A blood test may catch colorectal cancer before it's too late
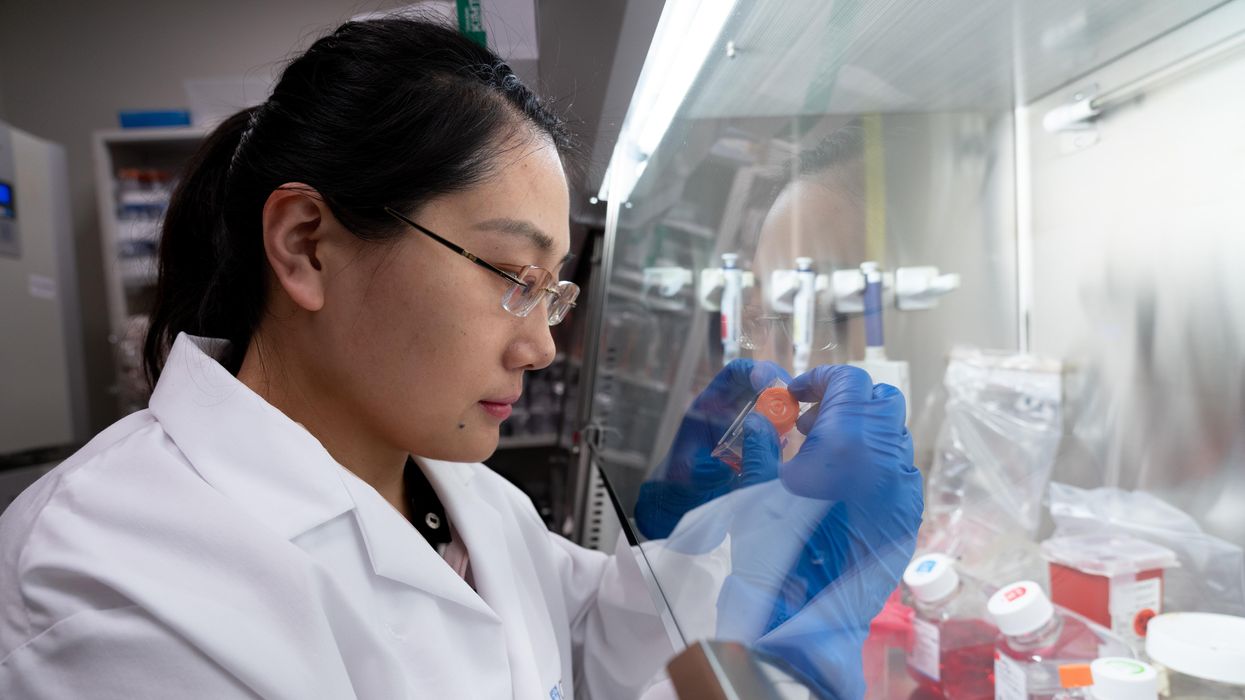
A scientist works on a blood test in the Ajay Goel Lab, one of many labs that are developing blood tests to screen for different types of cancer.
Soon it may be possible to find different types of cancer earlier than ever through a simple blood test.
Among the many blood tests in development, researchers announced in July that they have developed one that may screen for early-onset colorectal cancer. The new potential screening tool, detailed in a study in the journal Gastroenterology, represents a major step in noninvasively and inexpensively detecting nonhereditary colorectal cancer at an earlier and more treatable stage.
In recent years, this type of cancer has been on the upswing in adults under age 50 and in those without a family history. In 2021, the American Cancer Society's revised guidelines began recommending that colorectal cancer screenings with colonoscopy begin at age 45. But that still wouldn’t catch many early-onset cases among people in their 20s and 30s, says Ajay Goel, professor and chair of molecular diagnostics and experimental therapeutics at City of Hope, a Los Angeles-based nonprofit cancer research and treatment center that developed the new blood test.
“These people will mostly be missed because they will never be screened for it,” Goel says. Overall, colorectal cancer is the fourth most common malignancy, according to the U.S. Centers for Disease Control and Prevention.
