Scientists redesign bacteria to tackle the antibiotic resistance crisis
Probiotic bacteria can be engineered to fight antibiotic-resistant superbugs by releasing chemicals that kill them.
In 1945, almost two decades after Alexander Fleming discovered penicillin, he warned that as antibiotics use grows, they may lose their efficiency. He was prescient—the first case of penicillin resistance was reported two years later. Back then, not many people paid attention to Fleming’s warning. After all, the “golden era” of the antibiotics age had just began. By the 1950s, three new antibiotics derived from soil bacteria — streptomycin, chloramphenicol, and tetracycline — could cure infectious diseases like tuberculosis, cholera, meningitis and typhoid fever, among others.
Today, these antibiotics and many of their successors developed through the 1980s are gradually losing their effectiveness. The extensive overuse and misuse of antibiotics led to the rise of drug resistance. The livestock sector buys around 80 percent of all antibiotics sold in the U.S. every year. Farmers feed cows and chickens low doses of antibiotics to prevent infections and fatten up the animals, which eventually causes resistant bacterial strains to evolve. If manure from cattle is used on fields, the soil and vegetables can get contaminated with antibiotic-resistant bacteria. Another major factor is doctors overprescribing antibiotics to humans, particularly in low-income countries. Between 2000 to 2018, the global rates of human antibiotic consumption shot up by 46 percent.
In recent years, researchers have been exploring a promising avenue: the use of synthetic biology to engineer new bacteria that may work better than antibiotics. The need continues to grow, as a Lancet study linked antibiotic resistance to over 1.27 million deaths worldwide in 2019, surpassing HIV/AIDS and malaria. The western sub-Saharan Africa region had the highest death rate (27.3 people per 100,000).
Researchers warn that if nothing changes, by 2050, antibiotic resistance could kill 10 million people annually.
To make it worse, our remedy pipelines are drying up. Out of the 18 biggest pharmaceutical companies, 15 abandoned antibiotic development by 2013. According to the AMR Action Fund, venture capital has remained indifferent towards biotech start-ups developing new antibiotics. In 2019, at least two antibiotic start-ups filed for bankruptcy. As of December 2020, there were 43 new antibiotics in clinical development. But because they are based on previously known molecules, scientists say they are inadequate for treating multidrug-resistant bacteria. Researchers warn that if nothing changes, by 2050, antibiotic resistance could kill 10 million people annually.
The rise of synthetic biology
To circumvent this dire future, scientists have been working on alternative solutions using synthetic biology tools, meaning genetically modifying good bacteria to fight the bad ones.
From the time life evolved on earth around 3.8 billion years ago, bacteria have engaged in biological warfare. They constantly strategize new methods to combat each other by synthesizing toxic proteins that kill competition.
For example, Escherichia coli produces bacteriocins or toxins to kill other strains of E.coli that attempt to colonize the same habitat. Microbes like E.coli (which are not all pathogenic) are also naturally present in the human microbiome. The human microbiome harbors up to 100 trillion symbiotic microbial cells. The majority of them are beneficial organisms residing in the gut at different compositions.
The chemicals that these “good bacteria” produce do not pose any health risks to us, but can be toxic to other bacteria, particularly to human pathogens. For the last three decades, scientists have been manipulating bacteria’s biological warfare tactics to our collective advantage.
In the late 1990s, researchers drew inspiration from electrical and computing engineering principles that involve constructing digital circuits to control devices. In certain ways, every cell in living organisms works like a tiny computer. The cell receives messages in the form of biochemical molecules that cling on to its surface. Those messages get processed within the cells through a series of complex molecular interactions.
Synthetic biologists can harness these living cells’ information processing skills and use them to construct genetic circuits that perform specific instructions—for example, secrete a toxin that kills pathogenic bacteria. “Any synthetic genetic circuit is merely a piece of information that hangs around in the bacteria’s cytoplasm,” explains José Rubén Morones-Ramírez, a professor at the Autonomous University of Nuevo León, Mexico. Then the ribosome, which synthesizes proteins in the cell, processes that new information, making the compounds scientists want bacteria to make. “The genetic circuit remains separated from the living cell’s DNA,” Morones-Ramírez explains. When the engineered bacteria replicates, the genetic circuit doesn’t become part of its genome.
