Why Haven’t Researchers Developed an HIV Vaccine or Cure Yet?
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

A blood test for analysis of HIV.
Last week, top experts on HIV/AIDS convened in Amsterdam for the 22nd International AIDS conference, and the mood was not great. Even though remarkable advances in treating HIV have led to effective management for many people living with the disease, and its overall incidence has declined, there are signs that the virus could make a troubling comeback.
"In a perfect world, we'd get a vaccine like the HPV vaccine that was 100% effective and I think that's ultimately what we're going to strive for."
Growing resistance to current HIV drugs, a population boom in Sub-Saharan Africa, and insufficient public health resources are all poised to contribute to a second AIDS pandemic, according to published reports.
Already, the virus is nowhere near under control. Though the infection rate has declined 47 percent since its peak in 1996, last year 1.8 million people became newly infected with HIV around the world, and 37 million people are currently living with it. About 1 million people die of AIDS every year, making it the fourth biggest killer in low-income countries.
Leapsmag Editor-in-Chief Kira Peikoff reached out to Dr. Carl Dieffenbach, Director of the Division of AIDS at the National Institute of Allergy and Infectious Diseases, to find out what the U.S. government is doing to develop an HIV vaccine and cure. This interview has been edited and condensed for clarity.
What is the general trajectory of research in HIV/AIDS today?
We can break it down to two specific domains: focus on treatment and cure, and prevention.
Let's start with people living with HIV. This is the area where we've had the most success over the past 30 plus years, because we've taken a disease that was essentially a death sentence and converted it through the development of medications to a treatable chronic disease.
The second half of this equation is, can we cure or create a functional cure for people living with HIV? And the definition of functional cure would be the absence of circulating virus in the body in the absence of therapy. Essentially the human body would control the HIV infection within the individual. That is a much more, very early research stage of discovery. There are some interesting signals but it's still in need of innovation.
I'd like to make a contrast between what we are able to do with a virus called Hepatitis C and what we can do with the virus HIV. Hep C, with 12 weeks of highly active antiviral therapy, we can cure 95 to 100% of infections. With HIV, we cannot do that. The difference is the behavior of the virus. HIV integrates into the host's genome. Hep C is an RNA virus that stays in the cytoplasm of the cell and never gets into the DNA.
On the prevention side, we have two strategies: The first is pre-exposure prophylaxis. Then of course, we have the need for a safe, effective and durable HIV vaccine, which is a very active area of discovery. We've had some spectacular success with RV144, and we're following up on that success, and other vaccines are in the pipeline. Whether they are sufficient to provide the level of durability and activity is not yet clear, but progress has been made and there's still the need for innovation.
The most important breakthrough in the past 5 to 10 years has been the discovery of broad neutralizing monoclonal antibodies. They are proteins that the body makes, and not everybody who's HIV infected makes these antibodies, but we've been able to clone out these antibodies from certain individuals that are highly potent, and when used either singly or in combination, can truly neutralize the vast majority of HIV strains. Can those be used by themselves as treatment or as prevention? That is the question.
Can you explain more about RV144 and why you consider it a success?
Prior to RV144, we had run a number of vaccine studies and nothing had ever statistically shown to be protective. RV144 showed a level of efficacy of about 31 percent, which was statistically significant. Not enough to take forward into other studies, but it allowed us to generate some ideas about why this worked, go back to the drawing board, and redesign the immunogens to optimize and test the next generation for this vaccine. We just recently opened that new study, the follow-up to RV144, called HVTN702. That's up and enrolling and moving along quite nicely.

Carl Dieffenbach, Director of the Division of AIDS at the National Institute of Allergy and Infectious Diseases
(Courtesy)
Where is that enrolling?
Primarily in Sub-Saharan Africa and South Africa.
When will you expect to see signals from that?
Between 2020 and 2021. It's complicated because the signal also takes into account the durability. After a certain time of vaccination, we're going to count up endpoints.
How would you explain the main scientific obstacle in the way of creating a very efficacious HIV vaccine?
Simply put, it's the black box of the human immune system. HIV employs a shield technology, and the virus is constantly changing its shield to protect itself, but there are some key parts of the virus that it cannot shield, so that's the trick – to be able to target that.
So, you're trying to find the Achilles' Heel of the virus?