Goel is far from the only one working on this. Dozens of companies are in the process of developing blood tests to screen for different types of malignancies.
Some estimates indicate that between one-fourth and one-third of all newly diagnosed colorectal cancers are early-onset. These patients generally present with more aggressive and advanced disease at diagnosis compared to late-onset colorectal cancer detected in people 50 years or older.
To develop his test, Goel examined publicly available datasets and figured out that changes in novel microRNAs, or miRNAs, which regulate the expression of genes, occurred in people with early-onset colorectal cancer. He confirmed these biomarkers by looking for them in the blood of 149 patients who had the early-onset form of the disease. In particular, Goel and his team of researchers were able to pick out four miRNAs that serve as a telltale sign of this cancer when they’re found in combination with each other.
The blood test is being validated by following another group of patients with early-onset colorectal cancer. “We have filed for intellectual property on this invention and are currently seeking biotech/pharma partners to license and commercialize this invention,” Goel says.
He’s far from the only one working on this. Dozens of companies are in the process of developing blood tests to screen for different types of malignancies, says Timothy Rebbeck, a professor of cancer prevention at the Harvard T.H. Chan School of Public Health and the Dana-Farber Cancer Institute. But, he adds, “It’s still very early, and the technology still needs a lot of work before it will revolutionize early detection.”
The accuracy of the early detection blood tests for cancer isn’t yet where researchers would like it to be. To use these tests widely in people without cancer, a very high degree of precision is needed, says David VanderWeele, interim director of the OncoSET Molecular Tumor Board at Northwestern University’s Lurie Cancer Center in Chicago.
Otherwise, “you’re going to cause a lot of anxiety unnecessarily if people have false-positive tests,” VanderWeele says. So far, “these tests are better at finding cancer when there’s a higher burden of cancer present,” although the goal is to detect cancer at the earliest stages. Even so, “we are making progress,” he adds.
While early detection is known to improve outcomes, most cancers are detected too late, often after they metastasize and people develop symptoms. Only five cancer types have recommended standard screenings, none of which involve blood tests—breast, cervical, colorectal, lung (smokers considered at risk) and prostate cancers, says Trish Rowland, vice president of corporate communications at GRAIL, a biotechnology company in Menlo Park, Calif., which developed a multi-cancer early detection blood test.
These recommended screenings check for individual cancers rather than looking for any form of cancer someone may have. The devil lies in the fact that cancers without widespread screening recommendations represent the vast majority of cancer diagnoses and most cancer deaths.
GRAIL’s Galleri multi-cancer early detection test is designed to find more cancers at earlier stages by analyzing DNA shed into the bloodstream by cells—with as few false positives as possible, she says. The test is currently available by prescription only for those with an elevated risk of cancer. Consumers can request it from their healthcare or telemedicine provider. “Galleri can detect a shared cancer signal across more than 50 types of cancers through a simple blood draw,” Rowland says, adding that it can be integrated into annual health checks and routine blood work.
Cancer patients—even those with early and curable disease—often have tumor cells circulating in their blood. “These tumor cells act as a biomarker and can be used for cancer detection and diagnosis,” says Andrew Wang, a radiation oncologist and professor at the University of Texas Southwestern Medical Center in Dallas. “Our research goal is to be able to detect these tumor cells to help with cancer management.” Collaborating with Seungpyo Hong, the Milton J. Henrichs Chair and Professor at the University of Wisconsin-Madison School of Pharmacy, “we have developed a highly sensitive assay to capture these circulating tumor cells.”
Even if the quality of a blood test is superior, finding cancer early doesn’t always mean it’s absolutely best to treat it. For example, prostate cancer treatment’s potential side effects—the inability to control urine or have sex—may be worse than living with a slow-growing tumor that is unlikely to be fatal. “[The test] needs to tell me, am I going to die of that cancer? And, if I intervene, will I live longer?” says John Marshall, chief of hematology and oncology at Medstar Georgetown University Hospital in Washington, D.C.