Highly intelligent by bacterial standards, some multidrug resistant V. cholerae strains can also “collaborate” with other intestinal bacterial species to gain advantage and take hold of the gut.
In 2000, Boston-based researchers constructed an E.coli with a genetic switch that toggled between turning genes on and off two. Later, they built some safety checks into their bacteria. “To prevent unintentional or deleterious consequences, in 2009, we built a safety switch in the engineered bacteria’s genetic circuit that gets triggered after it gets exposed to a pathogen," says James Collins, a professor of biological engineering at MIT and faculty member at Harvard University’s Wyss Institute. “After getting rid of the pathogen, the engineered bacteria is designed to switch off and leave the patient's body.”
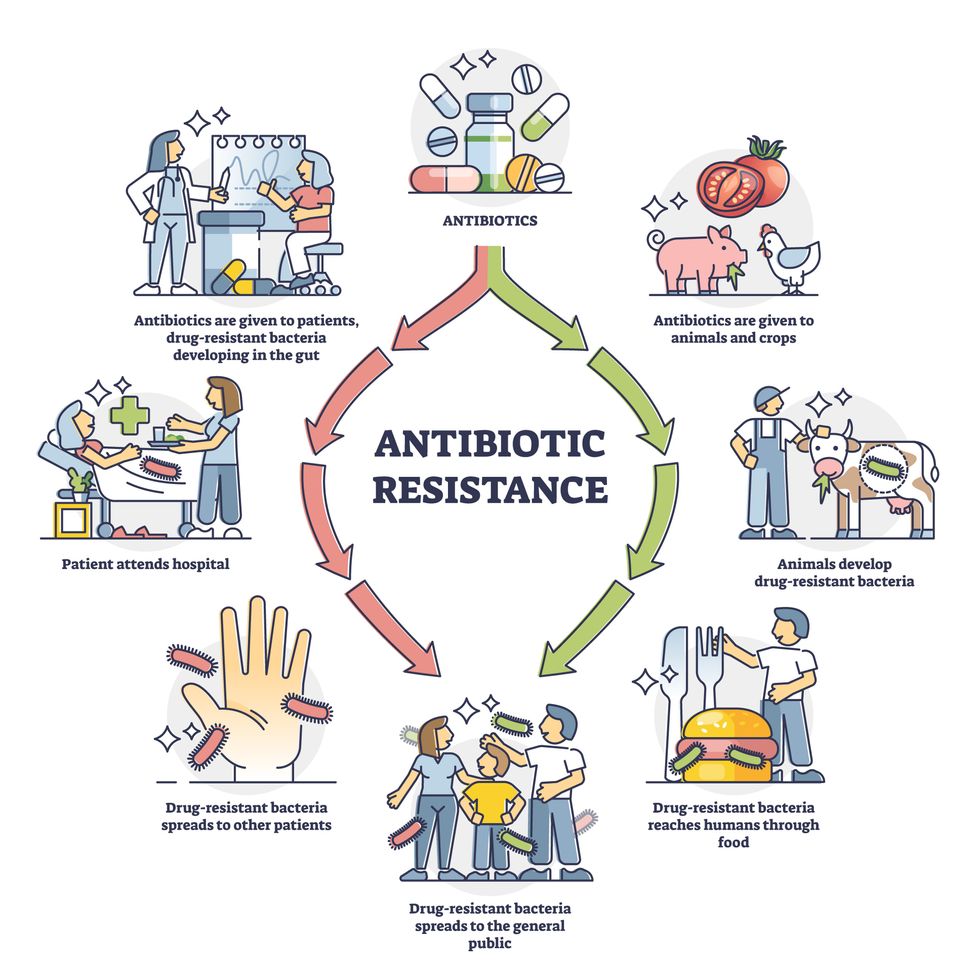
Overuse and misuse of antibiotics causes resistant strains to evolve
Adobe Stock
Seek and destroy
As the field of synthetic biology developed, scientists began using engineered bacteria to tackle superbugs. They first focused on Vibrio cholerae, which in the 19th and 20th century caused cholera pandemics in India, China, the Middle East, Europe, and Americas. Like many other bacteria, V. cholerae communicate with each other via quorum sensing, a process in which the microorganisms release different signaling molecules, to convey messages to its brethren. Highly intelligent by bacterial standards, some multidrug resistant V. cholerae strains can also “collaborate” with other intestinal bacterial species to gain advantage and take hold of the gut. When untreated, cholera has a mortality rate of 25 to 50 percent and outbreaks frequently occur in developing countries, especially during floods and droughts.