Exactly. To make a flu vaccine or a Zika vaccine or even an Ebola vaccine, the virus is a little bit more forthcoming with the target. In HIV, the virus does everything in its power to hide the target, so we're dealing with a well-adapted [adversary] that actively avoids neutralization. That's the scientific challenge we face.
What's next?
On the vaccine side, we are currently performing, in collaboration with partners, two vaccine trials – HVTN702, which we talked about, and another one called 705. If either of those are highly successful, they would both require an additional phase 3 clinical trial before they could be licensed. This is an important but not final step. Then we would move into scale up to global vaccination. Those conversations have begun but they are not very far along and need additional attention.
What percent of people in the current trials would need to be protected to move on to phase 3?
Between 50 and 60 percent. That comes with this question of durability: how long does the vaccine last?
It also includes, can we simplify the vaccine regimen? The vaccines we're testing right now are multiple shots over a period of time. Can we get more like the polio or smallpox vaccine, a shot with a booster down the road?
We're dealing with sovereign nations. We're doing this in partnership, not as helicopter-type researchers.
If these current trials pan out, do you think kids in the developed world will end up getting an HIV vaccine one day? Or just people in-at risk areas?
That's a good question. I don't have an answer to that. In a perfect world, we'd get a vaccine like the HPV vaccine that was 100% effective and I think that's ultimately what we're going to strive for. That's where that second or third generation of vaccines that trigger broad neutralizing antibodies come in.
With any luck at all, globally, the combination of antiretroviral treatment, pre-exposure prophylaxis and other prevention and treatment strategies will lower the incidence rate where the HIV pandemic continues to wane, and we will then be able to either target the vaccine or roll it out in a way that is both cost effective and destigmatizing.
And also, what does the country want? We're dealing with sovereign nations. We're doing this in partnership, not as helicopter-type researchers.
How close do you think we are globally to eradicating HIV infections?
Eradication's a big word. It means no new infections. We are nowhere close to eradicating HIV. Whether or not we can continue to bend the curve on the epidemic and have less infections so that the total number of people continues to decline over time, I think we can achieve that if we had the political will. And that's not just the U.S. political will. That's the will of the world. We have the tools, albeit they're not perfect. But that's where a vaccine that is efficacious and simple to deliver could be the gamechanger.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
New Blood Test Can Detect Lymphoma Cells Before a Tumor Grows Back
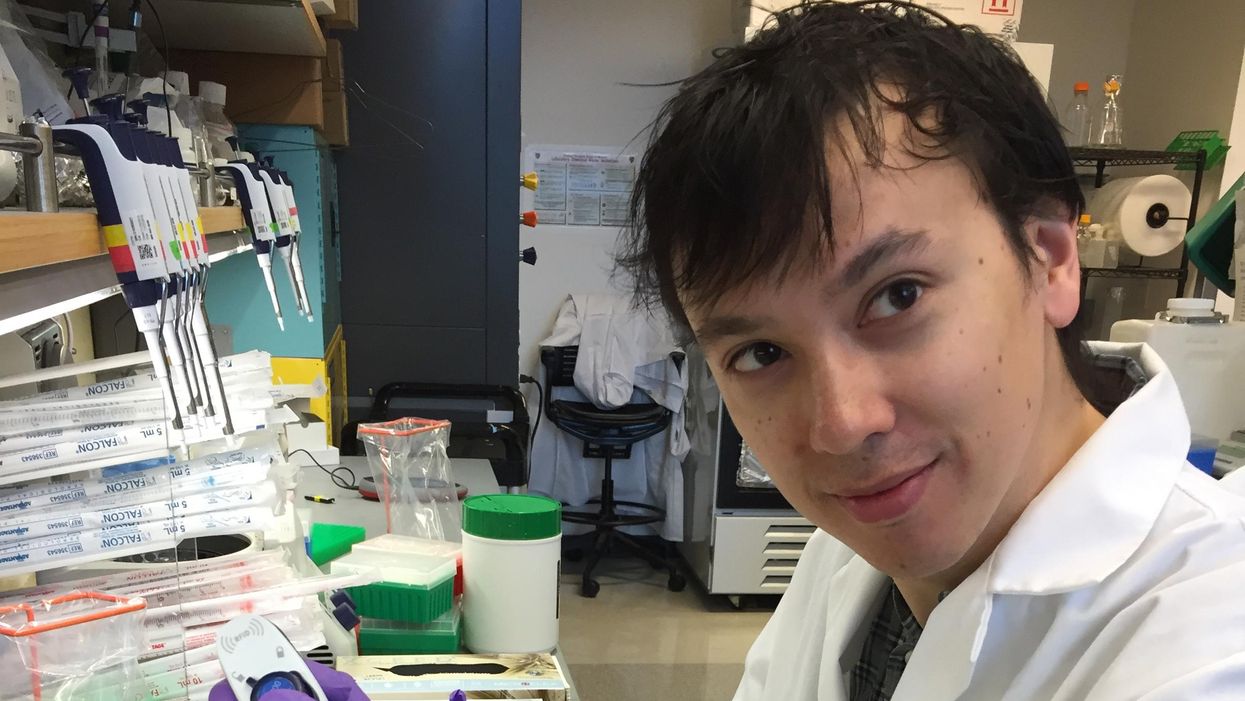
David Kurtz making DNA sequencing libraries in his lab.
