As More People Crowdfund Medical Bills, Beware of Dubious Campaigns

Individuals seeking funding for experimental therapies may enroll in legitimate clinical trials -- or fall prey to snake oil.
Nearly a decade ago, Jamie Anderson hit his highest weight ever: 618 pounds. Depression drove him to eat and eat. He tried all kinds of diets, losing and regaining weight again and again. Then, four years ago, a friend nudged him to join a gym, and with a trainer's guidance, he embarked on a life-altering path.
Ethicists become particularly alarmed when medical crowdfunding appeals are for scientifically unfounded and potentially harmful interventions.
"The big catalyst for all of this is, I was diagnosed as a diabetic," says Anderson, a 46-year-old sales associate in the auto care department at Walmart. Within three years, he was down to 276 pounds but left with excess skin, which sagged from his belly to his mid-thighs.
Plastic surgery would cost $4,000 more than the sum his health insurance approved. That's when Anderson, who lives in Cabot, Arkansas, a suburb outside of Little Rock, turned to online crowdfunding to raise money. In a few months last year, current and former co-workers and friends of friends came up with that amount, covering the remaining expenses for the tummy tuck and overnight hospital stay.
The crowdfunding site that he used, CoFund Health, aimed to give his donors some peace of mind about where their money was going. Unlike GoFundMe and other platforms that don't restrict how donations are spent, Anderson's funds were loaded on a debit card that only worked at health care providers, so the donors "were assured that it was for medical bills only," he says.
CoFund Health was started in January 2019 in response to concerns about the legitimacy of many medical crowdfunding campaigns. As crowdfunding for health-related expenses has gained more traction on social media sites, with countless campaigns seeking to subsidize the high costs of care, it has given rise to some questionable transactions and legitimate ethical concerns.
Common examples of alleged fraud have involved misusing the donations for nonmedical purposes, feigning or embellishing the story of one's own unfortunate plight or that of another person, or impersonating someone else with an illness. Ethicists become particularly alarmed when medical crowdfunding appeals are for scientifically unfounded and potentially harmful interventions.
About 20 percent of American adults reported giving to a crowdfunding campaign for medical bills or treatments, according to a survey by AmeriSpeak Spotlight on Health from NORC, formerly called the National Opinion Research Center, a non-partisan research institution at the University of Chicago. The self-funded poll, conducted in November 2019, included 1,020 interviews with a representative sample of U.S. households. Researchers cited a 2019 City University of New York-Harvard study, which noted that medical bills are the most common basis for declaring personal bankruptcy.
Some experts contend that crowdfunding platforms should serve as gatekeepers in prohibiting campaigns for unproven treatments. Facing a dire diagnosis, individuals may go out on a limb to try anything and everything to prolong and improve the quality of their lives.
They may enroll in well-designed clinical trials, or they could fall prey "to snake oil being sold by people out there just making a buck," says Jeremy Snyder, a health sciences professor at Simon Fraser University in British Columbia, Canada, and the lead author of a December 2019 article in The Hastings Report about crowdfunding for dubious treatments.
For instance, crowdfunding campaigns have sought donations for homeopathic healing for cancer, unapproved stem cell therapy for central nervous system injury, and extended antibiotic use for chronic Lyme disease, according to an October 2018 report in the Journal of the American Medical Association.
Ford Vox, the lead author and an Atlanta-based physician specializing in brain injury, maintains that a repository should exist to monitor the outcomes of experimental treatments. "At the very least, there ought to be some tracking of what happens to the people the funds are being raised for," he says. "It would be great for an independent organization to do so."
"Even if it appears like a good cause, consumers should still do some research before donating to a crowdfunding campaign."
The Federal Trade Commission, the national consumer watchdog, cautions online that "it might be impossible for you to know if the cause is real and if the money actually gets to the intended recipient." Another caveat: Donors can't deduct contributions to individuals on tax returns.
"Even if it appears like a good cause, consumers should still do some research before donating to a crowdfunding campaign," says Malini Mithal, associate director of financial practices at the FTC. "Don't assume all medical treatments are tested and safe."
Before making any donation, it would be wise to check whether a crowdfunding site offers some sort of guarantee if a campaign ends up being fraudulent, says Kristin Judge, chief executive and founder of the Cybercrime Support Network, a Michigan-based nonprofit that serves victims before, during, and after an incident. They should know how the campaign organizer is related to the intended recipient and note whether any direct family members and friends have given funds and left supportive comments.