Sometimes, however, V. cholerae makes mistakes. In 2008, researchers at Cornell University observed that when quorum sensing V. cholerae accidentally released high concentrations of a signaling molecule called CAI-1, it had a counterproductive effect—the pathogen couldn’t colonize the gut.
So the group, led by John March, professor of biological and environmental engineering, developed a novel strategy to combat V. cholerae. They genetically engineered E.coli to eavesdrop on V. cholerae communication networks and equipped it with the ability to release the CAI-1 molecules. That interfered with V. cholerae progress. Two years later, the Cornell team showed that V. cholerae-infected mice treated with engineered E.coli had a 92 percent survival rate.
These findings inspired researchers to sic the good bacteria present in foods like yogurt and kimchi onto the drug-resistant ones.
Three years later in 2011, Singapore-based scientists engineered E.coli to detect and destroy Pseudomonas aeruginosa, an often drug-resistant pathogen that causes pneumonia, urinary tract infections, and sepsis. Once the genetically engineered E.coli found its target through its quorum sensing molecules, it then released a peptide, that could eradicate 99 percent of P. aeruginosa cells in a test-tube experiment. The team outlined their work in a Molecular Systems Biology study.
“At the time, we knew that we were entering new, uncharted territory,” says lead author Matthew Chang, an associate professor and synthetic biologist at the National University of Singapore and lead author of the study. “To date, we are still in the process of trying to understand how long these microbes stay in our bodies and how they might continue to evolve.”
More teams followed the same path. In a 2013 study, MIT researchers also genetically engineered E.coli to detect P. aeruginosa via the pathogen’s quorum-sensing molecules. It then destroyed the pathogen by secreting a lab-made toxin.
Probiotics that fight
A year later in 2014, a Nature study found that the abundance of Ruminococcus obeum, a probiotic bacteria naturally occurring in the human microbiome, interrupts and reduces V.cholerae’s colonization— by detecting the pathogen’s quorum sensing molecules. The natural accumulation of R. obeum in Bangladeshi adults helped them recover from cholera despite living in an area with frequent outbreaks.
The findings from 2008 to 2014 inspired Collins and his team to delve into how good bacteria present in foods like yogurt and kimchi can attack drug-resistant bacteria. In 2018, Collins and his team developed the engineered probiotic strategy. They tweaked a bacteria commonly found in yogurt called Lactococcus lactis to treat cholera.
Engineered bacteria can be trained to target pathogens when they are at their most vulnerable metabolic stage in the human gut. --José Rubén Morones-Ramírez.
More scientists followed with more experiments. So far, researchers have engineered various probiotic organisms to fight pathogenic bacteria like Staphylococcus aureus (leading cause of skin, tissue, bone, joint and blood infections) and Clostridium perfringens (which causes watery diarrhea) in test-tube and animal experiments. In 2020, Russian scientists engineered a probiotic called Pichia pastoris to produce an enzyme called lysostaphin that eradicated S. aureus in vitro. Another 2020 study from China used an engineered probiotic bacteria Lactobacilli casei as a vaccine to prevent C. perfringens infection in rabbits.
In a study last year, Ramírez’s group at the Autonomous University of Nuevo León, engineered E. coli to detect quorum-sensing molecules from Methicillin-resistant Staphylococcus aureus or MRSA, a notorious superbug. The E. coli then releases a bacteriocin that kills MRSA. “An antibiotic is just a molecule that is not intelligent,” says Ramírez. “On the other hand, engineered bacteria can be trained to target pathogens when they are at their most vulnerable metabolic stage in the human gut.”
Collins and Timothy Lu, an associate professor of biological engineering at MIT, found that engineered E. coli can help treat other conditions—such as phenylketonuria, a rare metabolic disorder, that causes the build-up of an amino acid phenylalanine. Their start-up Synlogic aims to commercialize the technology, and has completed a phase 2 clinical trial.
