Your Prescription Is Ready for Download

A close up of a doctor pointing at a smart phone, heralding the new era of prescription digital therapeutics.
You may be familiar with Moore's Law, the prediction made by Intel co-founder Gordon Moore that computer chips would get faster and cheaper with each passing year. That's been borne out by the explosive growth of the tech industry, but you may not know that there is an inverse Moore's Law for drug development.
What if there were a way to apply the fast-moving, low-cost techniques of software development to drug discovery?
Eroom's Law—yes that's "Moore" spelled backward—is the observation that drug discovery has become slower and more expensive over time, despite technological improvements. And just like Moore's Law, it's been borne out by experience—from the 1950s to today, the number of drugs that can be developed per billion dollars in spending has steadily decreased, contributing to the continued growth of health care costs.
But what if there were a way to apply the fast-moving, low-cost techniques of software development to drug discovery? That's what a group of startups in the new field of digital therapeutics are promising. They develop apps that are used—either on their own or in conjunction with conventional drugs—to treat chronic disorders like addiction, diabetes and mental health that have so far resisted a pharmaceutical approach. Unlike the thousands of wellness and health apps that can be downloaded to your phone, digital therapeutics are developed and are meant to be used like drugs, complete with clinical trials, FDA approval and doctor prescriptions.
The field is hot—in 2017 global investment in digital therapeutics jumped to $11.5 billion, a fivefold increase from 2012, and major pharma companies like Novartis are developing their own digital products or partnering with startups. One such startup is the bicoastal Pear Therapeutics. Last month, Pear's reSET-O product became the first digital therapeutic to be approved for use by the millions of Americans who struggle with opioid use disorder, and the company has other products addressing addiction and mental illness in the pipeline.
I spoke with Dr. Corey McCann, Pear's CEO, about the company's efforts to meld software and medicine, designing clinical trials for an entirely new kind of treatment, and the future of digital therapeutics.
The interview has been edited and condensed for clarity and length.
"We're looking at conditions that currently can't be cured with drugs."
BRYAN WALSH: What makes a digital therapeutic different than a wellness app?
COREY MCCANN: What we do is develop therapeutics that are designed to be used under the auspices of a physician, just as a drug developed under good manufacturing would be. We do clinical studies for both safety and efficacy, and then they go through the development process you'd expect for a drug. We look at the commercial side, at the role of doctors. Everything we do is what would be done with a traditional medical product. It's a piece of software developed like a drug.
WALSH: What kind of conditions are you first aiming to treat with digital therapeutics?
MCCANN: We're looking at conditions that currently can't be cured with drugs. A good example is our reSET product, which is designed to treat addiction to alcohol, cannabis, stimulants, cocaine. There really aren't pharmaceutical products that are approved to treat people addicted to these substances. What we're doing is functional therapy, the standard of care for addiction treatment, but delivered via software. But we can also work with medication—our reSET-O product is a great example. It's for patients struggling with opioid addiction, and it's delivered in concert with the drug buprenorphine.
WALSH: Walk me through what the patient experience would be like for someone on a digital therapeutic like reSET.
MCCANN: Imagine you're a patient who has been diagnosed with cocaine addiction by a doctor. You would then receive a prescription for reSET during the same office visit. Instead of a pharmacy, the script is sent to the reSET Connect Patient Service Center, where you are onboarded and given an access code that is used to unlock the product after downloading it onto your device. The product has 60 different modules—each one requiring about a 10 to 15-minute interaction—all derived from a form of cognitive behavioral therapy called community reinforcement approach. The treatment takes place over 90 days.
"The patients receiving the digital therapeutic were more than twice as likely to remain abstinent as those receiving standard care."
Patients report their substance abuse, cravings and triggers, and they are also tested on core proficiencies through the therapy. Physicians have access to all of their data, which helps facilitate their one-on-one meetings. We know from regular urine tests how effective the treatment is.
WALSH: What kind of data did you find when you did clinical studies on reSET?
MCCANN: We had 399 patients in 10 centers taking part in a randomized clinical trial run by the National Institute on Drug Abuse. Every patient enrolled in the study had an active substance abuse disorder. The study was randomized so that patients either received the best current standard of care, which is three hours a week of face-to-face therapy, or they received the digital therapeutic. The primary endpoint was abstinence in weeks 9 to 12—if the patient had a single dirty urine screen in the last month, they counted as a failure.
In the end, the patients receiving the digital therapeutic were more than twice as likely to remain abstinent as those receiving standard care—40 percent versus 17 percent. Those receiving reSET were also much more likely to remain in treatment through the entire trial.
