With Lab-Grown Chicken Nuggets, Dumplings, and Burgers, Futuristic Foods Aim to Seem Familiar

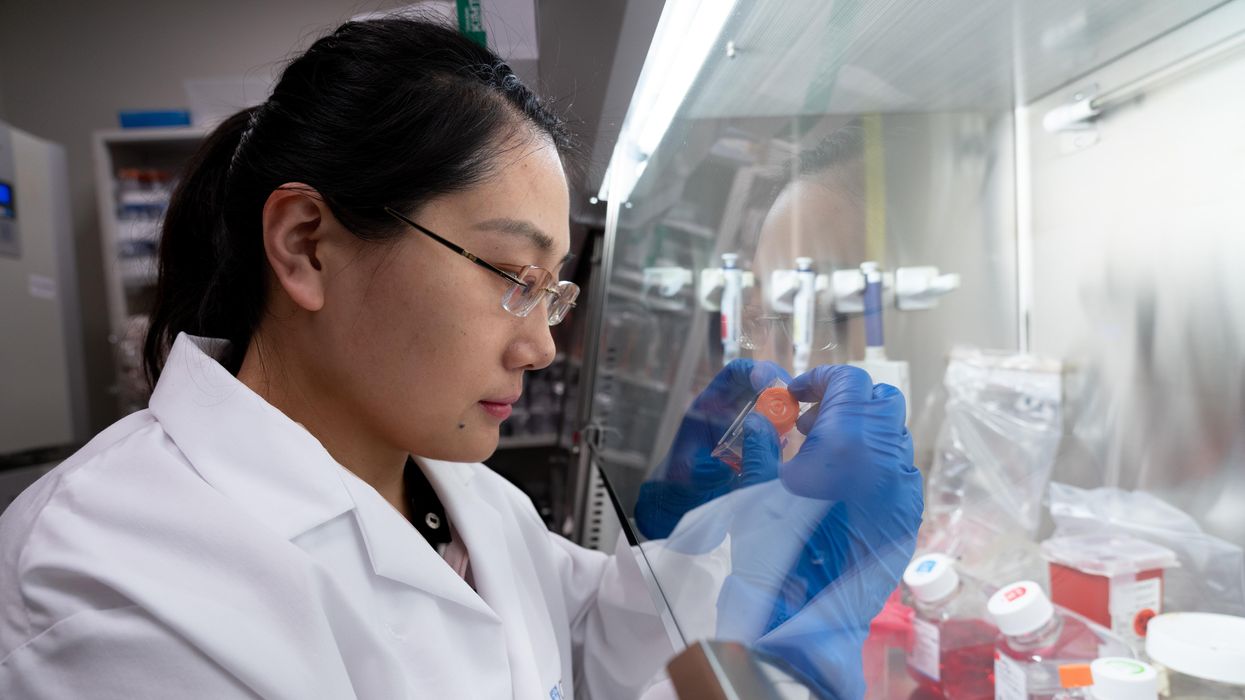
Shiok Meat's lab-grown "shrimp" dumplings, alongside a photo of the company's CTO, Ka Yi Ling, in a lab.
Sandhya Sriram is at the forefront of the expanding lab-grown meat industry in more ways than one.
"[Lab-grown meat] is kind of a brave new world for a lot of people, and food isn't something people like being brave about."
She's the CEO and co-founder of one of fewer than 30 companies that is even in this game in the first place. Her Singapore-based company, Shiok Meats, is the only one to pop up in Southeast Asia. And it's the only company in the world that's attempting to grow crustaceans in a lab, starting with shrimp. This spring, the company debuted a prototype of its shrimp, and completed a seed funding round of $4.6 million.
Yet despite all of these wins, Sriram's own mother won't try the company's shrimp. She's a staunch, lifelong vegetarian, adhering to a strict definition of what that means.
"[Lab-grown meat] is kind of a brave new world for a lot of people, and food isn't something people like being brave about. It's really a rather hard-wired thing," says Kate Krueger, the research director at New Harvest, a non-profit accelerator for cellular agriculture (the umbrella field that studies how to grow animal products in the lab, including meat, dairy, and eggs).
It's so hard-wired, in fact, that trends in food inform our species' origin story. In 2017, a group of paleoanthropologists caused an upset when they unearthed fossils in present day Morocco showing that our earliest human ancestors lived much further north and 100,000 years earlier than expected -- the remains date back 300,000 years. But the excavation not only included bones and tools, it also painted a clear picture of the prevailing menu at the time: The oldest humans were apparently chomping on tons of gazelle, as well as wildebeest and zebra when they could find them, plus the occasional seasonal ostrich egg.
These were people with a diet shaped by available resources, but also by the ability to cook in the first place. In his book Catching Fire: How Cooking Made Us Human, Harvard primatologist Richard Wrangam writes that the very thing that allowed for the evolution of Homo sapiens was the ability to transform raw ingredients into edible nutrients through cooking.