When David M. Kurtz was doing his clinical fellowship at Stanford University Medical Center in 2009, specializing in lymphoma treatments, he found himself grappling with a question no one could answer. A typical regimen for these blood cancers prescribed six cycles of chemotherapy, but no one knew why. "The number seemed to be drawn out of a hat," Kurtz says. Some patients felt much better after just two doses, but had to endure the toxic effects of the entire course. For some elderly patients, the side effects of chemo are so harsh, they alone can kill. Others appeared to be cancer-free on the CT scans after the requisite six but then succumbed to it months later.
"Anecdotally, one patient decided to stop therapy after one dose because he felt it was so toxic that he opted for hospice instead," says Kurtz, now an oncologist at the center. "Five years down the road, he was alive and well. For him, just one dose was enough." Others would return for their one-year check up and find that their tumors grew back. Kurtz felt that while CT scans and MRIs were powerful tools, they weren't perfect ones. They couldn't tell him if there were any cancer cells left, stealthily waiting to germinate again. The scans only showed the tumor once it was back.
Blood cancers claim about 68,000 people a year, with a new diagnosis made about every three minutes, according to the Leukemia Research Foundation. For patients with B-cell lymphoma, which Kurtz focuses on, the survival chances are better than for some others. About 60 percent are cured, but the remaining 40 percent will relapse—possibly because they will have a negative CT scan, but still harbor malignant cells. "You can't see this on imaging," says Michael Green, who also treats blood cancers at University of Texas MD Anderson Medical Center.
The new blood test is sensitive enough to spot one cancerous perpetrator amongst one million other DNA molecules.
Kurtz wanted a better diagnostic tool, so he started working on a blood test that could capture the circulating tumor DNA or ctDNA. For that, he needed to identify the specific mutations typical for B-cell lymphomas. Working together with another fellow PhD student Jake Chabon, Kurtz finally zeroed-in on the tumor's genetic "appearance" in 2017—a pair of specific mutations sitting in close proximity to each other—a rare and telling sign. The human genome contains about 3 billion base pairs of nucleotides—molecules that compose genes—and in case of the B-cell lymphoma cells these two mutations were only a few base pairs apart. "That was the moment when the light bulb went on," Kurtz says.
The duo formed a company named Foresight Diagnostics, focusing on taking the blood test to the clinic. But knowing the tumor's mutational signature was only half the process. The other was fishing the tumor's DNA out of patients' bloodstream that contains millions of other DNA molecules, explains Chabon, now Foresight's CEO. It would be like looking for an escaped criminal in a large crowd. Kurtz and Chabon solved the problem by taking the tumor's "mug shot" first. Doctors would take the biopsy pre-treatment and sequence the tumor, as if taking the criminal's photo. After treatments, they would match the "mug shot" to all DNA molecules derived from the patient's blood sample to see if any molecular criminals managed to escape the chemo.
Foresight isn't the only company working on blood-based tumor detection tests, which are dubbed liquid biopsies—other companies such as Natera or ArcherDx developed their own. But in a recent study, the Foresight team showed that their method is significantly more sensitive in "fishing out" the cancer molecules than existing tests. Chabon says that this test can detect circulating tumor DNA in concentrations that are nearly 100 times lower than other methods. Put another way, it's sensitive enough to spot one cancerous perpetrator amongst one million other DNA molecules.