Ajay Goel Lab
A blood test developed at the University of Texas MD Anderson Cancer Center in Houston helps predict who may benefit from lung cancer screening when it is combined with a risk model based on an individual’s smoking history, according to a study published in January in the Journal of Clinical Oncology. The personalized lung cancer risk assessment was more sensitive and specific than the 2021 and 2013 U.S. Preventive Services Task Force criteria.
The study involved participants from the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial with a minimum of a 10 pack-year smoking history, meaning they smoked 20 cigarettes per day for ten years. If implemented, the blood test plus model would have found 9.2 percent more lung cancer cases for screening and decreased referral to screening among non-cases by 13.7 percent compared to the 2021 task force criteria, according to Oncology Times.
The conventional type of screening for lung cancer is an annual low-dose CT scan, but only a small percentage of people who are eligible will actually get these scans, says Sam Hanash, professor of clinical cancer prevention and director of MD Anderson’s Center for Global Cancer Early Detection. Such screening is not readily available in most countries.
In methodically searching for blood-based biomarkers for lung cancer screening, MD Anderson researchers developed a simple test consisting of four proteins. These proteins circulating in the blood were at high levels in individuals who had lung cancer or later developed it, Hanash says.
“The interest in blood tests for cancer early detection has skyrocketed in the past few years,” he notes, “due in part to advances in technology and a better understanding of cancer causation, cancer drivers and molecular changes that occur with cancer development.”
However, at the present time, none of the blood tests being considered eliminate the need for screening of eligible subjects using established methods, such as colonoscopy for colorectal cancer. Yet, Hanash says, “they have the potential to complement these modalities.”
Why Neglected Tropical Diseases Should Matter to Americans
Kissing bugs can carry a parasite called Trypanosoma cruzi, which causes Chagas disease.
Daisy Hernández was five years old when one of her favorite aunts was struck with a mysterious illness. Tía Dora had stayed behind in Colombia when Daisy's mother immigrated to Union City, New Jersey. A schoolteacher in her late 20s, she began suffering from fevers and abdominal pain, and her belly grew so big that people thought she was pregnant. Exploratory surgery revealed that her large intestine had swollen to ten times its normal size, and she was fitted with a colostomy bag. Doctors couldn't identify the underlying problem—but whatever it was, they said, it would likely kill her within a year or two.
Tía Dora's sisters in New Jersey—Hernández's mother and two other aunts—weren't about to let that happen. They pooled their savings and flew her to New York City, where a doctor at Columbia-Presbyterian Medical Center with a penchant for obscure ailments provided a diagnosis: Chagas disease. Transmitted by the bite of triatomine insects, commonly known as kissing bugs, Chagas is endemic in many parts of Latin America. It's caused by the parasite Trypanoma cruzi, which usually settles in the heart, where it feeds on muscle tissue. In some cases, however, it attacks the intestines or esophagus. Tía Dora belonged to that minority.
In 1980, U.S. immigration laws were more forgiving than they are today. Tía Dora was able to have surgery to remove a part of her colon, despite not being a citizen or having a green card. She eventually married a legal resident and began teaching Spanish at an elementary school. Over the next three decades, she earned a graduate degree, built a career, and was widowed. Meanwhile, Chagas continued its slow devastation. "Every couple of years, we were back in the hospital with her," Hernández recalls. "When I was in high school, she started feeling like she couldn't swallow anything. It was the parasite, destroying the muscles of her esophagus."
When Tía Dora died in 2010, at 59, her niece was among the family members at her bedside. By then, Hernández had become a journalist and fiction writer. Researching a short story about Chagas disease, she discovered that it affected an estimated 6 million people in South America, Central America, and Mexico—as well as 300,000 in the United States, most of whom were immigrants from those places. "I was shocked to learn it wasn't rare," she says. "That made me hungry to know more about this disease, and about the families grappling with it."
