Your Prescription Is Ready for Download

A close up of a doctor pointing at a smart phone, heralding the new era of prescription digital therapeutics.
You may be familiar with Moore's Law, the prediction made by Intel co-founder Gordon Moore that computer chips would get faster and cheaper with each passing year. That's been borne out by the explosive growth of the tech industry, but you may not know that there is an inverse Moore's Law for drug development.
What if there were a way to apply the fast-moving, low-cost techniques of software development to drug discovery?
Eroom's Law—yes that's "Moore" spelled backward—is the observation that drug discovery has become slower and more expensive over time, despite technological improvements. And just like Moore's Law, it's been borne out by experience—from the 1950s to today, the number of drugs that can be developed per billion dollars in spending has steadily decreased, contributing to the continued growth of health care costs.
But what if there were a way to apply the fast-moving, low-cost techniques of software development to drug discovery? That's what a group of startups in the new field of digital therapeutics are promising. They develop apps that are used—either on their own or in conjunction with conventional drugs—to treat chronic disorders like addiction, diabetes and mental health that have so far resisted a pharmaceutical approach. Unlike the thousands of wellness and health apps that can be downloaded to your phone, digital therapeutics are developed and are meant to be used like drugs, complete with clinical trials, FDA approval and doctor prescriptions.
The field is hot—in 2017 global investment in digital therapeutics jumped to $11.5 billion, a fivefold increase from 2012, and major pharma companies like Novartis are developing their own digital products or partnering with startups. One such startup is the bicoastal Pear Therapeutics. Last month, Pear's reSET-O product became the first digital therapeutic to be approved for use by the millions of Americans who struggle with opioid use disorder, and the company has other products addressing addiction and mental illness in the pipeline.
I spoke with Dr. Corey McCann, Pear's CEO, about the company's efforts to meld software and medicine, designing clinical trials for an entirely new kind of treatment, and the future of digital therapeutics.
The interview has been edited and condensed for clarity and length.
"We're looking at conditions that currently can't be cured with drugs."
BRYAN WALSH: What makes a digital therapeutic different than a wellness app?
COREY MCCANN: What we do is develop therapeutics that are designed to be used under the auspices of a physician, just as a drug developed under good manufacturing would be. We do clinical studies for both safety and efficacy, and then they go through the development process you'd expect for a drug. We look at the commercial side, at the role of doctors. Everything we do is what would be done with a traditional medical product. It's a piece of software developed like a drug.
WALSH: What kind of conditions are you first aiming to treat with digital therapeutics?
MCCANN: We're looking at conditions that currently can't be cured with drugs. A good example is our reSET product, which is designed to treat addiction to alcohol, cannabis, stimulants, cocaine. There really aren't pharmaceutical products that are approved to treat people addicted to these substances. What we're doing is functional therapy, the standard of care for addiction treatment, but delivered via software. But we can also work with medication—our reSET-O product is a great example. It's for patients struggling with opioid addiction, and it's delivered in concert with the drug buprenorphine.
WALSH: Walk me through what the patient experience would be like for someone on a digital therapeutic like reSET.
MCCANN: Imagine you're a patient who has been diagnosed with cocaine addiction by a doctor. You would then receive a prescription for reSET during the same office visit. Instead of a pharmacy, the script is sent to the reSET Connect Patient Service Center, where you are onboarded and given an access code that is used to unlock the product after downloading it onto your device. The product has 60 different modules—each one requiring about a 10 to 15-minute interaction—all derived from a form of cognitive behavioral therapy called community reinforcement approach. The treatment takes place over 90 days.
"The patients receiving the digital therapeutic were more than twice as likely to remain abstinent as those receiving standard care."
Patients report their substance abuse, cravings and triggers, and they are also tested on core proficiencies through the therapy. Physicians have access to all of their data, which helps facilitate their one-on-one meetings. We know from regular urine tests how effective the treatment is.
WALSH: What kind of data did you find when you did clinical studies on reSET?
