Your Community and COVID-19: How to Make Sense of the Numbers Where You Live
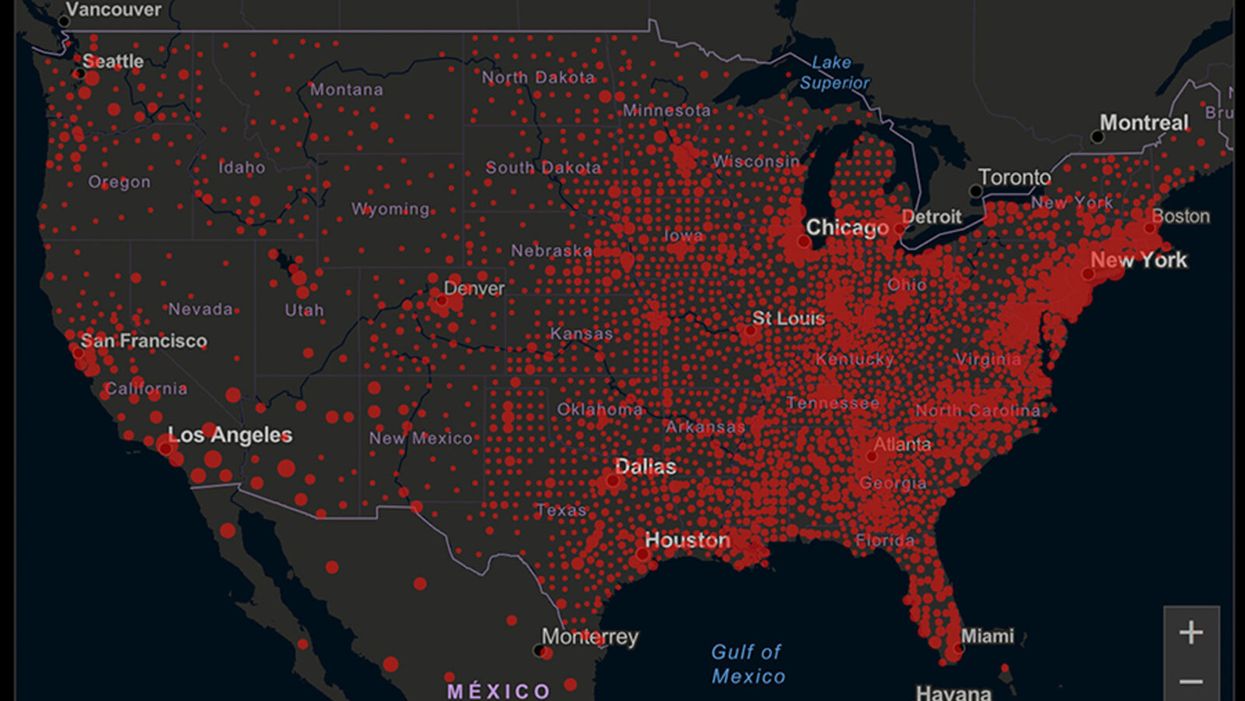
A map of cumulative known cases of COVID-19 in the U.S., as of June 12th, 2020.
Have you felt a bit like an armchair epidemiologist lately? Maybe you've been poring over coronavirus statistics on your county health department's website or on the pages of your local newspaper.
If the percentage of positive tests steadily stays under 8 percent, that's generally a good sign.
You're likely to find numbers and charts but little guidance about how to interpret them, let alone use them to make day-to-day decisions about pandemic safety precautions.
Enter the gurus. We asked several experts to provide guidance for laypeople about how to navigate the numbers. Here's a look at several common COVID-19 statistics along with tips about how to understand them.
Case Counts: Consider the Context
The number of confirmed COVID-19 cases in American counties is widely available. Local and state health departments should provide them online, or you can easily look them up at The New York Times' coronavirus database. However, you need to be cautious about interpreting them.
"Case counts are the obvious numbers to look at. But they're probably the hardest thing to sort out," said Dr. Jeff Martin, an epidemiologist at the University of California at San Francisco.
That's because case counts by themselves aren't a good window into how the coronavirus is affecting your community since they rely on testing. And testing itself varies widely from day to day and community to community.
"The more testing that's done, the more infections you'll pick up," explained Dr. F. Perry Wilson, a physician at Yale University. The numbers can also be thrown off when tests are limited to certain groups of people.
"If the tests are being mostly given to people with a high probability of having been infected -- for example, they have had symptoms or work in a high-risk setting -- then we expect lots of the tests to be positive. But that doesn't tell us what proportion of the general public is likely to have been infected," said Eleanor Murray, an epidemiologist at Boston University.