"It increases the sensitivity of detection and really catches most patients who are going to progress," says Green, the University of Texas oncologist who wasn't involved in the study, but is familiar with the method. It would also allow monitoring patients during treatment and making better-informed decisions about which therapy regimens would be most effective. "It's a minimally invasive test," Green says, and "it gives you a very high confidence about what's going on."
Having shown that the test works well, Kurtz and Chabon are planning a new trial in which oncologists would rely on their method to decide when to stop or continue chemo. They also aim to extend their test to detect other malignancies such as lung, breast or colorectal cancers. The latest genome sequencing technologies have sequenced and catalogued over 2,500 different tumor specimens and the Foresight team is analyzing this data, says Chabon, which gives the team the opportunity to create more molecular "mug shots."
The team hopes that that their blood cancer test will become available to patients within about five years, making doctors' job easier, and not only at the biological level. "When I tell patients, "good news, your cancer is in remission', they ask me, 'does it mean I'm cured?'" Kurtz says. "Right now I can't answer this question because I don't know—but I would like to." His company's test, he hopes, will enable him to reply with certainty. He'd very much like to have the power of that foresight.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
The First Mass-Produced Solar Car Is Coming Soon, Sparking Excitement and Uncertainty
Reporter Michaela Haas takes Aptera's Sol car out for a test drive in San Diego, Calif.
The white two-seater car that rolls down the street in the Sorrento Valley of San Diego looks like a futuristic batmobile, with its long aerodynamic tail and curved underbelly. Called 'Sol' (Spanish for "sun"), it runs solely on solar and could be the future of green cars. Its maker, the California startup Aptera, has announced the production of Sol, the world's first mass-produced solar vehicle, by the end of this year. Aptera co-founder Chris Anthony points to the sky as he says, "On this sunny California day, there is ample fuel. You never need to charge the car."
If you live in a sunny state like California or Florida, you might never need to plug in the streamlined Sol because the solar panels recharge while driving and parked. Its 60-mile range is more than the average commuter needs. For cloudy weather, battery packs can be recharged electronically for a range of up to 1,000 miles. The ultra-aerodynamic shape made of lightweight materials such as carbon, Kevlar, and hemp makes the Sol four times more energy-efficient than a Tesla, according to Aptera. "The material is seven times stronger than steel and even survives hail or an angry ex-girlfriend," Anthony promises.
Co-founder Steve Fambro opens the Sol's white doors that fly upwards like wings and I get inside for a test drive. Two dozen square solar panels, each the size of a large square coaster, on the roof, front, and tail power the car. The white interior is spartan; monitors have replaced mirrors and the dashboard. An engineer sits in the driver's seat, hits the pedal, and the low-drag two-seater zooms from 0 to 60 in 3.5 seconds.
It feels like sitting in a race car because the two-seater is so low to the ground but the car is built to go no faster than 100 or 110 mph. The finished car will weigh less than 1,800 pounds, about half of the smallest Tesla. The average car, by comparison, weighs more than double that. "We've built it primarily for energy efficiency," Steve Fambro says, explaining why the Sol has only three wheels. It's technically an "auto-cycle," a hybrid between a motorcycle and a car, but Aptera's designers are also working to design a four-seater.
There has never been a lack of grand visions for the future of the automobile, but until these solar cars actually hit the streets, nobody knows how the promises will hold up.
Transportation is currently the biggest source of greenhouse gases. Developing an efficient solar car that does not burden the grid has been the dream of innovators for decades. Every other year, dozens of innovators race their self-built solar cars 2,000 miles through the Australian desert.
More effective solar panels are finally making the dream mass-compatible, but just like other innovative car ideas, Aptera's vision has been plagued with money problems. Anthony and Fambro were part of the original crew that founded Aptera in 2006 and worked on the first prototype around the same time Tesla built its first roadster, but Aptera went bankrupt in 2011. Anthony and Fambro left a year before the bankruptcy and went on to start other companies. Among other projects, Fambro developed the first USDA organic vertical farm in the United Arab Emirates, and Anthony built a lithium battery company, before the two decided to buy Aptera back. Without a billionaire such as Elon Musk bankrolling the risky process of establishing a whole new car production system from scratch, the huge production costs are almost insurmountable.
