at New York University’s Grossman School of Medicine, said of the endeavor. “Research participants are beautifully altruistic.”
Lauren Sankary, a bioethicist and associate director of the neuroethics program at Cleveland Clinic, agrees that the pilot program provides increased transparency for study participants regarding how scientists use their tissues while acknowledging individuals’ contributions to research.
However, she added, “it may require researchers to develop a process for ongoing communication to be responsive to additional input from research participants.”
Peter H. Schwartz, professor of medicine and director of Indiana University’s Center for Bioethics in Indianapolis, said the program is promising, but he wonders what will happen if a patient has concerns about a particular research project involving their tissues.
“I can imagine a situation where a patient objects to their sample being used for some disease they’ve never heard about, or which carries some kind of stigma like a mental illness,” Schwartz said, noting that researchers would have to evaluate how to react. “There’s no simple answer to those questions, but the technology has to be assessed with an eye to the problems it could raise.”
To truly make a difference, blockchain must enable broad consent from patients, not just de-identification.
As a result, researchers may need to factor in how much information to share with patients and how to explain it, Schiff said. There are also concerns that in tracking their samples, patients could tell others what they learned before researchers are ready to publicly release this information. However, Bogdan, the vice president of the HIMSS nonprofit, believes only a minimal study identifier would be stored in an NFT, not patient data, research results or any type of proprietary trial information.
Some patients may be confused by blockchain and reluctant to embrace it. “The complexity of NFTs may prevent the average citizen from capitalizing on their potential or vendors willing to participate in the blockchain network,” Bogdan said. “Blockchain technology is also quite costly in terms of computational power and energy consumption, contributing to greenhouse gas emissions and climate change.”
In addition, this nascent, groundbreaking technology is immature and vulnerable to data security flaws, disputes over intellectual property rights and privacy issues, though it does offer baseline protections to maintain confidentiality. To truly make a difference, blockchain must enable broad consent from patients, not just de-identification, said Robyn Shapiro, a bioethicist and founding attorney at Health Sciences Law Group near Milwaukee.
The Henrietta Lacks story is a prime example, Shapiro noted. During her treatment for cervical cancer at Johns Hopkins, Lacks’s tissue was de-identified (albeit not entirely, because her cell line, HeLa, bore her initials). After her death, those cells were replicated and distributed for important and lucrative research and product development purposes without her knowledge or consent.
Nonetheless, Shapiro thinks that the initiative by the University of Pittsburgh and Johns Hopkins has potential to solve some ethical challenges involved in research use of biospecimens. “Compared to the system that allowed Lacks’s cells to be used without her permission, Shapiro said, “blockchain technology using nonfungible tokens that allow patients to follow their samples may enhance transparency, accountability and respect for persons who contribute their tissue and clinical data for research.”
Read more about laws that have prevented people from the rights to their own cells.