Circumventing the challenges
The bacteria-engineering technique is not without pitfalls. One major challenge is that beneficial gut bacteria produce their own quorum-sensing molecules that can be similar to those that pathogens secrete. If an engineered bacteria’s biosensor is not specific enough, it will be ineffective.
Another concern is whether engineered bacteria might mutate after entering the gut. “As with any technology, there are risks where bad actors could have the capability to engineer a microbe to act quite nastily,” says Collins of MIT. But Collins and Ramírez both insist that the chances of the engineered bacteria mutating on its own are virtually non-existent. “It is extremely unlikely for the engineered bacteria to mutate,” Ramírez says. “Coaxing a living cell to do anything on command is immensely challenging. Usually, the greater risk is that the engineered bacteria entirely lose its functionality.”
However, the biggest challenge is bringing the curative bacteria to consumers. Pharmaceutical companies aren’t interested in antibiotics or their alternatives because it’s less profitable than developing new medicines for non-infectious diseases. Unlike the more chronic conditions like diabetes or cancer that require long-term medications, infectious diseases are usually treated much quicker. Running clinical trials are expensive and antibiotic-alternatives aren’t lucrative enough.
“Unfortunately, new medications for antibiotic resistant infections have been pushed to the bottom of the field,” says Lu of MIT. “It's not because the technology does not work. This is more of a market issue. Because clinical trials cost hundreds of millions of dollars, the only solution is that governments will need to fund them.” Lu stresses that societies must lobby to change how the modern healthcare industry works. “The whole world needs better treatments for antibiotic resistance.”
Many children use makeup and body products such as glitter, face paint and lip gloss. Scientists are pointing to the harmful chemicals in some of these products, and advocates are looking to outlaw them.
When Erika Schreder’s 14-year-old daughter, who is Black, had her curly hair braided at a Seattle-area salon two or three times recently, the hairdresser applied a styling gel to seal the tresses in place.
Schreder and her daughter had been trying to avoid harmful chemicals, so they were shocked to later learn that this particular gel had the highest level of formaldehyde of any product tested by the Washington State Departments of Ecology and Health. In January 2023, the agencies released a report that uncovered high levels of formaldehyde in certain hair products, creams and lotions marketed to or used by people of color. When Schreder saw the report, she mentioned it to her daughter, who told her the name of the gel smoothed on her hair.
“It was really upsetting,” said Schreder, science director at Toxic-Free Future, a Seattle-based nonprofit environmental health research and advocacy organization. “Learning that this product used on my daughter’s hair contained cancer-causing formaldehyde made me even more committed to advocating for our state to ban toxic ingredients in cosmetics and personal care products.”
In 2013, Toxic-Free Future launched Mind the Store to challenge the nation’s largest retailers in adopting comprehensive policies that eliminate toxic chemicals in their personal care products and packaging, and develop safer alternatives.
Now, more efforts are underway to expose and mitigate the harm in cosmetics, hair care and other products that children apply on their faces, heads, nails and other body parts. Advocates hope to raise awareness among parents while prompting manufacturers and salon professionals to adopt safer alternatives.
A recent study by researchers at Columbia University Mailman School of Public Health and Earthjustice, a San Francisco-based nonprofit public interest environmental law organization, revealed that most children in the United States use makeup and body products that may contain carcinogens and other toxic chemicals. In January, the results were published in the International Journal of Environmental Research and Public Health. Based on more than 200 surveys, 70 percent of parents in the study reported that their children 12 or younger have used makeup and body products marketed to youth — for instance, glitter, face paint and lip gloss.
Childhood exposure to harmful makeup and body product ingredients can also be considered an environmental justice issue, as communities of color may be more likely to use these products.
“We are concerned about exposure to chemicals that may be found in cosmetics and body products, including those that are marketed toward children,” said the study’s senior author, Julie Herbstman, a professor and director of the Columbia Center for Children's Environmental Health. The goal of the survey was to try to understand how much kids are using cosmetic and body products and when, how and why they are using them.