Today, our behavior and feelings around food are the product of local climate, crops, animal populations, and tools, but also religion, tradition, and superstition. So what happens when you add science to the mix? Turns out, we still trend toward the familiar. The innovations in lab-grown meat that are picking up the most steam are foods like burgers, not meat chips, and salmon, not salmon-cod-tilapia hybrids. It's not for lack of imagination, it's because the industry's practitioners know that a lifetime of food memories is a hard thing to contend with. So far, the nascent lab-grown meat industry is not so much disrupting as being shaped by the oldest culture we have.
Not a single piece of lab-grown meat is commercially available to consumers yet, and already so much ink has been spilled debating if it's really meat, if it's kosher, if it's vegetarian, if it's ethical, if it's sustainable. But whether or not the industry succeeds and sticks around is almost moot -- watching these conversations and innovations unfold serves as a mirror reflecting back who we are, what concerns us, and what we aspire to.
The More Things Change, the More They Stay the Same
The building blocks for making lab-grown meat right now are remarkably similar, no matter what type of animal protein a company is aiming to produce.
First, a small biopsy, about the size of a sesame seed, is taken from a single animal. Then, the muscle cells are isolated and added to a nutrient-dense culture in a bioreactor -- the same tool used to make beer -- where the cells can multiply, grow, and form muscle tissue. This tissue can then be mixed with additives like nutrients, seasonings, binders, and sometimes colors to form a food product. Whether a company is attempting to make chicken, fish, beef, shrimp, or any other animal protein in a lab, the basic steps remain similar. Cells from various animals do behave differently, though, and each company has its own proprietary techniques and tools. Some, for example, use fetal calf serum as their cell culture, while others, aiming for a more vegan approach, eschew it.
"New gadgets feel safest when they remind us of other objects that we already know."
According to Mark Post, who made the first lab-grown hamburger at Maastricht University in the Netherlands in 2013, the cells of just one cow can give way to 175 million four-ounce burgers. By today's available burger-making methods, you'd need to slaughter 440,000 cows for the same result. The projected difference in the purely material efficiency between the two systems is staggering. The environmental impact is hard to predict, though. Some companies claim that their lab-grown meat requires 99 percent less land and 96 percent less water than traditional farming methods -- and that rearing fewer cows, specifically, would reduce methane emissions -- but the energy cost of running a lab-grown-meat production facility at an industrial scale, especially as compared to small-scale, pasture-raised farming, could be problematic. It's difficult to truly measure any of this in a burgeoning industry.
At this point, growing something like an intact shrimp tail or a marbled steak in a lab is still a Holy Grail. It would require reproducing the complex musculo-skeletal and vascular structure of meat, not just the cellular basis, and no one's successfully done it yet. Until then, many companies working on lab-grown meat are perfecting mince. Each new company's demo of a prototype food feels distinctly regional, though: At the Disruption in Food and Sustainability Summit in March, Shiok (which is pronounced "shook," and is Singaporean slang for "very tasty and delicious") first shared a prototype of its shrimp as an ingredient in siu-mai, a dumpling of Chinese origin and a fixture at dim sum. JUST, a company based in the U.S., produced a demo chicken nugget.
As Jean Anthelme Brillat-Savarin, the 17th century founder of the gastronomic essay, famously said, "Show me what you eat, and I'll tell you who you are."
For many of these companies, the baseline animal protein they are trying to innovate also feels tied to place and culture: When meat comes from a bioreactor, not a farm, the world's largest exporter of seafood could be a landlocked region, and beef could be "reared" in a bayou, yet the handful of lab-grown fish companies, like Finless Foods and BlueNalu, hug the American coasts; VOW, based in Australia, started making lab-grown kangaroo meat in August; and of course the world's first lab-grown shrimp is in Singapore.
"In the U.S., shrimps are either seen in shrimp cocktail, shrimp sushi, and so on, but [in Singapore] we have everything from shrimp paste to shrimp oil," Sriram says. "It's used in noodles and rice, as flavoring in cup noodles, and in biscuits and crackers as well. It's seen in every form, shape, and size. It just made sense for us to go after a protein that was widely used."
It's tempting to assume that innovating on pillars of cultural significance might be easier if the focus were on a whole new kind of food to begin with, not your popular dim sum items or fast food offerings. But it's proving to be quite the opposite.
"That could have been one direction where [researchers] just said, 'Look, it's really hard to reproduce raw ground beef. Why don't we just make something completely new, like meat chips?'" says Mike Lee, co-founder and co-CEO of Alpha Food Labs, which works on food innovation more broadly. "While that strategy's interesting, I think we've got so many new things to explain to people that I don't know if you want to also explain this new format of food that you've never, ever seen before."