Donating to vetted charities offers more assurance than crowdfunding that the money will be channeled toward helping someone in need, says Daniel Billingsley, vice president of external affairs for the Oklahoma Center of Nonprofits. "Otherwise, you could be putting money into all sorts of scams." There is "zero accountability" for the crowdfunding site or the recipient to provide proof that the dollars were indeed funneled into health-related expenses.
Even if donors may have limited recourse against scammers, the "platforms have an ethical obligation to protect the people using their site from fraud," says Bryanna Moore, a postdoctoral fellow at Baylor College of Medicine's Center for Medical Ethics and Health Policy. "It's easy to take advantage of people who want to be charitable."
There are "different layers of deception" on a broad spectrum of fraud, ranging from "outright lying for a self-serving reason" to publicizing an imaginary illness to collect money genuinely needed for basic living expenses. With medical campaigns being a top category among crowdfunding appeals, it's "a lot of money that's exchanging hands," Moore says.
The advent of crowdfunding "reveals and, in some ways, reinforces a health care system that is totally broken," says Jessica Pierce, a faculty affiliate in the Center for Bioethics and Humanities at the University of Colorado Anschutz Medical Campus in Denver. "The fact that people have to scrounge for money to get life-saving treatment is unethical."
Crowdfunding also highlights socioeconomic and racial disparities by giving an unfair advantage to those who are social-media savvy and capable of crafting a compelling narrative that attracts donors. Privacy issues enter into the picture as well, because telling that narrative entails revealing personal details, Pierce says, particularly when it comes to children, "who may not be able to consent at a really informed level."
CoFund Health, the crowdfunding site on which Anderson raised the money for his plastic surgery, offers to help people write their campaigns and copy edit for proper language, says Matthew Martin, co-founder and chief executive officer. Like other crowdfunding sites, it retains a few percent of the donations for each campaign. Martin is the husband of Anderson's acquaintance from high school.
So far, the site, which is based in Raleigh, North Carolina, has hosted about 600 crowdfunding campaigns, some completed and some still in progress. Campaigns have raised as little as $300 to cover immediate dental expenses and as much as $12,000 for cancer treatments, Martin says, but most have set a goal between $5,000 and $10,000.
Whether or not someone's campaign is based on fact or fiction remains for prospective donors to decide.
The services could be cosmetic—for example, a breast enhancement or reduction, laser procedures for the eyes or skin, and chiropractic care. A number of campaigns have sought funding for transgender surgeries, which many insurers consider optional, he says.
In July 2019, a second site was hatched out of pet owners' requests for assistance with their dogs' and cats' medical expenses. Money raised on CoFund My Pet can only be used at veterinary clinics. Martin says the debit card would be declined at other merchants, just as its CoFund Health counterpart for humans will be rejected at places other than health care facilities, dental and vision providers, and pharmacies.
Whether or not someone's campaign is based on fact or fiction remains for prospective donors to decide. If a donor were to regret a transaction, he says the site would reach out to the campaign's owner but ultimately couldn't force a refund, Martin explains, because "it's hard to chase down fraud without having access to people's health records."
In some crowdfunding campaigns, the individual needs some or all the donated resources to pay for travel and lodging at faraway destinations to receive care, says Snyder, the health sciences professor and crowdfunding report author. He suggests people only give to recipients they know personally.
"That may change the calculus a little bit," tipping the decision in favor of donating, he says. As long as the treatment isn't harmful, the funds are a small gesture of support. "There's some value in that for preserving hope or just showing them that you care."
Three Big Biotech Ideas to Watch in 2020—And Beyond
Body-on-a-chip, prime editing, and gut microbes all are poised to make a big impact in 2020.
1. Happening Now: Body-on-a-Chip Technology Is Enabling Safer Drug Trials and Better Cancer Research
Researchers have increasingly used the technology known as "lab-on-a-chip" or "organ-on-a-chip" to test the effects of pharmaceuticals, toxins, and chemicals on humans. Rather than testing on animals, which raises ethical concerns and can sometimes be inaccurate, and human-based clinical trials, which can be expensive and difficult to iterate, scientists turn to tiny, micro-engineered chips—about the size of a thumb drive.
It's possible that doctors could one day take individual cell samples and create personalized treatments, testing out any medications on the chip.