But Aptera's founders believe they have found solutions for the entire production process as well as the car design. Most parts of the Sol's body can be made by 3D printers and assembled like a Lego kit. If this makes you think of a toy car, Anthony assures potential buyers that the car aced stress tests and claims it's safer than any vehicle on the market, "because the interior is shaped like an egg and if there is an impact, the pressure gets distributed equally." However, Aptera has yet to release crash test safety data so outside experts cannot evaluate their claims.
Instead of building a huge production facility, Anthony and Fambro envision "micro-factories," each less than 10,000 square feet, where a small crew can assemble cars on demand wherever the orders are highest, be it in California, Canada, or China.
If a part of the Sol breaks, Aptera promises to send replacement parts to any corner of the world within 24 hours, with instructions. So a mechanic in a rural corner in Arkansas or China who never worked on a solar car before simply needs to download the instructions and replace the broken part. At least that's the idea. "The material does not rust nor fatigue," Fambro promises. "You can pass the car onto your grandchildren. When more efficient solar panels hit the market, we simply replace them."
More than 11,000 potential buyers have already signed up; the cheapest model costs around $26,000 USD and Aptera expects the first cars to ship by the end of the year.
Two other solar carmakers are vying for the pole position in the race to be the first to market: The German startup Sono has also announced it will also produce its first solar car by the end of this year. The price tag for the basic model is also around $26,000, but its concept is very different. From the outside, the Sion looks like a conservative minivan for a family; only a closer look reveals that the dark exterior is made of solar panels. Sono, too, nearly went bankrupt a few years ago and was saved through a crowdfunding campaign by enthusiastic fans.
Meanwhile, Norwegian company Lightyear wants to produce a sleek solar-powered luxury sedan by the end of the year, but its price of around $180,000 makes it unaffordable for most buyers.
There has never been a lack of grand visions for the future of the automobile, but until these solar cars actually hit the streets, nobody knows how the promises will hold up. How often will the cars need to be repaired? What happens when snow and ice cover the solar panels? Also, you can't park the car in a garage if you need the sun to charge it.
Critics, including students at the Solar Car team at the University of Michigan, say that mounting solar panels on a moving vehicle will never yield the most efficient results compared to static panels. Also, they are quick to point out that no company has managed to overcome the production hurdles yet. Others in the field also wonder how well the solar panels will actually work.
"It's important to realize that the solar mileage claims by these companies are likely the theoretical best case scenario but in the real world, solar range will be significantly less when you factor in shading, parking in garages, and geographies with lower solar irradiance," says Evan Stumpges, the team coordinator for the American Solar Challenge, a competition in which enthusiasts build and race solar-powered cars. "The encouraging thing is that I have seen videos of real working prototypes for each of these vehicles which is a key accomplishment. That said, I believe the biggest hurdle these companies have yet to face is successfully ramping up to volume production and understanding what their profitability point will be for selling the vehicles once production has stabilized."
Professor Daniel M. Kammen, the founding director of the Renewable and Appropriate Energy Laboratory at the University of California, Berkeley, and one of the world's foremost experts on renewable energy, believes that the technical challenges have been solved, and that solar cars have real advantages over electric vehicles.
"This is the right time to be bullish. Cutting out the charging is a natural solution for long rides," he says. "These vehicles are essentially solar panels and batteries on wheels. These are now record low-cost and can be built from sustainable materials." Apart from Aptera's no-charge technology, he appreciates the move toward no-conflict materials. "Not only is the time ripe but the youth movement is pushing toward conflict-free material and reducing resource waste....A low-cost solar fleet could be really interesting in relieving burden on the grid, or you could easily imagine a city buying a bunch of them and connecting them with mass transit." While he has followed all three new solar companies with interest, he has already ordered an Aptera car for himself, "because it's American and it looks the most different."
After taking a spin in the Sol, it is startling to switch back into a regular four-seater. Rolling out of Aptera's parking lot onto the freeway next to all the oversized gas guzzlers that need to stop every couple of hundreds of miles to fill up, one can't help but think: We've just taken a trip into the future.