MCCANN: We had 399 patients in 10 centers taking part in a randomized clinical trial run by the National Institute on Drug Abuse. Every patient enrolled in the study had an active substance abuse disorder. The study was randomized so that patients either received the best current standard of care, which is three hours a week of face-to-face therapy, or they received the digital therapeutic. The primary endpoint was abstinence in weeks 9 to 12—if the patient had a single dirty urine screen in the last month, they counted as a failure.
In the end, the patients receiving the digital therapeutic were more than twice as likely to remain abstinent as those receiving standard care—40 percent versus 17 percent. Those receiving reSET were also much more likely to remain in treatment through the entire trial.
WALSH: Why start by focusing your first digital therapeutics on addiction?
MCCANN: We have tried to build a company that is poised to make a difference in medicine. If you look at addiction, there is little to nothing in the drug pipeline to address this. More than 30 million people in the U.S. suffer from addiction disorders, and not only is efficacy a concern, but so is access. Many patients aren't able to receive anything like the kind of face-to-face therapy our control group received. So we think digital therapeutics can make a difference there as well.
WALSH: reSET was the first digital therapeutic approved by the FDA to treat a specific disorder. What has the approval process been like?
MCCANN: It's been a learning process for all involved, including the FDA. Our philosophy is to work within the clinical trials structure, which has specific disease targets and endpoints, and develop quality software, and bring those two strands together to generate digital therapeutics. We now have two products that have been FDA-approved, and four more in development. The FDA is appropriately cautious about all of this, balancing the tradeoff between patient risk and medical value. As we see it, our company is half tech and half biotech, and we follow regulatory trials that are as rigorous as they would be with any drug company.
"This is a new space, but when you look back in 10 years there will be an entire industry of prescription digital therapeutics."
WALSH: How do you balance those two halves, the tech side and the biology side? Tech companies are known for iterating rapidly and cheaply, while pharma companies develop drugs slowly and expensively.
MCCANN: This is a new space, but when you look back in 10 years there will be an entire industry of prescription digital therapeutics. Right now for us we're combining the rigor of the pharmaceutical model with the speed and agility of a tech company. Our product takes longer to develop than an unverified health app, but less time and with less clinical risk than a new molecular entity. This is still a work in progress and not a day goes by where we don't notice the difference between those disciplines.
WALSH: Who's going to pay for these treatments? Insurers are traditionally slow to accept new innovations in the therapeutic space.
MCCANN: This is just like any drug launch. We need to show medical quality and value, and we need to get clinician demand. We want to focus on demonstrating as many scripts as we can in 2019. And we know we'll need to be persistent—we live in a world where payers will say no to anything three times before they say yes. Demonstrating value is how you get there.
WALSH: Is part of that value the possibility that digital therapeutics could be much cheaper than paying someone for multiple face-to-face therapy sessions?
MCCANN: I believe the cost model is very compelling here, especially when you can treat diseases that were not treatable before. That is something that creates medical value. Then you have the data aspect, which makes our product fundamentally different from a drug. We know everything about every patient that uses our product. We know engagement, we can push patient self-reports to clinicians. We can measure efficiency out in the real world, not just in a measured clinical trial. That is the holy grail in the pharma world—to understand compliance in practice.
WALSH: What's the future of digital therapeutics?
MCCANN: In 10 years, what we think of as digital medicine will just be medicine. This is something that will absolutely become standard of care. We are working on education to help partners and payers figure out where go from here, and to incorporate digital therapeutics into standard care. It will start in 2019 and 2020 with addiction medicine, and then in three to five years you'll see treatments designed to address disorders of the brain. And then past the decade horizon you'll see plenty of products that aim at every facet of medicine.
Scientists turn pee into power in Uganda
With conventional fuel cells as their model, researchers learned to use similar chemical reactions to make a fuel from microbes in pee.