We've seen this same cautious approach to change before in other ways that relate to cooking. Perhaps the most obvious example is the kitchen range. As Bee Wilson writes in her book Consider the Fork: A History of How We Cook and Eat, in the 1880s, convincing ardent coal-range users to switch to newfangled gas was a hard sell. To win them over, inventor William Sugg designed a range that used gas, but aesthetically looked like the coal ones already in fashion at the time -- and which in some visual ways harkened even further back to the days of open-hearth cooking. Over time, gas range designs moved further away from those of the past, but the initial jump was only made possible through familiarity. There's a cleverness to meeting people where they are.
"New gadgets feel safest when they remind us of other objects that we already know," writes Wilson. "It is far harder to accept a technology that is entirely new."
Maybe someday we won't want anything other than meat chips, but not today.
Measuring Success
A 2018 Gallup poll shows that in the U.S., rates of true vegetarianism and veganism have been stagnant for as long as they've been measured. When the poll began in 1999, six percent of Americans were vegetarian, a number that remained steady until 2012, when the number dropped one point. As of 2018, it remained at five percent.
In 2012, when Gallup first measured the percentage of vegans, the rate was two percent. By 2018 it had gone up just one point, to three percent. Increasing awareness of animal welfare, health, and environmental concerns don't seem to be incentive enough to convince Americans, en masse, to completely slam the door on a food culture characterized in many ways by its emphasis on traditional meat consumption.
"A lot of consumers get over the ick factor when you tell them that most of the food that you're eating right now has entered the lab at some point."
Wilson writes that "experimenting with new foods has always been a dangerous business. In the wild, trying out some tempting new berries might lead to death. A lingering sense of this danger may make us risk-averse in the kitchen."
That might be one psychologically deep-seated reason that Americans are so resistant to ditch meat altogether. But a middle ground is emerging with a rise in flexitarianism, which aims to reduce reliance on traditional animal products. "Americans are eager to include alternatives to animal products in their diets, but are not willing to give up animal products completely," the same 2018 Gallup poll reported. This may represent the best opportunity for lab-grown meat to wedge itself into the culture.
Quantitatively predicting a population's willingness to try a lab-grown version of its favorite protein is proving a hard thing to measure, however, because it's still science fiction to a regular consumer. Measuring popular opinion of something that doesn't really exist yet is a dubious pastime.
In 2015, University of Wisconsin School of Public Health researchers Linnea Laestadius and Mark Caldwell conducted a study using online comments on articles about lab-grown meat to suss out public response to the food. The results showed a mostly negative attitude, but that was only two years into a field that is six years old today. Already public opinion may have shifted.
Shiok Meat's Sriram and her co-founder Ka Yi Ling have used online surveys to get a sense of the landscape, but they also take a more direct approach sometimes. Every time they give a public talk about their company and their shrimp, they poll their audience before and after the talk, using the question, "How many of you are willing to try, and pay, to eat lab-grown meat?"
They consistently find that the percentage of people willing to try goes up from 50 to 90 percent after hearing their talk, which includes information about the downsides of traditional shrimp farming (for one thing, many shrimp are raised in sewage, and peeled and deveined by slaves) and a bit of information about how lab-grown animal protein is being made now. I saw this pan out myself when Ling spoke at a New Harvest conference in Cambridge, Massachusetts in July.
"A lot of consumers get over the ick factor when you tell them that most of the food that you're eating right now has entered the lab at some point," Sriram says. "We're not going to grow our meat in the lab always. It's in the lab right now, because we're in R&D. Once we go into manufacturing ... it's going to be a food manufacturing facility, where a lot of food comes from."
The downside of the University of Wisconsin's and Shiok Meat's approach to capturing public opinion is that they each look at self-selecting groups: Online commenters are often fueled by a need to complain, and it's likely that anyone attending a talk by the co-founders of a lab-grown meat company already has some level of open-mindedness.
So Sriram says that she and Ling are also using another method to assess the landscape, and it's somewhere in the middle. They've been watching public responses to the closest available product to lab-grown meat that's on the market: Impossible Burger. As a 100 percent plant-based burger, it's not quite the same, but this bleedable, searable patty is still very much the product of science and laboratory work. Its remarkable similarity to beef is courtesy of yeast that have been genetically engineered to contain DNA from soy plant roots, which produce a protein called heme as they multiply. This heme is a plant-derived protein that can look and act like the heme found in animal muscle.
So far, the sciencey underpinnings of the burger don't seem to be turning people off. In just four years, it's already found its place within other American food icons. It's readily available everywhere from nationwide Burger Kings to Boston's Warren Tavern, which has been in operation since 1780, is one of the oldest pubs in America, and is even named after the man who sent Paul Revere on his midnight ride. Some people have already grown so attached to the Impossible Burger that they will actually walk out of a restaurant that's out of stock. Demand for the burger is outpacing production.