These Stats Are More Meaningful
According to Dr. Wilson, it's more useful to keep two other statistics in mind: the number of COVID tests that are being performed in your community and the percentage that turn up positive, showing that people have the disease. (These numbers may or may not be available locally. Check the websites of your community's health department and local news media outlets.)
If the number of people being tested is going up, but the percentage of positive tests is going down, Dr. Wilson said, that's a good sign. But if both numbers are going up – the number of people tested and the percentage of positive results – then "that's a sign that there are more infections burning in the community."
It's especially worrisome if the percentage of positive cases is growing compared to previous days or weeks, he said. According to him, that's a warning of a "high-risk situation."
Dr. George Rutherford, an epidemiologist at University of California at San Francisco, offered this tip: If the percentage of positive tests steadily stays under 8 percent, that's generally a good sign.
There's one more caveat about case counts. It takes an average of a week for someone to be infected with COVID-19, develop symptoms, and get tested, Dr. Rutherford said. It can take an additional several days for those test results to be reported to the county health department. This means that case numbers don't represent infections happening right now, but instead are a picture of the state of the pandemic more than a week ago.
Hospitalizations: Focus on Current Statistics
You should be able to find numbers about how many people in your community are currently hospitalized – or have been hospitalized – with diagnoses of COVID-19. But experts say these numbers aren't especially revealing unless you're able to see the number of new hospitalizations over time and track whether they're rising or falling. This number often isn't publicly available, however.
If new hospitalizations are increasing, "you may want to react by being more careful yourself."
And there's an important caveat: "The problem with hospitalizations is that they do lag," UC San Francisco's Dr. Martin said, since it takes time for someone to become ill enough to need to be hospitalized. "They tell you how much virus was being transmitted in your community 2 or 2.5 weeks ago."
Also, he said, people should be cautious about comparing new hospitalization rates between communities unless they're adjusted to account for the number of more-vulnerable older people.
Still, if new hospitalizations are increasing, he said, "you may want to react by being more careful yourself."
Deaths: They're an Even More Delayed Headline
Cable news networks obsessively track the number of coronavirus deaths nationwide, and death counts for every county in the country are available online. Local health departments and media websites may provide charts tracking the growth in deaths over time in your community.
But while death rates offer insight into the disease's horrific toll, they're not useful as an instant snapshot of the pandemic in your community because severely ill patients are typically sick for weeks. Instead, think of them as a delayed headline.
"These numbers don't tell you what's happening today. They tell you how much virus was being transmitted 3-4 weeks ago," Dr. Martin said.
'Reproduction Value': It May Be Revealing
You're not likely to find an available "reproduction value" for your community, but it is available for your state and may be useful.
A reproduction value, also known as R0 or R-naught, "tells us how many people on average we expect will be infected from a single case if we don't take any measures to intervene and if no one has been infected before," said Boston University's Murray.
As The New York Times explained, "R0 is messier than it might look. It is built on hard science, forensic investigation, complex mathematical models — and often a good deal of guesswork. It can vary radically from place to place and day to day, pushed up or down by local conditions and human behavior."
It may be impossible to find the R0 for your community. However, a website created by data specialists is providing updated estimates of a related number -- effective reproduction number, or Rt – for each state. (The R0 refers to how infectious the disease is in general and if precautions aren't taken. The Rt measures its infectiousness at a specific time – the "t" in Rt.) The site is at rt.live.
"The main thing to look at is whether the number is bigger than 1, meaning the outbreak is currently growing in your area, or smaller than 1, meaning the outbreak is currently decreasing in your area," Murray said. "It's also important to remember that this number depends on the prevention measures your community is taking. If the Rt is estimated to be 0.9 in your area and you are currently under lockdown, then to keep it below 1 you may need to remain under lockdown. Relaxing the lockdown could mean that Rt increases above 1 again."
"Whether they're on the upswing or downswing, no state is safe enough to ignore the precautions about mask wearing and social distancing."
Keep in mind that you can still become infected even if an outbreak in your community appears to be slowing. Low risk doesn't mean no risk.
Putting It All Together: Why the Numbers Matter
So you've reviewed COVID-19 statistics in your community. Now what?
Dr. Wilson suggests using the data to remind yourself that the coronavirus pandemic "is still out there. You need to take it seriously and continue precautions," he said. "Whether they're on the upswing or downswing, no state is safe enough to ignore the precautions about mask wearing and social distancing. 'My state is doing well, no one I know is sick, is it time to have a dinner party?' No."
He also recommends that laypeople avoid tracking COVID-19 statistics every day. "Check in once a week or twice a month to see how things are going," he suggested. "Don't stress too much. Just let it remind you to put that mask on before you get out of your car [and are around others]."