The chips are lined with living samples of human cells, which mimic the physiology and mechanical forces experienced by cells inside the human body, down to blood flow and breathing motions; the functions of organs ranging from kidneys and lungs to skin, eyes, and the blood-brain barrier.
A more recent—and potentially even more useful—development takes organ-on-a-chip technology to the next level by integrating several chips into a "body-on-a-chip." Since human organs don't work in isolation, seeing how they all react—and interact—once a foreign element has been introduced can be crucial to understanding how a certain treatment will or won't perform. Dr. Shyni Varghese, a MEDx investigator at the Duke University School of Medicine, is one of the researchers working with these systems in order to gain a more nuanced understanding of how multiple different organs react to the same stimuli.
Her lab is working on "tumor-on-a-chip" models, which can not only show the progression and treatment of cancer, but also model how other organs would react to immunotherapy and other drugs. "The effect of drugs on different organs can be tested to identify potential side effects," Varghese says. In addition, these models can help the researchers figure out how cancers grow and spread, as well as how to effectively encourage immune cells to move in and attack a tumor.
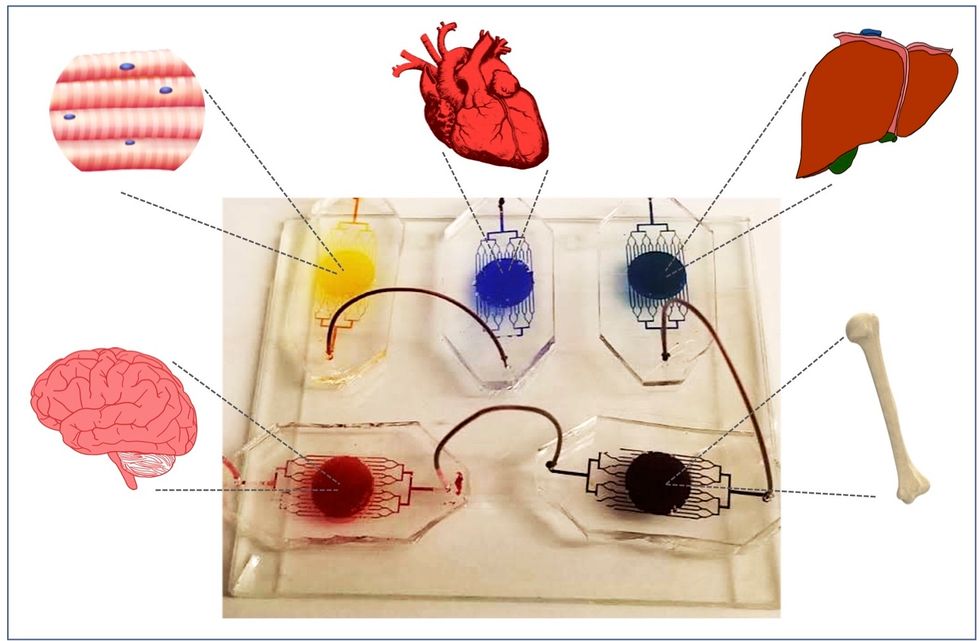
One body-on-a-chip used by Dr. Varghese's lab tracks the interactions of five organs—brain, heart, liver, muscle, and bone.
As their research progresses, Varghese and her team are looking for ways to maintain the long-term function of the engineered organs. In addition, she notes that this kind of research is not just useful for generalized testing; "organ-on-chip technologies allow patient-specific analyses, which can be used towards a fundamental understanding of disease progression," Varghese says. It's possible that doctors could one day take individual cell samples and create personalized treatments, testing out any medications on the chip for safety, efficacy, and potential side effects before writing a prescription.
2. Happening Soon: Prime Editing Will Have the Power to "Find and Replace" Disease-Causing Genes
Biochemist David Liu made industry-wide news last fall when he and his lab at MIT's Broad Institute, led by Andrew Anzalone, published a paper on prime editing: a new, more focused technology for editing genes. Prime editing is a descendant of the CRISPR-Cas9 system that researchers have been working with for years, and a cousin to Liu's previous innovation—base editing, which can make a limited number of changes to a single DNA letter at a time.
By contrast, prime editing has the potential to make much larger insertions and deletions; it also doesn't require the tweaked cells to divide in order to write the changes into the DNA, which could make it especially suitable for central nervous system diseases, like Parkinson's.