“There is widespread use of children’s cosmetic and body products, and kids are using them principally to play,” Herbstman said. “That’s really quite different than how adults use cosmetic and body products.” Even with products that are specifically designed for children, “there’s no regulation that ensures that these products are safe for kids.” Also, she said, some children are using adult products — and they may do so in inadvisable ways, such as ingesting lipstick or applying it to other areas of the face.
Earlier research demonstrated that beauty and personal care products manufactured for children and adults frequently contain toxic chemicals, such as lead, asbestos, PFAS, phthalates and formaldehyde. Heavy metals and other toxic chemicals in children’s makeup and body products are particularly harmful to infants and youth, who are growing rapidly and whose bodies are less efficient at metabolizing these chemicals. Whether these chemicals are added intentionally or are present as contaminants, they have been associated with cancer, neurodevelopmental harm, and other serious and irreversible health effects, the Columbia University and Earthjustice researchers noted.
“Even when concentrations of individual chemicals are low in products, the potential for interactive effects from multiple toxicants is important to take into consideration,” the authors wrote in the journal article. “Allergic reactions, such as contact dermatitis, are some of the most frequently cited negative health outcomes associated with the use of cosmetics.”

Children’s small body side, rapid growth rate and immature immune systems are biologically more prone to the effects of toxicants than adults.
Adobe Stock
In addition to children’s rapid growth rate, the study also reported that their small body size, developing tissues and organs, and immature immune systems are biologically more prone to the effects of toxicants than adults. Meanwhile, the study noted, “childhood exposure to harmful makeup and body product ingredients can also be considered an environmental justice issue, as communities of color may be more likely to use these products.”
Although adults are the typical users of cosmetics, similar items are heavily marketed to youth with attention-grabbing features such as bright colors, animals and cartoon characters, according to the study. Beyond conventional makeup such as eyeshadow and lipstick, children may apply face paint, body glitter, nail polish, hair gel and fragrances. They also may frequent social media platforms on which these products are increasingly being promoted.
Products for both children and adults are currently regulated by the U.S. Food and Drug Administration under the Federal Food, Drug, and Cosmetic Act of 1938. Also, the Fair Packaging and Labeling Act of 1967 directs the Federal Trade Commission and the FDA “to issue regulations requiring that all ‘consumer commodities’ be labeled to disclose net contents, identity of commodity, and name and place of business of the product's manufacturer, packer, or distributor.” As the Columbia University and Earthjustice authors pointed out, though, “current safety regulations have been widely criticized as inadequate.”
The Personal Care Products Council in Washington, D.C., “fundamentally disagrees with the premise that companies put toxic chemicals in products produced for children,” industry spokeswoman Lisa Powers said in an email. Founded in 1894, the national trade association represents 600 member companies that manufacture, distribute and supply most personal care products marketed in the United States.
No category of consumer products is subject to less government oversight than cosmetics and other personal care products. -- Environmental Working Group.
“Science and safety are the cornerstones of our industry,” Powers stated. For more than a decade, she wrote, “the [Council] and our member companies worked diligently with a bipartisan group of congressional leaders and a diverse group of stakeholders to enhance the effectiveness of the FDA regulatory authority and to provide the safety reassurances that consumers expect and deserve.”
Powers added that the “industry employs and consults thousands of scientific and medical experts” who study the impacts of cosmetics and personal care products and the ingredients used in them. The Council also maintains a comprehensive database where consumers can look up science and safety information on the thousands of ingredients in sunscreens, toothpaste, shampoo, moisturizer, makeup, fragrances and other products.
However, the Environmental Working Group, which empowers consumers with breakthrough research to make informed choices about healthy living, believes the regulations are still not robust enough. “No category of consumer products is subject to less government oversight than cosmetics and other personal care products,” states the organization’s website. “Although many of the chemicals and contaminants in cosmetics and personal care products likely pose little risk, exposure to some has been linked to serious health problems, including cancer.”
The group, which operates the Skin Deep Database noted that “since 2009, 595 cosmetics manufacturers have reported using 88 chemicals, in more than 73,000 products, that have been linked to cancer, birth defects or reproductive harm.”