You won't score many glamor points for using a neti pot, but it could be a worthwhile asset in fighting Covid-19, according to the author's experience and recent research.
Twice a day, morning and night, I use a neti pot to send a warm saltwater solution coursing through one nostril and out the other to flush out debris and pathogens. I started many years ago because of sinus congestion and infections and it has greatly reduced those problems. Along with vaccination when it became available, it seems to have helped with protecting me from developing Covid-19 symptoms despite being of an age and weight that puts me squarely at risk.
Now that supposition of protection has been backed up with evidence from a solidly designed randomized clinical trial. It found that irrigating your sinuses twice a day with a simple saltwater solution can lead to an 8.5-fold reduction in hospitalization from Covid-19. The study is another example of recent research that points to easy and inexpensive ways to help protect yourself and help control the epidemic.
Amy Baxter, the physician researcher behind the study at Augusta University, Medical College of Georgia, began the study in 2020, before a vaccine or monoclonal antibodies became available to counter the virus. She wanted to be able to offer another line of defense for people with limited access to healthcare.
The nasal cavity is the front door that the SARS-CoV-2 virus typically uses to enter the body, latching on to the ACE2 receptors on cells lining those tissue compartments to establish infection. Once the virus replicates here, infection spreads into the lungs and often other parts of the body, including the brain and gut. Some studies have shown that a mouthwash could reduce the viral load, but any effect on disease progression was less clear. Baxter reasoned that reducing the amount of virus in the nose might give the immune system a better chance to react and control that growth before it got out of hand.
She decided to test this approach in patients who had just tested positive for Covid-19, were over 55 years of age, and often had other risk factors for developing serious symptoms. It was the quickest and easiest way to get results. A traditional prevention study would have required many more volunteers, taken a longer period of follow up, and cost money she did not have.
The trial enrolled 79 participants within 24 hours of testing positive for Covid-19, and they agreed to follow the regimen of twice daily nasal irrigation. They were followed for 28 days. One patient was hospitalized; a 1.27% rate compared with 11% in a national sample control group of similar age people who tested positive for Covid-19. Patients who strictly adhered to nasal irrigation had fewer, shorter and less severe symptoms than people in the study who missed some of their saline rinses.
Baxter initially made the results of her clinical trial available as a preprint in the summer of 2021 and was dismayed when many of the comments were from anti-vaxxers who argued this was a reason why you did not need to get vaccinated. That was not her intent.
There are several mechanisms that explain why warm saltwater is so effective. First and most obvious is the physical force of the water that sweeps away debris just as a rainstorm sends trash into a street gutter and down a storm drain. It also lubricates the cilia, small hair-like structures whose job it is to move detritus away from cells for expulsion. Cilia are rich in ACE2 receptors and keeping them moving makes it harder for the virus to latch on to the receptors.
It turns out the saline has a direct effect on the virus itself. SARS-CoV-2 becomes activated when an enzyme called furin snips off part of its molecular structure, which allows the virus to grab on to the ACE2 receptor, but saline inhibits this process. Once inside a cell the virus replicates best in a low salt environment, but nasal cells absorb salt from the irrigation, which further slows viral replication, says Baxter.
Finally, “salt improves the jellification of liquid, it makes better and stickier mucus so that you can get those virus out,” she explains, lamenting, “Nobody cares about snot. I do now.”
She initially made the results of her clinical trial available as a preprint in the summer of 2021 and was dismayed when many of the comments were from anti-vaxxers who argued this was a reason why you did not need to get vaccinated. That was not her intent. Two journals rejected the paper, and Baxter believes getting caught up in the polarizing politics of Covid-19 was an important part of the reason why. She says that editors “didn't want to be associated with something that was being used by anti-vaxxers.” She strongly supports vaccination but realizes that additional and alternative approaches also are needed.
Premeasured packets of saline are inexpensive and can be purchased at any drug store. They are safe to use several times a day. Say you’re vaccinated but were in a situation where you fear you might have been exposed to SARS-CoV-2; an extra irrigation will clear out your sinuses and may reduce the risk of that possible exposure.
Baxter plans no further study in this area. She is returning to her primary research focus, which is pain control and reducing opioid use, but she hopes that others will expand on what she had done.
Podcast: The Friday Five Weekly Roundup in Health Research
In this week's Friday Five: progress on a pill to prevent lung cancer. Plus, ancient wisdom about Neti pots could pay off against Covid, a breakthrough for precision medicine and obesity, the connection between taking a multivitamin pill and brain health - and much more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- A pill to prevent lung cancer?
- Ancient wisdom about Neti pots could pay off for Covid
- Breakthrough for precision medicine and obesity
- How to refreeze the north and south poles
- The connection between taking multivitamin pills and brain health