WALSH: Why start by focusing your first digital therapeutics on addiction?
MCCANN: We have tried to build a company that is poised to make a difference in medicine. If you look at addiction, there is little to nothing in the drug pipeline to address this. More than 30 million people in the U.S. suffer from addiction disorders, and not only is efficacy a concern, but so is access. Many patients aren't able to receive anything like the kind of face-to-face therapy our control group received. So we think digital therapeutics can make a difference there as well.
WALSH: reSET was the first digital therapeutic approved by the FDA to treat a specific disorder. What has the approval process been like?
MCCANN: It's been a learning process for all involved, including the FDA. Our philosophy is to work within the clinical trials structure, which has specific disease targets and endpoints, and develop quality software, and bring those two strands together to generate digital therapeutics. We now have two products that have been FDA-approved, and four more in development. The FDA is appropriately cautious about all of this, balancing the tradeoff between patient risk and medical value. As we see it, our company is half tech and half biotech, and we follow regulatory trials that are as rigorous as they would be with any drug company.
"This is a new space, but when you look back in 10 years there will be an entire industry of prescription digital therapeutics."
WALSH: How do you balance those two halves, the tech side and the biology side? Tech companies are known for iterating rapidly and cheaply, while pharma companies develop drugs slowly and expensively.
MCCANN: This is a new space, but when you look back in 10 years there will be an entire industry of prescription digital therapeutics. Right now for us we're combining the rigor of the pharmaceutical model with the speed and agility of a tech company. Our product takes longer to develop than an unverified health app, but less time and with less clinical risk than a new molecular entity. This is still a work in progress and not a day goes by where we don't notice the difference between those disciplines.
WALSH: Who's going to pay for these treatments? Insurers are traditionally slow to accept new innovations in the therapeutic space.
MCCANN: This is just like any drug launch. We need to show medical quality and value, and we need to get clinician demand. We want to focus on demonstrating as many scripts as we can in 2019. And we know we'll need to be persistent—we live in a world where payers will say no to anything three times before they say yes. Demonstrating value is how you get there.
WALSH: Is part of that value the possibility that digital therapeutics could be much cheaper than paying someone for multiple face-to-face therapy sessions?
MCCANN: I believe the cost model is very compelling here, especially when you can treat diseases that were not treatable before. That is something that creates medical value. Then you have the data aspect, which makes our product fundamentally different from a drug. We know everything about every patient that uses our product. We know engagement, we can push patient self-reports to clinicians. We can measure efficiency out in the real world, not just in a measured clinical trial. That is the holy grail in the pharma world—to understand compliance in practice.
WALSH: What's the future of digital therapeutics?
MCCANN: In 10 years, what we think of as digital medicine will just be medicine. This is something that will absolutely become standard of care. We are working on education to help partners and payers figure out where go from here, and to incorporate digital therapeutics into standard care. It will start in 2019 and 2020 with addiction medicine, and then in three to five years you'll see treatments designed to address disorders of the brain. And then past the decade horizon you'll see plenty of products that aim at every facet of medicine.
A Rare Disease Just "Messed with the Wrong Mother." Now She's Fighting to Beat It Once and For All.
Amber Freed and Maxwell near their home in Denver, Colorado.
Amber Freed felt she was the happiest mother on earth when she gave birth to twins in March 2017. But that euphoric feeling began to fade over the next few months, as she realized her son wasn't making the same developmental milestones as his sister. "I had a perfect benchmark because they were twins, and I saw that Maxwell was floppy—he didn't have muscle tone and couldn't hold his neck up," she recalls. At first doctors placated her with statements that boys sometimes develop slower than girls, but the difference was just too drastic. At 10 month old, Maxwell had never reached to grab a toy. In fact, he had never even used his hands.
Thinking that perhaps Maxwell couldn't see well, Freed took him to an ophthalmologist who was the first to confirm her worst fears. He didn't find Maxwell to have vision problems, but he thought there was something wrong with the boy's brain. He had seen similar cases before and they always turned out to be rare disorders, and always fatal. "Start preparing yourself for your child not to live," he had said.
Getting the diagnosis took months of painful, invasive procedures, as well as fighting with the health insurance to get the genetic testing approved. Finally, in June 2018, doctors at the Children's Hospital Colorado gave the Freeds their son's diagnosis—a genetic mutation so rare it didn't even have a name, just a bunch of letters jammed together into a word SLC6A1—same as the name of the mutated gene. The mutation, with only 40 cases known worldwide at the time, caused developmental disabilities, movement and speech disorders, and a debilitating form of epilepsy.