But change, for both adults and kids, is on the horizon. The Modernization of Cosmetics Regulation Act of 2022 significantly expanded the FDA’s authority to regulate cosmetics. In May 2023, Washington state adopted a law regulating cosmetics and personal care products. The Toxic-Free Cosmetics Act (HB 1047) bans chemicals in beauty and personal care products, such as PFAS, lead, mercury, phthalates and formaldehyde-releasing agents. These bans take effect in 2025, except for formaldehyde releasers, which have a phased-in approach starting in 2026.
Industry and advocates view this as a positive development. Powers, the spokesperson, praised “the long-awaited” Modernization Cosmetics Regulation Act of 2022, which she said, “advances product safety and innovation.” Jen Lee, chief impact officer at Beautycoutner, a company that sells personal care products, also welcomes the change. “We were proud to support the Washington Toxic-Free Cosmetics Act (HB 1047) by mobilizing our community of Brand Advocates who reside in Washington State,” Lee said. “Together, they made their voices heard by sending over 1,000 emails to their state legislators urging them to support and pass the bill.”
Laurie Valeriano, executive director of Toxic-Free Future, praised the upcoming Washington state law as “a huge win for public health and the environment that will have impacts that ripple across the nation.” She added that “companies won’t make special products for Washington state.” Instead, “they will reformulate and make products safer for everyone” — adults and children.
You shouldn’t have to be a toxicologist to shop for shampoo. -- Washington State Rep. Sharlett Mena
The new legislation will require Washington state agencies to assess the hazards of chemicals used in products that can impact vulnerable populations, while providing support for small businesses and independent cosmetologists to transition to safer products.

The Toxic-Free Future team lauds the Cosmetics Act, signed in May 2023.
Courtesy Toxic-Free Future
“When we go to a store, we assume the products on the shelf are safe, but this isn’t always true,” said Washington State Rep. Sharlett Mena, a Democrat serving in the 29th Legislative District (Tacoma), who sponsored the law. “I introduced this bill (HB 1047) because currently, the burden is on the consumer to navigate labels and find safe alternatives. You shouldn’t have to be a toxicologist to shop for shampoo.”
The new law aims to protect people of all ages, but especially youth. “Children are more susceptible to the impacts of toxic chemicals because their bodies are still developing,” Mena said. “Lead, for example, is significantly more hazardous to children than adults. Also, since children, unlike adults, tend to put things in their mouths all the time, they are more exposed to harmful chemicals in personal care and other products.”
Cosmetologists and hair professionals are taking notice. “Safety should be the practitioner’s number one concern” in using products on small children, said Anwar Saleem, a hair stylist, instructor and former salon owner in Washington, D.C., who is chairman of the D.C. Board of Barbering and Cosmetology and president of the National Interstate Council of State Boards of Cosmetology. “There are so many products on the market that it can be confusing.”
Hair products designed and labeled for children's use often have milder formulations, but “every child is unique, and what works for one may not work for another,” Saleem said. He recommends doing a patch test, in which the stylist or cosmetologist dabs the product on a small, inconspicuous area of the scalp or skin and waits anywhere from an hour to a day to check for irritation before continuing to serve the client. “Performing a patch test, observing children's reactions to a product and adequately adjusting are essential.”
Saleem seeks products that are free from harsh chemicals such as sulfates, phthalates and parabens, noting that these ingredients can be irritating and drying to the hair and scalp. If a child has sensitive skin or allergies, Saleem opts for hypoallergenic products.
We also need to ensure that less toxic alternatives are available and accessible to all consumers. It’s often under-resourced, low-income populations who suffer the burden of environmental exposures and do not have access or cannot afford these safer alternatives. -- Lesliam Quirós-Alcalá.
Lesliam Quirós-Alcalá, an assistant professor in the department of environmental health and engineering at the Johns Hopkins Bloomberg School of Public Health, said current regulatory loopholes on product labeling still allow manufacturers to advertise their cosmetics and personal care products as “gentle” and “natural.” However, she said, those terms may be misleading as they don’t necessarily mean the contents are less toxic or harmful to consumers.
“We also need to ensure that less toxic alternatives are available and accessible to all consumers,” Quirós-Alcalá said, “as often alternatives considered to be less toxic come with a hefty price tag.” As a result, “it’s often under-resourced, low-income populations who suffer the burden of environmental exposures and do not have access or cannot afford these safer alternatives.”