Hernández's curiosity led her to write The Kissing Bug, a lyrical hybrid of memoir and science reporting that was published in June. It also led her to another revelation: Chagas is not unique. It's among the many maladies that global health experts refer to as neglected tropical diseases—often-disabling illnesses that afflict 1.7 billion people worldwide, while getting notably less attention than the "big three" of HIV/AIDs, malaria, and tuberculosis. NTDs cause fewer deaths than those plagues, but they wreak untold suffering and economic loss.
Shortly before Hernández's book hit the shelves, the World Health Organization released its 2021-2030 roadmap for fighting NTDs. The plan sets targets for controlling, eliminating, or eradicating all the diseases on the WHO's list, through measures ranging from developing vaccines to improving healthcare infrastructure, sanitation, and access to clean water. Experts agree that for the campaign to succeed, leadership from wealthy nations—particularly the United States—is essential. But given the inward turn of many such countries in recent years (evidenced in movements ranging from America First to Brexit), and the continuing urgency of the COVID-19 crisis, public support is far from guaranteed.
As Hernández writes: "It is easier to forget a disease that cannot be seen." NTDs primarily affect residents of distant lands. They kill only 80,000 people a year, down from 204,000 in 1990. So why should Americans to bother to look?
Breaking the circle of poverty and disease
The World Health Organization counts 20 diseases as NTDs. Along with Chagas, they include dengue and chikungunya, which cause high fevers and agonizing pain; elephantiasis, which deforms victims' limbs and genitals; onchocerciasis, which causes blindness; schistosomiasis, which can damage the heart, lungs, brain, and genitourinary system; helminths such as roundworm and whipworm, which cause anemia, stunted growth, and cognitive disabilities; and a dozen more. Such ailments often co-occur in the same patient, exacerbating each other's effects and those of illnesses such as malaria.
NTDs may be spread by insects, animals, soil, or tainted water; they may be parasitic, bacterial, viral, or—in the case of snakebite envenoming—non-infectious. What they have in common is their longtime neglect by public health agencies and philanthropies. In part, this reflects their typically low mortality rates. But the biggest factor is undoubtedly their disempowered patient populations.
"These diseases occur in the setting of poverty, and they cause poverty, because of their chronic and debilitating effects," observes Peter Hotez, dean of the National School of Tropical Medicine at Baylor University and co-director of the Texas Children's Hospital for Vaccine Development. And historically, the everyday miseries of impoverished people have seldom been a priority for those who set the global health agenda.
That began to change about 20 years ago, when Hotez and others developed the conceptual framework for NTDs and early proposals for combating them. The WHO released its first roadmap in 2012, targeting 17 NTDs for control, elimination, or eradication by 2020. (Rabies, snakebite, and dengue were added later.) Since then, the number of people at risk for NTDs has fallen by 600 million, and 42 countries have eliminated at least one such disease. Cases of dracunculiasis—known as Guinea worm disease, for the parasite that creates painful blisters in a patient's skin—have dropped from the millions to just 27 in 2020.
Yet the battle is not over, and the COVID-19 pandemic has disrupted prevention and treatment programs around the globe.
A new direction — and longstanding obstacles
The WHO's new roadmap sets even more ambitious goals for 2030. Among them: reducing by 90 percent the number of people requiring treatment for NTDs; eliminating at least one NTD in another 100 countries; and fully eradicating dracunculiasis and yaws, a disfiguring skin infection.
The plan also places an increased focus on "country ownership," relying on nations with high incidence of NTDs to design their own plans based on local expertise. "I was so excited to see that," says Kristina Talbert-Slagle, director of the Yale College Global Health Studies program. "No one is a better expert on how to address these situations than the people who deal with it day by day."
Another fresh approach is what the roadmap calls "cross-cutting" targets. "One of the really cool things about the plan is how much it emphasizes coordination among different sectors of the health system," says Claire Standley, a faculty member at Georgetown University's Center for Global Health Science and Security. "For example, it explicitly takes into account the zoonotic nature of many neglected tropical diseases—the fact that we have to think about animal health as well as human health when we tackle NTDs."