Crucially, the prime editing technique has a much higher efficiency rate than the older CRISPR system, and a much lower incidence of accidental insertions or deletions, which can make dangerous changes for a patient.
It also has a very broad potential range: according to Liu, 89% of the pathogenic mutations that have been collected in ClinVar (a public archive of human variations) could, in principle, be treated with prime editing—although he is careful to note that correcting a single genetic mutation may not be sufficient to fully treat a genetic disease.
Figuring out just how prime editing can be used most effectively and safely will be a long process, but it's already underway. The same day that Liu and his team posted their paper, they also made the basic prime editing constructs available for researchers around the world through Addgene, a plasmid repository, so that others in the scientific community can test out the technique for themselves. It might be years before human patients will see the results, and in the meantime, significant bioethical questions remain about the limits and sociological effects of such a powerful gene-editing tool. But in the long fight against genetic diseases, it's a huge step forward.
3. Happening When We Fund It: Focusing on Microbiome Health Could Help Us Tackle Social Inequality—And Vice Versa
The past decade has seen a growing awareness of the major role that the microbiome, the microbes present in our digestive tract, play in human health. Having a less-healthy microbiome is correlated with health risks like diabetes and depression, and interventions that target gut health, ranging from kombucha to fecal transplants, have cropped up with increasing frequency.
New research from the University of Maine's Dr. Suzanne Ishaq takes an even broader view, arguing that low-income and disadvantaged populations are less likely to have healthy, diverse gut bacteria, and that increasing access to beneficial microorganisms is an important juncture of social justice and public health.
"Basically, allowing people to lead healthy lives allows them to access and recruit microbes."
"Typically, having a more diverse bacterial community is associated with health, and having fewer different species is associated with illness and may leave you open to infection from bacteria that are good at exploiting opportunities," Ishaq says.
Having a healthy biome doesn't mean meeting one fixed ratio of gut bacteria, since different combinations of microbes can generate roughly similar results when they work in concert. Generally, "good" microbes are the ones that break down fiber and create the byproducts that we use for energy, or ones like lactic acid bacteria that work to make microbials and keep other bacteria in check. The microbial universe in your gut is chaotic, Ishaq says. "Microbes in your gut interact with each other, with you, with your food, or maybe they don't interact at all and pass right through you." Overall, it's tricky to name specific microbial communities that will make or break someone's health.
There are important corollaries between environment and biome health, though, which Ishaq points out: Living in urban environments reduces microbial exposure, and losing the microorganisms that humans typically source from soil and plants can reduce our adaptive immunity and ability to fight off conditions like allergies and asthma. Access to green space within cities can counteract those effects, but in the U.S. that access varies along income, education, and racial lines. Likewise, lower-income communities are more likely to live in food deserts or areas where the cheapest, most convenient food options are monotonous and low in fiber, further reducing microbial diversity.
Ishaq also suggests other areas that would benefit from further study, like the correlation between paid family leave, breastfeeding, and gut microbiota. There are technical and ethical challenges to direct experimentation with human populations—but that's not what Ishaq sees as the main impediment to future research.
"The biggest roadblock is money, and the solution is also money," she says. "Basically, allowing people to lead healthy lives allows them to access and recruit microbes."
That means investment in things we already understand to improve public health, like better education and healthcare, green space, and nutritious food. It also means funding ambitious, interdisciplinary research that will investigate the connections between urban infrastructure, housing policy, social equity, and the millions of microbes keeping us company day in and day out.
Scientists Just Started Testing a New Class of Drugs to Slow--and Even Reverse--Aging
Eliminating "zombie-like" cells, called senescent cells, may hold the key to slowing aging and its chronic diseases.
Imagine reversing the processes of aging. It's an age-old quest, and now a study from the Mayo Clinic may be the first ray of light in the dawn of that new era.
The immune system can handle a certain amount of senescence, but that capacity declines with age.
The small preliminary report, just nine patients, primarily looked at the safety and tolerability of the compounds used. But it also showed that a new class of small molecules called senolytics, which has proven to reverse markers of aging in animal studies, can work in humans.
Aging is a relentless assault of chronic diseases including Alzheimer's, cardiovascular disease, diabetes, and frailty. Developing one chronic condition strongly predicts the rapid onset of another. They pile on top of each other and impede the body's ability to respond to the next challenge.