The doctors didn't know much about the disorder, but they said that Maxwell would also regress in his development when he turned three or four. They couldn't tell how long he would live. "Hopefully you would become an expert and educate us about it," they said, as they gave Freed a five-page paper on the SLC6A1 and told her to start calling scientists if she wanted to help her son in any way. When she Googled the name, nothing came up. She felt horrified. "Our disease was too rare to care."
Freed's husband, a 6'2'' college football player broke down in sobs and she realized that if anything could be done to help Maxwell, she'd have be the one to do it. "I understood that I had to fight like a mother," she says. "And a determined mother can do a lot of things."

The Freed family.
Courtesy Amber Freed
She quit her job as an equity analyst the day of the diagnosis and became a full-time SLC6A1 citizen scientist looking for researchers studying mutations of this gene. In the wee hours of the morning, she called scientists in Europe. As the day progressed, she called researchers on the East Coast, followed by the West in the afternoon. In the evening, she switched to Asia and Australia. She asked them the same question. "Can you help explain my gene and how do we fix it?"
Scientists need money to do research, so Freed launched Milestones for Maxwell fundraising campaign, and a SLC6A1 Connect patient advocacy nonprofit, dedicated to improving the lives of children and families battling this rare condition. And then it became clear that the mutation wasn't as rare as it seemed. As other parents began to discover her nonprofit, the number of known cases rose from 40 to 100, and later to 400, Freed says. "The disease is only rare until it messes with the wrong mother."
It took one mother to find another to start looking into what's happening inside Maxwell's brain. Freed came across Jeanne Paz, a Gladstone Institutes researcher who studies epilepsy with particular interest in absence or silent seizures—those that don't manifest by convulsions, but rather make patients absently stare into space—and that's one type of seizures Maxwell has. "It's like a brief period of silence in the brain during which the person doesn't pay attention to what's happening, and as soon as they come out of the seizure they are back to life," Paz explains. "It's like a pause button on consciousness." She was working to understand the underlying biology.
To understand how seizures begin, spread and stop, Paz uses optogenetics in mice. From words "genetic" and "optikós," which means visible in Greek, the optogenetics technique involves two steps. First, scientists introduce a light-sensitive gene into a specific brain cell type—for example into excitatory neurons that release glutamate, a neurotransmitter, which activates other cells in the brain. Then they implant a very thin optical fiber into the brain area where they forged these light-sensitive neurons. As they shine the light through the optical fiber, researchers can make excitatory neurons to release glutamate—or instead tell them to stop being active and "shut up". The ability to control what these neurons of interest do, quite literally sheds light onto where seizures start, how they propagate and what cells are involved in stopping them.
"Let's say a seizure started and we shine the light that reduces the activity of specific neurons," Paz explains. "If that stops the seizure, we know that activating those cells was necessary to maintain the seizure." Likewise, shutting down their activity will make the seizure stop.
Freed reached out to Paz in 2019 and the two women had an instant connection. They were both passionate about brain and seizures research, even if for different reasons. Freed asked Paz if she would study her son's seizures and Paz agreed.
To do that, Paz needed mice that carried the SLC6A1 mutation, so Freed found a company in China that created them to specs. The company replaced a mouse SLC6A1 gene with a human mutated one and shipped them over to Paz's lab. "We call them Maxwell mice," Paz says, "and we are now implanting electrodes into them to see which brain regions generate seizures." That would help them understand what goes wrong and what brain cells are malfunctioning in the SLC6A1 mice—and help scientists better understand what might cause seizures in children.