Whether this grand vision can be realized, however, will depend largely on funding—and that, in turn, is a question of political will in the countries most able to provide it. On the upside, the U.S. has ended its Trump-era feud with the WHO. "One thing that's been really encouraging," says Standley, "has been the strong commitment toward global cooperation from the current administration." Even under the previous president, the U.S. remained the single largest contributor to the global health kitty, spending over $100 million annually on NTDs—six times the figure in 2006, when such financing started.
On the downside, America's outlay has remained flat for several years, and the Biden administration has so far not moved to increase it. A "back-of-the-envelope calculation," says Hotez, suggests that the current level of aid could buy medications for the most common NTDs for about 200 million people a year. But the number of people who need treatment, he notes, is at least 750 million.
Up to now, the United Kingdom—long the world's second-most generous health aid donor—has taken up a large portion of the slack. But the UK last month announced deep cuts in its portfolio, eliminating 102 previously supported countries and leaving only 34. "That really concerns me," Hotez says.
The struggle for funds, he notes, is always harder for projects involving NTDs than for those aimed at higher-profile diseases. His lab, which he co-directs with microbiologist Maria Elena Bottazzi, started developing a COVID-19 vaccine soon after the pandemic struck, for example, and is now in Phase 3 trials. The team has been working on vaccines for Chagas, hookworm, and schistosomiasis for much longer, but trials for those potential game-changers lag behind. "We struggle to get the level of resources needed to move quickly," Hotez explains.
Two million reasons to care
One way to prompt a government to open its pocketbook is for voters to clamor for action. A longtime challenge with NTDs, however, has been getting people outside the hardest-hit countries to pay attention.
The reasons to care, global health experts argue, go beyond compassion. "When we have high NTD burden," says Talbert-Slagle, "it can prevent economic growth, prevent innovation, lead to more political instability." That, in turn, can lead to wars and mass migration, affecting economic and political events far beyond an affected country's borders.
Like Hernández's aunt Dora, many people driven out of NTD-wracked regions wind up living elsewhere. And that points to another reason to care about these diseases: Some of your neighbors might have them. In the U.S., up to 14 million people suffer from neglected parasitic infections—including 70,000 with Chagas in California alone.
When Hernández was researching The Kissing Bug, she worried that such statistics would provide ammunition to racists and xenophobes who claim that immigrants "bring disease" or exploit overburdened healthcare systems. (This may help explain some of the stigma around NTDs, which led Tía Dora to hide her condition from most people outside her family.) But as the book makes clear, these infections know no borders; they flourish wherever large numbers of people lack access to resources that most residents of rich countries take for granted.
Indeed, far from gaming U.S. healthcare systems, millions of low-income immigrants can't access them—or must wait until they're sick enough to go to an emergency room. Since Congress changed the rules in 1996, green card holders have to wait five years before they can enroll in Medicaid. Undocumented immigrants can never qualify.
Closing the great divide
Hernández uses a phrase borrowed from global health crusader Paul Farmer to describe this access gap: "the great epi divide." On one side, she explains, "people will die from cancer, from diabetes, from chronic illnesses later in life. On the other side of the epidemiological divide, people are dying because they can't get to the doctor, or they can't get medication. They don't have a hospital anywhere near them. When I read Dr. Farmer's work, I realized how much that applied to neglected diseases as well."
When it comes to Chagas disease, she says, the epi divide is embodied in the lack of a federal mandate for prenatal or newborn screening. Each year, according to the Centers for Disease Control and Prevention, up to 300 babies in the U.S. are born with Chagas, which can be passed from the mother in utero. The disease can be cured with medication if treated in infancy. (It can also be cured in adults in the acute stage, but is seldom detected in time.) Yet the CDC does not require screening for Chagas—even though newborns are tested for 15 diseases that are less common. According to one study, it would be 10 times cheaper to screen and treat babies and their mothers than to cover the costs related to the illness in later years. Few states make the effort.