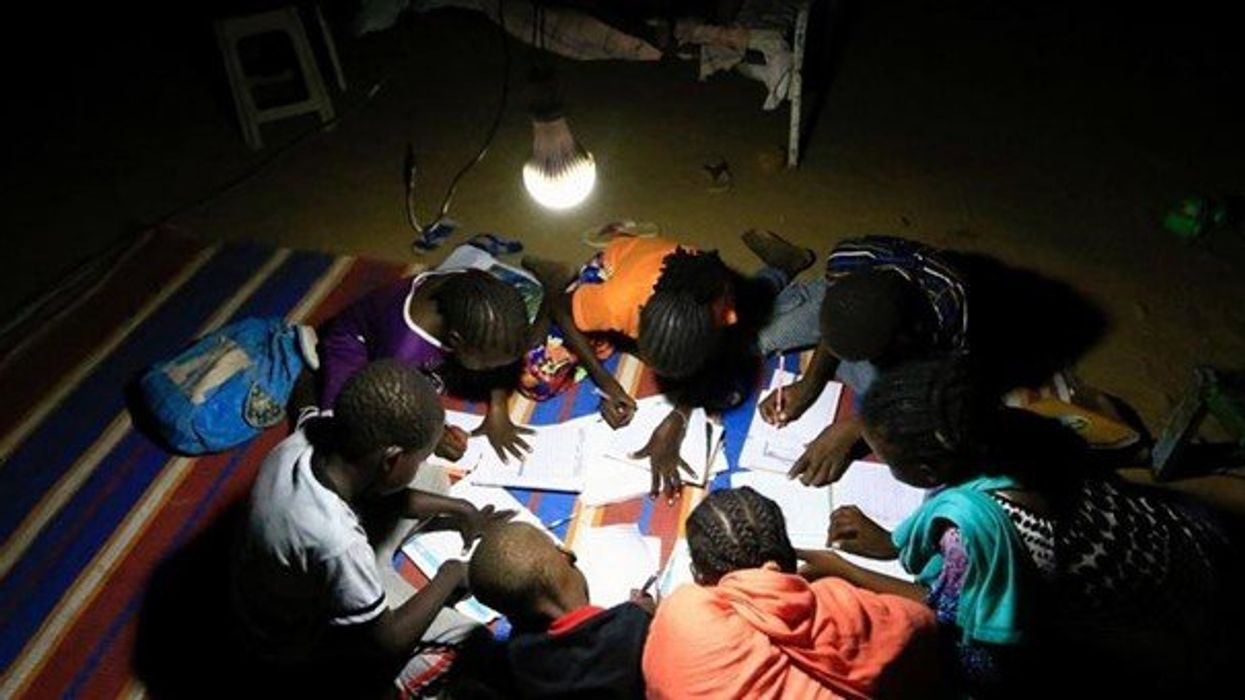
At the edge of a dirt road flanked by trees and green mountains outside the town of Kisoro, Uganda, sits the concrete building that houses Sesame Girls School, where girls aged 11 to 19 can live, learn and, at least for a while, safely use a toilet. In many developing regions, toileting at night is especially dangerous for children. Without electrical power for lighting, kids may fall into the deep pits of the latrines through broken or unsteady floorboards. Girls are sometimes assaulted by men who hide in the dark.
For the Sesame School girls, though, bright LED lights, connected to tiny gadgets, chased the fears away. They got to use new, clean toilets lit by the power of their own pee. Some girls even used the light provided by the latrines to study.
Urine, whether animal or human, is more than waste. It’s a cheap and abundant resource. Each day across the globe, 8.1 billion humans make 4 billion gallons of pee. Cows, pigs, deer, elephants and other animals add more. By spending money to get rid of it, we waste a renewable resource that can serve more than one purpose. Microorganisms that feed on nutrients in urine can be used in a microbial fuel cell that generates electricity – or "pee power," as the Sesame girls called it.
Plus, urine contains water, phosphorus, potassium and nitrogen, the key ingredients plants need to grow and survive. Human urine could replace about 25 percent of current nitrogen and phosphorous fertilizers worldwide and could save water for gardens and crops. The average U.S. resident flushes a toilet bowl containing only pee and paper about six to seven times a day, which adds up to about 3,500 gallons of water down per year. Plus cows in the U.S. produce 231 gallons of the stuff each year.
Pee power
A conventional fuel cell uses chemical reactions to produce energy, as electrons move from one electrode to another to power a lightbulb or phone. Ioannis Ieropoulos, a professor and chair of Environmental Engineering at the University of Southampton in England, realized the same type of reaction could be used to make a fuel from microbes in pee.