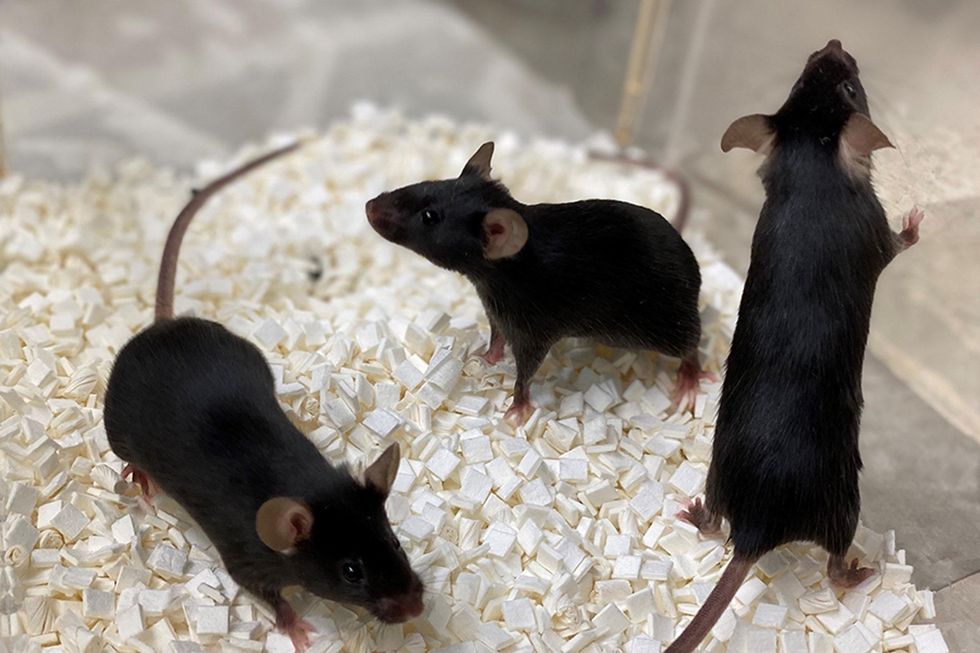
Bred to carry SLC6A1 mutation, these "Maxwell mice" will help better understand this debilitating genetic disease. (These mice are from Vanderbilt University, where researchers are also studying SLC6A1.)
Courtesy Amber Freed
This information—along with other research Amber is funding in other institutions—will inform the development of a novel genetic treatment, in which scientists would deploy a harmless virus to deliver a healthy, working copy of the SLC6A1 gene into the mice brains. They would likely deliver the therapeutic via a spinal tap infusion, and if it works and doesn't produce side effects in mice, the human trials will follow.
In the meantime, Freed is raising money to fund other research of various stop-gap measures. On April 22, 2021, she updated her Milestone for Maxwell page with a post that her nonprofit is funding yet another effort. It is a trial at Weill Cornell Medicine in New York City, in which doctors will use an already FDA-approved drug, which was recently repurposed for the SLC6A1 condition to treat epilepsy in these children. "It will buy us time," Freed says—while the gene therapy effort progresses.
Freed is determined to beat SLC6A1 before it beats down her family. She hopes to put an end to this disease—and similar genetic diseases—once and for all. Her goal is not only to have scientists create a remedy, but also to add the mutation to a newborn screening panel. That way, children born with this condition in the future would receive gene therapy before they even leave the hospital.
"I don't want there to be another Maxwell Freed," she says, "and that's why I am fighting like a mother." The gene therapy trial still might be a few years away, but the Weill Cornell one aims to launch very soon—possibly around Mother's Day. This is yet another milestone for Maxwell, another baby step forward—and the best gift a mother can get.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
On May 13th, scientific and medical experts will discuss and answer questions about the vaccine for those under 16.
This virtual event convened leading scientific and medical experts to address the public's questions and concerns about Covid-19 vaccines in kids and teens. Highlight video below.
DATE:
Thursday, May 13th, 2021
12:30 p.m. - 1:45 p.m. EDT
Dr. H. Dele Davies, M.D., MHCM

Senior Vice Chancellor for Academic Affairs and Dean for Graduate Studies at the University of Nebraska Medical (UNMC). He is an internationally recognized expert in pediatric infectious diseases and a leader in community health.
Dr. Emily Oster, Ph.D.

Professor of Economics at Brown University. She is a best-selling author and parenting guru who has pioneered a method of assessing school safety.
Dr. Tina Q. Tan, M.D.

Professor of Pediatrics at the Feinberg School of Medicine, Northwestern University. She has been involved in several vaccine survey studies that examine the awareness, acceptance, barriers and utilization of recommended preventative vaccines.
Dr. Inci Yildirim, M.D., Ph.D., M.Sc.
Associate Professor of Pediatrics (Infectious Disease); Medical Director, Transplant Infectious Diseases at Yale School of Medicine; Associate Professor of Global Health, Yale Institute for Global Health. She is an investigator for the multi-institutional COVID-19 Prevention Network's (CoVPN) Moderna mRNA-1273 clinical trial for children 6 months to 12 years of age.
About the Event Series
This event is the second of a four-part series co-hosted by Leaps.org, the Aspen Institute Science & Society Program, and the Sabin–Aspen Vaccine Science & Policy Group, with generous support from the Gordon and Betty Moore Foundation and the Howard Hughes Medical Institute.
:
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