"Even though [Impossible] doesn't consider their product cellular agriculture, it's part of a spectrum of innovation," Krueger says. "There are novel proteins that you're not going to find in your average food, and there's some cool tech there. So to me, that does show a lot of willingness on people's part to think about trying something new."
The message for those working on animal-based lab-grown meat is clear: People will accept innovation on their favorite food if it tastes good enough and evokes the same emotional connection as the real deal.
"How people talk about lab-grown meat now, it's still a conversation about science, not about culture and emotion," Lee says. But he's confident that the conversation will start to shift in that direction if the companies doing this work can nail the flavor memory, above all.
And then proving how much power flavor lords over us, we quickly derail into a conversation about Doritos, which he calls "maniacally delicious." The chips carry no health value whatsoever and are a native product of food engineering and manufacturing — just watch how hard it is for Bon Appetit associate food editor Claire Saffitz to try and recreate them in the magazine's test kitchen — yet devotees remain unfazed and crunch on.
"It's funny because it shows you that people don't ask questions about how [some foods] are made, so why are they asking so many questions about how lab-grown meat is made?" Lee asks.
For all the hype around Impossible Burger, there are still controversies and hand-wringing around lab-grown meat. Some people are grossed out by the idea, some people are confused, and if you're the U.S. Cattlemen's Association (USCA), you're territorial. Last year, the group sent a petition to the USDA to "exclude products not derived directly from animals raised and slaughtered from the definition of 'beef' and meat.'"
"I think we are probably three or four big food safety scares away from everyone, especially younger generations, embracing lab-grown meat as like, 'Science is good; nature is dirty, and can kill you.'"
"I have this working hypothesis that if you look at the nation in 50-year spurts, we revolve back and forth between artisanal, all-natural food that's unadulterated and pure, and food that's empowered by science," Lee says. "Maybe we've only had one lap around the track on that, but I think we are probably three or four big food safety scares away from everyone, especially younger generations, embracing lab-grown meat as like, 'Science is good; nature is dirty, and can kill you.'"
Food culture goes beyond just the ingredients we know and love — it's also about how we interact with them, produce them, and expect them to taste and feel when we bite down. We accept a margin of difference among a fast food burger, a backyard burger from the grill, and a gourmet burger. Maybe someday we'll accept the difference between a burger created by killing a cow and a burger created by biopsying one.
Looking to the Future
Every time we engage with food, "we are enacting a ritual that binds us to the place we live and to those in our family, both living and dead," Wilson writes in Consider the Fork. "Such things are not easily shrugged off. Every time a new cooking technology has been introduced, however useful … it has been greeted in some quarters with hostility and protestations that the old ways were better and safer."
This is why it might be hard for a vegetarian mother to try her daughter's lab-grown shrimp, no matter how ethically it was produced or how awe-inspiring the invention is. Yet food cultures can and do change. "They're not these static things," says Benjamin Wurgaft, a historian whose book Meat Planet: Artificial Flesh and the Future of Food comes out this month. "The real tension seems to be between slow change and fast change."
In fact, the very definition of the word "meat" has never exclusively meant what the USCA wants it to mean. Before the 12th century, when it first appeared in Old English as "mete," it wasn't very specific at all and could be used to describe anything from "nourishment," to "food item," to "fodder," to "sustenance." By the 13th century it had been narrowed down to mean "flesh of warm-blooded animals killed and used as food." And yet the British mincemeat pie lives on as a sweet Christmas treat full of -- to the surprise of many non-Brits -- spiced, dried fruit. Since 1901, we've also used this word with ease as a general term for anything that's substantive -- as in, "the meat of the matter." There is room for yet more definitions to pile on.
"The conversation [about lab-ground meat] has changed remarkably in the last six years," Wurgaft says. "It has become a conversation about whether or not specific companies will bring a product to market, and that's a really different conversation than asking, 'Should we produce meat in the lab?'"
As part of the field research for his book, Wurgaft visited the Rijksmuseum Boerhaave, a Dutch museum that specializes in the history of science and medicine. It was 2015, and he was there to see an exhibit on the future of food. Just two years earlier, Mark Post had made that first lab-grown hamburger about a two-and-a-half hour drive south of the museum. When Wurgaft arrived, he found the novel invention, which Post had donated to the museum, already preserved and served up on a dinner plate, the whole outfit protected by plexiglass.
"They put this in the exhibit as if it were already part of the historical records, which to a historian looked really weird," Wurgaft says. "It looked like somebody taking the most recent supercomputer and putting it in a museum exhibit saying, 'This is the supercomputer that changed everything,' as if you were already 100 years in the future, looking back."