Bacterial species like Shewanella oneidensis and Pseudomonas aeruginosa can consume carbon and other nutrients in urine and pop out electrons as a result of their digestion. In a microbial fuel cell, one electrode is covered in microbes, immersed in urine and kept away from oxygen. Another electrode is in contact with oxygen. When the microbes feed on nutrients, they produce the electrons that flow through the circuit from one electrod to another to combine with oxygen on the other side. As long as the microbes have fresh pee to chomp on, electrons keep flowing. And after the microbes are done with the pee, it can be used as fertilizer.
These microbes are easily found in wastewater treatment plants, ponds, lakes, rivers or soil. Keeping them alive is the easy part, says Ieropoulos. Once the cells start producing stable power, his group sequences the microbes and keeps using them.
Like many promising technologies, scaling these devices for mass consumption won’t be easy, says Kevin Orner, a civil engineering professor at West Virginia University. But it’s moving in the right direction. Ieropoulos’s device has shrunk from the size of about three packs of cards to a large glue stick. It looks and works much like a AAA battery and produce about the same power. By itself, the device can barely power a light bulb, but when stacked together, they can do much more—just like photovoltaic cells in solar panels. His lab has produced 1760 fuel cells stacked together, and with manufacturing support, there’s no theoretical ceiling, he says.
Although pure urine produces the most power, Ieropoulos’s devices also work with the mixed liquids of the wastewater treatment plants, so they can be retrofit into urban wastewater utilities.
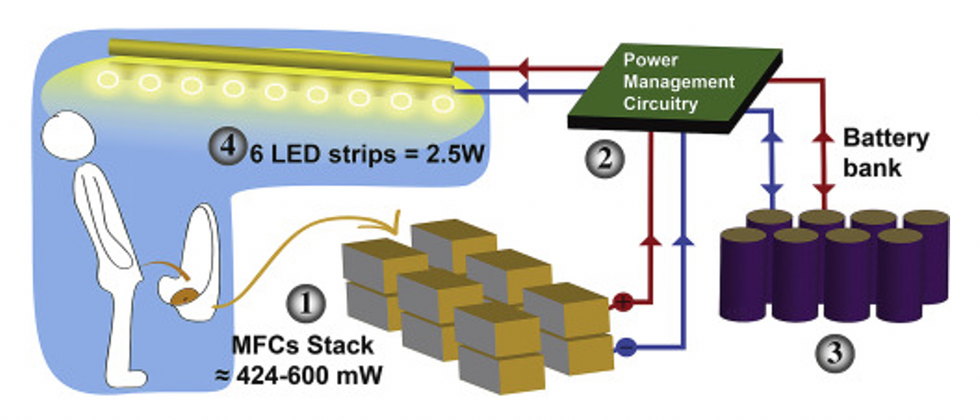
This image shows how the pee-powered system works. Pee feeds bacteria in the stack of fuel cells (1), which give off electrons (2) stored in parallel cylindrical cells (3). These cells are connected to a voltage regulator (4), which smooths out the electrical signal to ensure consistent power to the LED strips lighting the toilet.
Courtesy Ioannis Ieropoulos
Key to the long-term success of any urine reclamation effort, says Orner, is avoiding what he calls “parachute engineering”—when well-meaning scientists solve a problem with novel tech and then abandon it. “The way around that is to have either the need come from the community or to have an organization in a community that is committed to seeing a project operate and maintained,” he says.
Success with urine reclamation also depends on the economy. “If energy prices are low, it may not make sense to recover energy,” says Orner. “But right now, fertilizer prices worldwide are generally pretty high, so it may make sense to recover fertilizer and nutrients.” There are obstacles, too, such as few incentives for builders to incorporate urine recycling into new construction. And any hiccups like leaks or waste seepage will cost builders money and reputation. Right now, Orner says, the risks are just too high.