"Potentially, by targeting fundamental aging processes, it may be possible to delay or prevent or alleviate multiple age-related conditions and many diseases as a group, instead of one at a time," says James Kirkland, the Mayo Clinic physician who led the study and is a top researcher in the growing field of geroscience, the biology of aging.
Getting Rid of "Zombie" Cells
One element common to many of the diseases is senescence, a kind of limbo or zombie-like state where cells no longer divide or perform many regular functions, but they don't die. Senescence is thought to be beneficial in that it inhibits the cancerous proliferation of cells. But in aging, the senescent cells still produce molecules that create inflammation both locally and throughout the body. It is a cycle that feeds upon itself, slowly ratcheting down normal body function and health.
Disease and harmful stimuli like radiation to treat cancer can also generate senescence, which is why young cancer patients seem to experience earlier and more rapid aging. The immune system can handle a certain amount of senescence, but that capacity declines with age. There also appears to be a threshold effect, a tipping point where senescence becomes a dominant factor in aging.
Kirkland's team used an artificial intelligence approach called machine learning to look for cell signaling networks that keep senescent cells from dying. To date, researchers have identified at least eight such signaling networks, some of which seem to be unique to a particular type of cell or tissue, but others are shared or overlap.
Then a computer search identified molecules known to disrupt these signaling pathways "and allow cells that are fully senescent to kill themselves," he explains. The process is a bit like looking for the right weapons in a video game to wipe out lingering zombie cells. But instead of swords, guns, and grenades, the list of biological tools so far includes experimental molecules, approved drugs, and natural supplements.
Treatment
"We found early on that targeting single components of those networks will only kill a very small minority of senescent cells or senescent cell types," says Kirkland. "So instead of going after one drug-one target-one disease, we're going after networks with combinations of drugs or drugs that have multiple targets. And we're going after every age-related disease."
The FDA is grappling with guidance for researchers wanting to conduct clinical trials on something as broad as aging rather than a single disease.
The large number of potential senolytic (i.e. zombie-neutralizing) compounds they identified allowed Kirkland to be choosy, "purposefully selecting drugs where the side effects profile was good...and with short elimination half-lives." The hit and run approach meant they didn't have to worry about maintaining a steady state of drugs in the body for an extended period of time. Some of the compounds they selected need only a half hour exposure to trigger the dying process in senescent cells, which can then take several days.
Work in mice has already shown impressive results in reversing diabetes, weight gain, Alzheimer's, cardiovascular disease and other conditions using senolytic agents.
That led to Kirkland's pilot study in humans with diabetes-related kidney disease using a three-day regimen of dasatinib, a kinase inhibitor first approved in 2006 to treat some forms of blood cancer, and quercetin, a flavonoid found in many plants and sold as a food supplement.
The combination was safe and well tolerated; it reduced the number of senescent cells in the belly fat of patients and restored their normal function, according to results published in September in the journal EBioMedicine. This preliminary paper was based on 9 patients in an ongoing study of 30 patients.
Kirkland cautions that these are initial and incomplete findings looking primarily at safety issues, not effectiveness. There is still much to be learned about the use of senolytics, starting with proof that they actually provide clinical benefit, and against what chronic conditions. The drug combinations, doses, duration, and frequency, not to mention potential risks all must be worked out. Additional studies of other diseases are being developed.
What's Next
Ron Kohanski, a senior administrator at the NIH National Institute on Aging (NIA), says the field of senolytics is so new that there isn't even a consensus on how to identify a senescent cell, and the FDA is grappling with guidance for researchers wanting to conduct clinical trials on something as broad as aging rather than a single disease.
Intellectual property concerns may temper the pharmaceutical industry's interest in developing senolytics to treat chronic diseases of aging. It looks like many mix-and-match combinations are possible, and many of the potential molecules identified so far are found in nature or are drugs whose patents have or will soon expire. So the ability to set high prices for such future drugs, and hence the willingness to spend money on expensive clinical trials, may be limited.
Still, Kohanski believes the field can move forward quickly because it often will include products that are already widely used and have a known safety profile. And approaches like Kirkland's hit and run strategy will minimize potential exposure and risk.
He says the NIA is going to support a number of clinical trials using these new approaches. Pharmaceutical companies may feel that they can develop a unique part of a senolytic combination regimen that will justify their investment. And if they don't, countries with socialized medicine may take the lead in supporting such research with the goal of reducing the costs of treating aging patients.