It seemed to symbolize an effort to codify a lab-grown hamburger as a matter of Dutch pride, perhaps someday occupying a place in people's hearts right next to the stroopwafel.
"Who's to say that we couldn't get a whole school of how to cook with lab-grown meat?"
Lee likes to imagine that part of the legacy of lab-grown meat, if it succeeds, will be to inspire entirely new fads in cooking -- a step beyond ones like the crab-filled avocado of the 1960s or the pesto of the 1980s in the U.S.
"[Lab-grown meat] is inherently going to be a different quality than anything we've done with an animal," he says. "Look at every cut [of meat] on the sphere today -- each requires a slightly different cooking method to optimize the flavor of that cut. Who's to say that we couldn't get a whole school of how to cook with lab-grown meat?"
At this point, most of us have no way of trying lab-grown meat. It remains exclusively available through sometimes gimmicky demos reserved for investors and the media. But Wurgaft says the stories we tell about this innovation, the articles we write, the films we make, and yes, even the museum exhibits we curate, all hold as much cultural significance as the product itself might someday.
A blood test may catch colorectal cancer before it's too late
A scientist works on a blood test in the Ajay Goel Lab, one of many labs that are developing blood tests to screen for different types of cancer.
Soon it may be possible to find different types of cancer earlier than ever through a simple blood test.
Among the many blood tests in development, researchers announced in July that they have developed one that may screen for early-onset colorectal cancer. The new potential screening tool, detailed in a study in the journal Gastroenterology, represents a major step in noninvasively and inexpensively detecting nonhereditary colorectal cancer at an earlier and more treatable stage.
In recent years, this type of cancer has been on the upswing in adults under age 50 and in those without a family history. In 2021, the American Cancer Society's revised guidelines began recommending that colorectal cancer screenings with colonoscopy begin at age 45. But that still wouldn’t catch many early-onset cases among people in their 20s and 30s, says Ajay Goel, professor and chair of molecular diagnostics and experimental therapeutics at City of Hope, a Los Angeles-based nonprofit cancer research and treatment center that developed the new blood test.
“These people will mostly be missed because they will never be screened for it,” Goel says. Overall, colorectal cancer is the fourth most common malignancy, according to the U.S. Centers for Disease Control and Prevention.
Goel is far from the only one working on this. Dozens of companies are in the process of developing blood tests to screen for different types of malignancies.
Some estimates indicate that between one-fourth and one-third of all newly diagnosed colorectal cancers are early-onset. These patients generally present with more aggressive and advanced disease at diagnosis compared to late-onset colorectal cancer detected in people 50 years or older.
To develop his test, Goel examined publicly available datasets and figured out that changes in novel microRNAs, or miRNAs, which regulate the expression of genes, occurred in people with early-onset colorectal cancer. He confirmed these biomarkers by looking for them in the blood of 149 patients who had the early-onset form of the disease. In particular, Goel and his team of researchers were able to pick out four miRNAs that serve as a telltale sign of this cancer when they’re found in combination with each other.
The blood test is being validated by following another group of patients with early-onset colorectal cancer. “We have filed for intellectual property on this invention and are currently seeking biotech/pharma partners to license and commercialize this invention,” Goel says.
He’s far from the only one working on this. Dozens of companies are in the process of developing blood tests to screen for different types of malignancies, says Timothy Rebbeck, a professor of cancer prevention at the Harvard T.H. Chan School of Public Health and the Dana-Farber Cancer Institute. But, he adds, “It’s still very early, and the technology still needs a lot of work before it will revolutionize early detection.”
The accuracy of the early detection blood tests for cancer isn’t yet where researchers would like it to be. To use these tests widely in people without cancer, a very high degree of precision is needed, says David VanderWeele, interim director of the OncoSET Molecular Tumor Board at Northwestern University’s Lurie Cancer Center in Chicago.
Otherwise, “you’re going to cause a lot of anxiety unnecessarily if people have false-positive tests,” VanderWeele says. So far, “these tests are better at finding cancer when there’s a higher burden of cancer present,” although the goal is to detect cancer at the earliest stages. Even so, “we are making progress,” he adds.
While early detection is known to improve outcomes, most cancers are detected too late, often after they metastasize and people develop symptoms. Only five cancer types have recommended standard screenings, none of which involve blood tests—breast, cervical, colorectal, lung (smokers considered at risk) and prostate cancers, says Trish Rowland, vice president of corporate communications at GRAIL, a biotechnology company in Menlo Park, Calif., which developed a multi-cancer early detection blood test.
These recommended screenings check for individual cancers rather than looking for any form of cancer someone may have. The devil lies in the fact that cancers without widespread screening recommendations represent the vast majority of cancer diagnoses and most cancer deaths.