The gap that enables NTDs to persist, Hernández argues, is the same one that has led to COVID-19 death rates in Black and Latinx communities that are double those elsewhere in America. To close it, she suggests, caring is not enough.
"When I was working on my book," she says, "I thought about HIV in the '80s, when it had so much stigma that no one wanted to talk about it. Then activists stepped up and changed the conversation. I thought a lot about breast cancer, which was stigmatized for years, until people stepped forward and started speaking out. I thought about Lyme disease. And it wasn't only patients—it was also allies, right? The same thing needs to happen with neglected diseases around the world. Allies need to step up and make demands on policymakers. We need to make some noise."
When Wayne Jonas was in medical school 40 years ago, doctors would write out a prescription for placebos, spelling it out backwards in capital letters, O-B-E-C-A-L-P. The pharmacist would fill the prescription with a sugar pill, recalls Jonas, now director of integrative health programs at the Samueli Foundation. It fulfilled the patient's desire for the doctor to do something when perhaps no drug could help, and the sugar pills did no harm.
Today, that deception is seen as unethical. But time and time again, studies have shown that placebos can have real benefits. Now, researchers are trying to untangle the mysteries of placebo effect in an effort to better treat patients.
The use of placebos took off in the post-WWII period, when randomized controlled clinical trials became the gold standard for medical research. One group in a study would be treated with a placebo, a supposedly inert pill or procedure that would not affect normal healing and recovery, while another group in the study would receive an "active" component, most commonly a pill under investigation. Presumably, the group receiving the active treatment would have a better response and the difference from the placebo group would represent the efficacy of the drug being tested. That was the basis for drug approval by the U.S. Food and Drug Administration.
"Placebo responses were marginalized," says Ted Kaptchuk, director of the Program in Placebo Studies & Therapeutic Encounters at Harvard Medical School. "Doctors were taught they have to overcome it when they were thinking about using an effective drug."
But that began to change around the turn of the 21st century. The National Institutes of Health held a series of meetings to set a research agenda and fund studies to answer some basic questions, led by Jonas who was in charge of the office of alternative medicine at the time. "People spontaneously get better all the time," says Kaptchuk. The crucial question was, is the placebo effect real? Is it more than just spontaneous healing?
Brain mechanisms
A turning point came in 2001 in a paper in Science that showed physical evidence of the placebo effect. It used positron emission tomography (PET) scans to measure release patterns of dopamine — a chemical messenger involved in how we feel pleasure — in the brains of patients with Parkinson's disease. Surprisingly, the placebo activated the same patterns that were activated by Parkinson's drugs, such as levodopa. It proved the placebo effect was real; now the search was on to better understand and control it.
A key part of the effect can be the beliefs, expectations, context, and "rituals" of the encounter between doctor and patient. Belief by the doctor and patient that the treatment would work, and the formalized practices of administering the treatment can all contribute to a positive outcome.
Conditioning can be another important component in generating a response, as Pavlov demonstrated more than a century ago in his experiments with dogs. They were trained with a bell prior to feeding such that they would begin to salivate in anticipation at the sound of a bell even with no food present.
Translating that to humans, studies with pain medications and sleeping aids showed that patients who had a positive response with a certain dose of those medications could have the same response if the doses was reduced and a dummy pill substituted, even to the point where there was no longer any active ingredient.
Researchers think placebo treatments can work particularly well in helping people deal with pain and psychological disorders.
Those types of studies troubled Kaptchuk because they often relied on deception; patients weren't told they were receiving a placebo, or at best there was a possibility that they might be randomized to receive a placebo. He believed the placebo effect could work even if patients were told upfront that they were going to receive a placebo. More than a dozen so call "open-label placebo" studies across numerous medical conditions, by Kaptchuk and others, have shown that you don't have to lie to patients for a placebo to work.