To advocate for safer alternatives, Quirós-Alcalá suggests that parents turn to consumer groups involved in publicizing the harms of personal care products. The Campaign for Safe Cosmetics is a program of Breast Cancer Prevention Partners, a national science-based advocacy organization aiming to prevent the disease by eliminating related environmental exposures. Other resources that inform users about unsafe ingredients include the mobile apps Clearya and Think Dirty.
“Children are not little adults, so it’s important to increase parent and consumer awareness to minimize their exposures to toxic chemicals in everyday products,” Quirós-Alcalá said. “Becoming smarter, more knowledgeable consumers is the first step to protecting your family from potentially harmful and toxic ingredients in consumer products.”
A startup aims to make medicines in space
A company is looking to improve medicines by making them in the nearly weightless environment of space.
Story by Big Think
On June 12, a SpaceX Falcon 9 rocket deployed 72 small satellites for customers — including the world’s first space factory.
The challenge: In 2019, pharma giant Merck revealed that an experiment on the International Space Station had shown how to make its blockbuster cancer drug Keytruda more stable. That meant it could now be administered via a shot rather than through an IV infusion.
The key to the discovery was the fact that particles behave differently when freed from the force of gravity — seeing how its drug crystalized in microgravity helped Merck figure out how to tweak its manufacturing process on Earth to produce the more stable version.
Microgravity research could potentially lead to many more discoveries like this one, or even the development of brand-new drugs, but ISS astronauts only have so much time for commercial experiments.
“There are many high-performance products that are only possible to make in zero-gravity, which is a manufacturing capability that cannot be replicated in any factory on Earth.”-- Will Bruey.
The only options for accessing microgravity (or free fall) outside of orbit, meanwhile, are parabolic airplane flights and drop towers, and those are only useful for experiments that require less than a minute in microgravity — Merck’s ISS experiment took 18 days.
The idea: In 2021, California startup Varda Space Industries announced its intention to build the world’s first space factory, to manufacture not only pharmaceuticals but other products that could benefit from being made in microgravity, such as semiconductors and fiber optic cables.
This factory would consist of a commercial satellite platform attached to two Varda-made modules. One module would contain equipment capable of autonomously manufacturing a product. The other would be a reentry capsule to bring the finished goods back to Earth.
“There are many high-performance products that are only possible to make in zero-gravity, which is a manufacturing capability that cannot be replicated in any factory on Earth,” said CEO Will Bruey, who’d previously developed and flown spacecraft for SpaceX.
“We have a team stacked with aerospace talent in the prime of their careers, focused on getting working hardware to orbit as quickly as possible,” he continued.
“[Pharmaceuticals] are the most valuable chemicals per unit mass. And they also have a large market on Earth.” -- Will Bruey, CEO of Varda Space.
What’s new? At the time, Varda said it planned to launch its first space factory in 2023, and, in what feels like a first for a space startup, it has actually hit that ambitious launch schedule.
“We have ACQUISITION OF SIGNAL,” the startup tweeted soon after the Falcon 9 launch on June 12. “The world’s first space factory’s solar panels have found the sun and it’s beginning to de-tumble.”
During the satellite’s first week in space, Varda will focus on testing its systems to make sure everything works as hoped. The second week will be dedicated to heating and cooling the old HIV-AIDS drug ritonavir repeatedly to study how its particles crystalize in microgravity.
After about a month in space, Varda will attempt to bring its first space factory back to Earth, sending it through the atmosphere at hypersonic speeds and then using a parachute system to safely land at the Department of Defense’s Utah Test and Training Range.
Looking ahead: Ultimately, Varda’s space factories could end up serving dual purposes as manufacturing facilities and hypersonic testbeds — the Air Force has already awarded the startup a contract to use its next reentry capsule to test hardware for hypersonic missiles.
But as for manufacturing other types of goods, Varda plans to stick with drugs for now.
“[Pharmaceuticals] are the most valuable chemicals per unit mass,” Bruey told CNN. “And they also have a large market on Earth.”
“You’re not going to see Varda do anything other than pharmaceuticals for the next minimum of six, seven years,” added Delian Asparouhov, Varda’s co-founder and president.
This article originally appeared on Big Think, home of the brightest minds and biggest ideas of all time.