GRAIL’s Galleri multi-cancer early detection test is designed to find more cancers at earlier stages by analyzing DNA shed into the bloodstream by cells—with as few false positives as possible, she says. The test is currently available by prescription only for those with an elevated risk of cancer. Consumers can request it from their healthcare or telemedicine provider. “Galleri can detect a shared cancer signal across more than 50 types of cancers through a simple blood draw,” Rowland says, adding that it can be integrated into annual health checks and routine blood work.
Cancer patients—even those with early and curable disease—often have tumor cells circulating in their blood. “These tumor cells act as a biomarker and can be used for cancer detection and diagnosis,” says Andrew Wang, a radiation oncologist and professor at the University of Texas Southwestern Medical Center in Dallas. “Our research goal is to be able to detect these tumor cells to help with cancer management.” Collaborating with Seungpyo Hong, the Milton J. Henrichs Chair and Professor at the University of Wisconsin-Madison School of Pharmacy, “we have developed a highly sensitive assay to capture these circulating tumor cells.”
Even if the quality of a blood test is superior, finding cancer early doesn’t always mean it’s absolutely best to treat it. For example, prostate cancer treatment’s potential side effects—the inability to control urine or have sex—may be worse than living with a slow-growing tumor that is unlikely to be fatal. “[The test] needs to tell me, am I going to die of that cancer? And, if I intervene, will I live longer?” says John Marshall, chief of hematology and oncology at Medstar Georgetown University Hospital in Washington, D.C.

Ajay Goel Lab
A blood test developed at the University of Texas MD Anderson Cancer Center in Houston helps predict who may benefit from lung cancer screening when it is combined with a risk model based on an individual’s smoking history, according to a study published in January in the Journal of Clinical Oncology. The personalized lung cancer risk assessment was more sensitive and specific than the 2021 and 2013 U.S. Preventive Services Task Force criteria.
The study involved participants from the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial with a minimum of a 10 pack-year smoking history, meaning they smoked 20 cigarettes per day for ten years. If implemented, the blood test plus model would have found 9.2 percent more lung cancer cases for screening and decreased referral to screening among non-cases by 13.7 percent compared to the 2021 task force criteria, according to Oncology Times.
The conventional type of screening for lung cancer is an annual low-dose CT scan, but only a small percentage of people who are eligible will actually get these scans, says Sam Hanash, professor of clinical cancer prevention and director of MD Anderson’s Center for Global Cancer Early Detection. Such screening is not readily available in most countries.
In methodically searching for blood-based biomarkers for lung cancer screening, MD Anderson researchers developed a simple test consisting of four proteins. These proteins circulating in the blood were at high levels in individuals who had lung cancer or later developed it, Hanash says.
“The interest in blood tests for cancer early detection has skyrocketed in the past few years,” he notes, “due in part to advances in technology and a better understanding of cancer causation, cancer drivers and molecular changes that occur with cancer development.”
However, at the present time, none of the blood tests being considered eliminate the need for screening of eligible subjects using established methods, such as colonoscopy for colorectal cancer. Yet, Hanash says, “they have the potential to complement these modalities.”
Study Shows “Living Drug” Can Provide a Lasting Cure for Cancer
A recent study by researchers at the University of Pennsylvania examined how CAR-T therapy helped Doug Olson beat a cancer death sentence for over a decade - and how it could work for more people.
Doug Olson was 49 when he was diagnosed with chronic lymphocytic leukemia, a blood cancer that strikes 21,000 Americans annually. Although the disease kills most patients within a decade, Olson’s case progressed more slowly, and courses of mild chemotherapy kept him healthy for 13 years. Then, when he was 62, the medication stopped working. The cancer had mutated, his doctor explained, becoming resistant to standard remedies. Harsher forms of chemo might buy him a few months, but their side effects would be debilitating. It was time to consider the treatment of last resort: a bone-marrow transplant.
Olson, a scientist who developed blood-testing instruments, knew the odds. There was only a 50 percent chance that a transplant would cure him. There was a 20 percent chance that the agonizing procedure—which involves destroying the patient’s marrow with chemo and radiation, then infusing his blood with donated stem cells—would kill him. If he survived, he would face the danger of graft-versus-host disease, in which the donor’s cells attack the recipient’s tissues. To prevent it, he would have to take immunosuppressant drugs, increasing the risk of infections. He could end up with pneumonia if one of his three grandchildren caught a sniffle. “I was being pushed into a corner,” Olson recalls, “with very little room to move.”
Soon afterward, however, his doctor revealed a possible escape route. He and some colleagues at the University of Pennsylvania’s Abramson Cancer Center were starting a clinical trial, he said, and Olson—still mostly symptom-free—might be a good candidate. The experimental treatment, known as CAR-T therapy, would use genetic engineering to turn his T lymphocytes (immune cells that guard against viruses and other pathogens) into a weapon against cancer.