Despite the challenges, Ieropoulos envisions a future in which urine is passed through microbial fuel cells at wastewater treatment plants, retrofitted septic tanks, and building basements, and is then delivered to businesses to use as agricultural fertilizers. Although pure urine produces the most power, Ieropoulos’s devices also work with the mixed liquids of the wastewater treatment plants, so they can be retrofitted into urban wastewater utilities where they can make electricity from the effluent. And unlike solar cells, which are a common target of theft in some areas, nobody wants to steal a bunch of pee.
When Ieropoulos’s team returned to wrap up their pilot project 18 months later, the school’s director begged them to leave the fuel cells in place—because they made a major difference in students’ lives. “We replaced it with a substantial photovoltaic panel,” says Ieropoulos, They couldn’t leave the units forever, he explained, because of intellectual property reasons—their funders worried about theft of both the technology and the idea. But the photovoltaic replacement could be stolen, too, leaving the girls in the dark.
The story repeated itself at another school, in Nairobi, Kenya, as well as in an informal settlement in Durban, South Africa. Each time, Ieropoulos vowed to return. Though the pandemic has delayed his promise, he is resolute about continuing his work—it is a moral and legal obligation. “We've made a commitment to ourselves and to the pupils,” he says. “That's why we need to go back.”
Urine as fertilizer
Modern day industrial systems perpetuate the broken cycle of nutrients. When plants grow, they use up nutrients the soil. We eat the plans and excrete some of the nutrients we pass them into rivers and oceans. As a result, farmers must keep fertilizing the fields while our waste keeps fertilizing the waterways, where the algae, overfertilized with nitrogen, phosphorous and other nutrients grows out of control, sucking up oxygen that other marine species need to live. Few global communities remain untouched by the related challenges this broken chain create: insufficient clean water, food, and energy, and too much human and animal waste.
The Rich Earth Institute in Vermont runs a community-wide urine nutrient recovery program, which collects urine from homes and businesses, transports it for processing, and then supplies it as fertilizer to local farms.
One solution to this broken cycle is reclaiming urine and returning it back to the land. The Rich Earth Institute in Vermont is one of several organizations around the world working to divert and save urine for agricultural use. “The urine produced by an adult in one day contains enough fertilizer to grow all the wheat in one loaf of bread,” states their website.
Notably, while urine is not entirely sterile, it tends to harbor fewer pathogens than feces. That’s largely because urine has less organic matter and therefore less food for pathogens to feed on, but also because the urinary tract and the bladder have built-in antimicrobial defenses that kill many germs. In fact, the Rich Earth Institute says it’s safe to put your own urine onto crops grown for home consumption. Nonetheless, you’ll want to dilute it first because pee usually has too much nitrogen and can cause “fertilizer burn” if applied straight without dilution. Other projects to turn urine into fertilizer are in progress in Niger, South Africa, Kenya, Ethiopia, Sweden, Switzerland, The Netherlands, Australia, and France.
Eleven years ago, the Institute started a program that collects urine from homes and businesses, transports it for processing, and then supplies it as fertilizer to local farms. By 2021, the program included 180 donors producing over 12,000 gallons of urine each year. This urine is helping to fertilize hay fields at four partnering farms. Orner, the West Virginia professor, sees it as a success story. “They've shown how you can do this right--implementing it at a community level scale."
In this week's Friday Five, breathing this way may cut down on anxiety, a fasting regimen that could make you sick, this type of job makes men more virile, 3D printed hearts could save your life, and the role of metformin in preventing dementia.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Here are the promising studies covered in this week's Friday Five, featuring interviews with Dr. David Spiegel, associate chair of psychiatry and behavioral sciences at Stanford, and Dr. Filip Swirski, professor of medicine and cardiology at the Icahn School of Medicine at Mount Sinai.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five, featuring interviews with Dr. David Spiegel, associate chair of psychiatry and behavioral sciences at Stanford, and Dr. Filip Swirski, professor of medicine and cardiology at the Icahn School of Medicine at Mount Sinai.
- Breathing this way cuts down on anxiety*
- Could your fasting regimen make you sick?
- This type of job makes men more virile
- 3D printed hearts could save your life
- Yet another potential benefit of metformin
* This video with Dr. Andrew Huberman of Stanford shows exactly how to do the breathing practice.
This podcast originally aired on March 3, 2023.