Jonas likes to tell the story of a patient who used methotrexate, a potent immunosuppressant, to control her rheumatoid arthritis. She was planning a long trip and didn't want to be bothered with the injections and monitoring required in using the drug, So she began to drink a powerful herbal extract of anise, a licorice flavor that she hated, prior to each injection. She reduced the amount of methotrexate over a period of months and finally stopped, but continued to drink the anise. That process had conditioned her body "to alter her immune function and her autoimmunity" as if she were taking the drug, much like Pavlov's dogs had been trained. She has not taken methotrexate for more than a year.
An intriguing paper published in May found that mild, non-invasive electric stimulation to the brain could not only boost the placebo effect on pain but also reduce the "nocebo" effect — when patients report a negative effect to a sham treatment. While the work is very preliminary, it may open the door to directly manipulating these responses.
Researchers think placebo treatments can work particularly well in helping people deal with pain and psychological disorders, areas where drugs often are of little help. Still, placebos aren't a cure and only a portion of patients experience a placebo effect.
Nocebo
If medicine were a soap opera, the nocebo would be the evil twin of the placebo. It's what happens when patients have adverse side effects because of the expectation that they will. It's commonly seem when patients claims to experience pain or gastric distress that can occur with a drug even when they've received a placebo. The side effects were either imagined or caused by something else.
"Up to 97% of reported pharmaceutical side effects are not caused by the drug itself but rather by nocebo effects and symptom misattribution," according to one 2019 paper.
One way to reduce a nocebo response is to simply not tell patients that specific side effects might occur. An example is a liver biopsy, in which a large-gauge needle is used to extract a tissue sample for examination. Those told ahead of time that they might experience some pain were more likely to report pain and greater pain than those who weren't offered this information.
Interestingly, a nocebo response plays out in the hippocampus, a part of the brain that is never activated in a placebo response. "I think what we are dealing with with nocebo is anxiety," says Kaptchuk, but he acknowledges that others disagree.
Distraction may be another way to minimize the nocebo effect. Pediatricians are using virtual reality (VR) to engage children and distract them during routine procedures such as blood draws and changing wound dressings, and burn patients of all ages have found relief with specially created VRs.
Treatment response
Jonas argues that what we commonly call the placebo effect is misnamed and leading us astray. "The fact is people heal and that inherent healing capacity is both powerful and influenced by mental, social, and contextual factors that are embedded in every medical encounter since the idea of treatment began," he wrote in a 2019 article in the journal Frontiers in Psychiatry. "Our understanding of healing and ability to enhance it will be accelerated if we stop using the term 'placebo response' and call it what it is—the meaning response, and its special application in medicine called the healing response."
He cites evidence that "only 15% to 20% of the healing of an individual or a population comes from health care. The rest—nearly 80%—comes from other factors rarely addressed in the health care system: behavioral and lifestyle choices that people make in their daily life."
To better align treatments and maximize their effectiveness, Jonas has created HOPE (Healing Oriented Practices & Environments) Note, "a patient-guided process designed to identify the patient's values and goals in their life and for healing." Essentially, it seeks to make clear to both doctor and patient what the patient's goals are in seeking treatment. In an extreme example of terminal cancer, some patients may choose to extend life despite the often brutal treatments, while others might prefer to optimize quality of life in the remaining time that they have. It builds on practices already taught in medical schools. Jonas believes doctors and patients can use tools like these to maximize the treatment response and achieve better outcomes.
Much of the medical profession has been resistant to these approaches. Part of that is simply tradition and limited data on their effectiveness, but another very real factor is the billing process for how they are reimbursed. Jonas says a new medical billing code added this year gives doctors another way to be compensated for the extra time and effort that a more holistic approach to medicine may initially require. Other moves away from fee-for-service payments to bundling and payment for outcomes, and the integrated care provided by the Veterans Affairs, Kaiser Permanente and other groups offer longer term hope for the future of approaches that might enhance the healing response.