In September 2010, technicians took some of Olson’s T cells to a laboratory, where they were programmed with new molecular marching orders and coaxed to multiply into an army of millions. When they were ready, a nurse inserted a catheter into his neck. At the turn of a valve, his soldiers returned home, ready to do battle.
“I felt like I’d won the lottery,” Olson says. But he was only the second person in the world to receive this “living drug,” as the University of Pennsylvania investigators called it. No one knew how long his remission would last.
Three weeks later, Olson was slammed with a 102-degree fever, nausea, and chills. The treatment had triggered two dangerous complications: cytokine release syndrome, in which immune chemicals inflame the patient’s tissues, and tumor lysis syndrome, in which toxins from dying cancer cells overwhelm the kidneys. But the crisis passed quickly, and the CAR-T cells fought on. A month after the infusion, the doctor delivered astounding news: “We can’t find any cancer in your body.”
“I felt like I’d won the lottery,” Olson says. But he was only the second person in the world to receive this “living drug,” as the University of Pennsylvania investigators called it. No one knew how long his remission would last.
An Unexpected Cure
In February 2022, the same cancer researchers reported a remarkable milestone: the trial’s first two patients had survived for more than a decade. Although Olson’s predecessor—a retired corrections officer named Bill Ludwig—died of COVID-19 complications in early 2021, both men had remained cancer-free. And the modified immune cells continued to patrol their territory, ready to kill suspected tumor cells the moment they arose.
“We can now conclude that CAR-T cells can actually cure patients with leukemia,” University of Pennsylvania immunologist Carl June, who spearheaded the development of the technique, told reporters. “We thought the cells would be gone in a month or two. The fact that they’ve survived 10 years is a major surprise.”
Even before the announcement, it was clear that CAR-T therapy could win a lasting reprieve for many patients with cancers that were once a death sentence. Since the Food and Drug Administration approved June’s version (marketed as Kymriah) in 2017, the agency has greenlighted five more such treatments for various types of leukemia, lymphoma, and myeloma. “Every single day, I take care of patients who would previously have been told they had no options,” says Rayne Rouce, a pediatric hematologist/oncologist at Texas Children’s Cancer Center. “Now we not only have a treatment option for those patients, but one that could potentially be the last therapy for their cancer that they’ll ever have to receive.”

Immunologist Carl June, middle, spearheaded development of the CAR-T therapy that gave patients Bill Ludwig, left, and Doug Olson, right, a lengthy reprieve on their terminal cancer diagnoses.
Penn Medicine
Yet the CAR-T approach doesn’t help everyone. So far, it has only shown success for blood cancers—and for those, the overall remission rate is 30 to 40 percent. “When it works, it works extraordinarily well,” says Olson’s former doctor, David Porter, director of Penn’s blood and bone marrow transplant program. “It’s important to know why it works, but it’s equally important to know why it doesn’t—and how we can fix that.”
The team’s study, published in the journal Nature, offers a wealth of data on what worked for these two patients. It may also hold clues for how to make the therapy effective for more people.
Building a Better T Cell
Carl June didn’t set out to cure cancer, but his serendipitous career path—and a personal tragedy—helped him achieve insights that had eluded other researchers. In 1971, hoping to avoid combat in Vietnam, he applied to the U.S. Naval Academy in Annapolis, Maryland. June showed a knack for biology, so the Navy sent him on to Baylor College of Medicine. He fell in love with immunology during a fellowship researching malaria vaccines in Switzerland. Later, the Navy deployed him to the Fred Hutchinson Cancer Research Center in Seattle to study bone marrow transplantation.
There, June became part of the first research team to learn how to culture T cells efficiently in a lab. After moving on to the National Naval Medical Center in the ’80s, he used that knowledge to combat the newly emerging AIDS epidemic. HIV, the virus that causes the disease, invades T cells and eventually destroys them. June and his post-doc Bruce Levine developed a method to restore patients’ depleted cell populations, using tiny magnetic beads to deliver growth-stimulating proteins. Infused into the body, the new T cells effectively boosted immune function.
In 1999, after leaving the Navy, June joined the University of Pennsylvania. His wife, who’d been diagnosed with ovarian cancer, died two years later, leaving three young children. “I had not known what it was like to be on the other side of the bed,” he recalls. Watching her suffer through grueling but futile chemotherapy, followed by an unsuccessful bone-marrow transplant, he resolved to focus on finding better cancer treatments. He started with leukemia—a family of diseases in which mutant white blood cells proliferate in the marrow.
Cancer is highly skilled at slipping through the immune system’s defenses. T cells, for example, detect pathogens by latching onto them with receptors designed to recognize foreign proteins. Leukemia cells evade detection, in part, by masquerading as normal white blood cells—that is, as part of the immune system itself.
June planned to use a viral vector no one had tried before: HIV.
To June, chimeric antigen receptor (CAR) T cells looked like a promising tool for unmasking and destroying the impostors. Developed in the early ’90s, these cells could be programmed to identify a target protein, and to kill any pathogen that displayed it. To do the programming, you spliced together snippets of DNA and inserted them into a disabled virus. Next, you removed some of the patient’s T cells and infected them with the virus, which genetically hijacked its new hosts—instructing them to find and slay the patient’s particular type of cancer cells. When the T cells multiplied, their descendants carried the new genetic code. You then infused those modified cells into the patient, where they went to war against their designated enemy.
Or that’s what happened in theory. Many scientists had tried to develop therapies using CAR-T cells, but none had succeeded. Although the technique worked in lab animals, the cells either died out or lost their potency in humans.
But June had the advantage of his years nurturing T cells for AIDS patients, as well as the technology he’d developed with Levine (who’d followed him to Penn with other team members). He also planned to use a viral vector no one had tried before: HIV, which had evolved to thrive in human T cells and could be altered to avoid causing disease. By the summer of 2010, he was ready to test CAR-T therapy against chronic lymphocytic leukemia (CLL), the most common form of the disease in adults.
Three patients signed up for the trial, including Doug Olson and Bill Ludwig. A portion of each man’s T cells were reprogrammed to detect a protein found only on B lymphocytes, the type of white blood cells affected by CLL. Their genetic instructions ordered them to destroy any cell carrying the protein, known as CD19, and to multiply whenever they encountered one. This meant the patients would forfeit all their B cells, not just cancerous ones—but regular injections of gamma globulins (a cocktail of antibodies) would make up for the loss.
After being infused with the CAR-T cells, all three men suffered high fevers and potentially life-threatening inflammation, but all pulled through without lasting damage. The third patient experienced a partial remission and survived for eight months. Olson and Ludwig were cured.
Learning What Works
Since those first infusions, researchers have developed reliable ways to prevent or treat the side effects of CAR-T therapy, greatly reducing its risks. They’ve also been experimenting with combination therapies—pairing CAR-T with chemo, cancer vaccines, and immunotherapy drugs called checkpoint inhibitors—to improve its success rate. But CAR-T cells are still ineffective for at least 60 percent of blood cancer patients. And they remain in the experimental stage for solid tumors (including pancreatic cancer, mesothelioma, and glioblastoma), whose greater complexity make them harder to attack.
The new Nature study offers clues that could fuel further advances. The Penn team “profiled these cells at a level where we can almost say, ‘These are the characteristics that a T cell would need to survive 10 years,’” says Rouce, the physician at Texas Children’s Cancer Center.
One surprising finding involves how CAR-T cells change in the body over time. At first, those that Olson and Ludwig received showed the hallmarks of “killer” T-cells (also known as CD8 cells)—highly active lymphocytes bent on exterminating every tumor cell in sight. After several months, however, the population shifted toward “helper” T-cells (or CD4s), which aid in forming long-term immune memory but are normally incapable of direct aggression. Over the years, the numbers swung back and forth, until only helper cells remained. Those cells showed markers suggesting they were too exhausted to function—but in the lab, they were able not only to recognize but to destroy cancer cells.
June and his team suspect that those tired-looking helper cells had enough oomph to kill off any B cells Olson and Ludwig made, keeping the pair’s cancers permanently at bay. If so, that could prompt new approaches to selecting cells for CAR-T therapy. Maybe starting with a mix of cell types—not only CD8s, but CD4s and other varieties—would work better than using CD8s alone. Or perhaps inducing changes in cell populations at different times would help.
Another potential avenue for improvement is starting with healthier cells. Evidence from this and other trials hints that patients whose T cells are more robust to begin with respond better when their cells are used in CAR-T therapy. The Penn team recently completed a clinical trial in which CLL patients were treated with ibrutinib—a drug that enhances T-cell function—before their CAR-T cells were manufactured. The response rate, says David Porter, was “very high,” with most patients remaining cancer-free a year after being infused with the souped-up cells.
Such approaches, he adds, are essential to achieving the next phase in CAR-T therapy: “Getting it to work not just in more people, but in everybody.”

Doug Olson enjoys nature - and having a future.
Penn Medicine
To grasp what that could mean, it helps to talk with Doug Olson, who’s now 75. In the years since his infusion, he has watched his four children forge careers, and his grandkids reach their teens. He has built a business and enjoyed the rewards of semi-retirement. He’s done volunteer and advocacy work for cancer patients, run half-marathons, sailed the Caribbean, and ridden his bike along the sun-dappled roads of Silicon Valley, his current home.
And in his spare moments, he has just sat there feeling grateful. “You don’t really appreciate the effect of having a lethal disease until it’s not there anymore,” he says. “The world looks different when you have a future.”
This article was first published on Leaps.org on March 24, 2022.