Can an “old school” vaccine address global inequities in Covid-19 vaccination?

Scientists at Baylor College of Medicine developed a vaccine called Corbevax that, unlike mRNA vaccines, can be mass produced using technology already in place in low- and middle-income countries. It's now being administered in India to children aged 12-14.
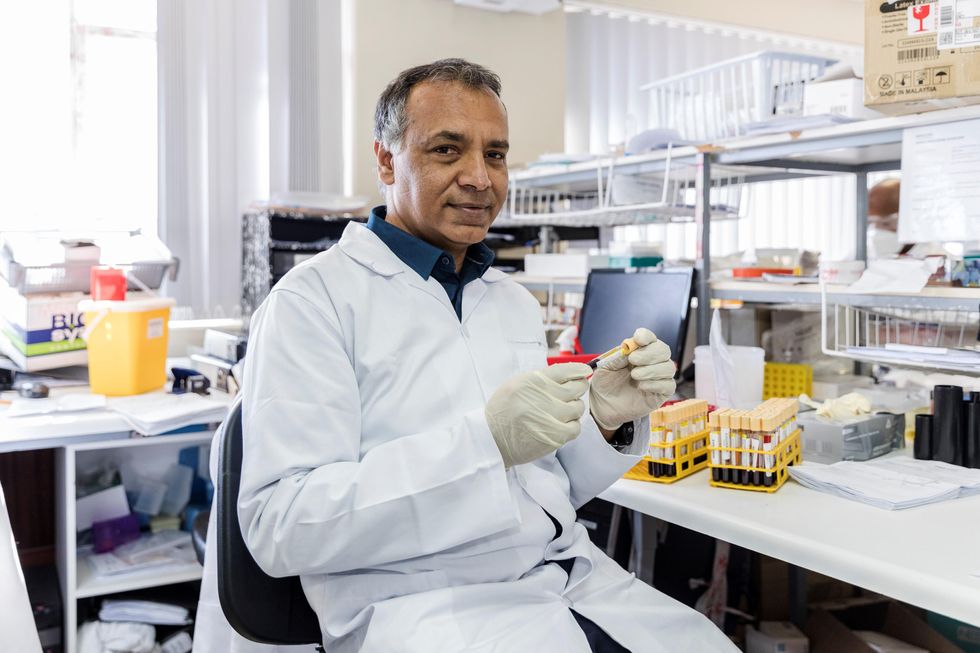
When the COVID-19 pandemic began invading the world in late 2019, Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. The scientists, with their prior experience of developing inexpensive vaccines for the world’s poor, had anticipated that the global rollout of Covid-19 jabs would be marked with several inequities. They wanted to create a patent-free vaccine to bridge this gap, but the U.S. government did not seem impressed, forcing the researchers to turn to private philanthropies for funds.
Hotez and Bottazzi, both scientists at the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, raised about $9 million in private funds. Meanwhile, the U.S. government’s contribution stood at $400,000.
“That was a very tough time early on in the pandemic, you know, trying to do the work and raise the money for it at the same time,” says Hotez, who was nominated in February for a Nobel Peace Prize with Bottazzi for their COVID-19 vaccine. He adds that at the beginning of the pandemic, governments emphasized speed, innovation and rapidly immunizing populations in North America and Europe with little consideration for poorer countries. “We knew this [vaccine] was going to be the answer to global vaccine inequality, but I just wish the policymakers had felt the same,” says Hotez.
Over the past two years, the world has witnessed 488 million COVID-19 infections and over 61 million deaths. Over 11 billion vaccine doses have been administered worldwide; however, the global rollout of COVID-19 vaccines is marked with alarming socio-economic inequities. For instance, 72 percent of the population in high-income countries has received at least one dose of the vaccine, whereas the number stands at 15 percent in low-income countries.
This inequity is worsening vulnerabilities across the world, says Lawrence Young, a virologist and co-lead of the Warwick Health Global Research Priority at the UK-based University of Warwick. “As long as the virus continues to spread and replicate, particularly in populations who are under-vaccinated, it will throw up new variants and these will remain a continual threat even to those countries with high rates of vaccination,” says Young, “Therefore, it is in all our interests to ensure that vaccines are distributed equitably across the world.”
“When your house is on fire, you don't call the patent attorney,” says Hotez. “We wanted to be the fire department.”
The vaccine developed by Hotez and Bottazzi recently received emergency use authorisation in India, which plans to manufacture 100 million doses every month. Dubbed ‘Corbevax’ by its Indian maker, Biological E Limited, the vaccine is now being administered in India to children aged 12-14. The patent-free arrangement means that other low- and middle-income countries could also produce and distribute the vaccine locally.
“When your house is on fire, you don't call the patent attorney, you call the fire department,” says Hotez, commenting on the intellectual property rights waiver. “We wanted to be the fire department.”
The Inequity
Vaccine equity simply means that all people, irrespective of their location, should have equal access to vaccines. However, data suggests that the global COVID-19 vaccine rollout has favoured those in richer countries. For instance, high-income countries like the UAE, Portugal, Chile, Singapore, Australia, Malta, Hong Kong and Canada have partially vaccinated over 85 percent of their populations. This percentage in poorer countries, meanwhile, is abysmally low – 2.1 percent in Yemen, 4.6 in South Sudan, 5 in Cameroon, 9.9 in Burkina Faso, 10 in Nigeria, 12 in Somalia, 12 in Congo, 13 in Afghanistan and 21 in Ethiopia.

In late 2019, scientists Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. In February, they were nominated for a Nobel Peace Prize.
Texas Children's Hospital
The COVID-19 vaccination coverage is particularly low in African countries, and according to Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of African Local Initiative for Vaccinology Expertise, vaccine access and inequity remains a challenge in Africa. Madhi adds that a lack of vaccine access has affected the pandemic’s trajectory on the continent, but a majority of its people have now developed immunity through natural infection. “This has come at a high cost of loss of lives,” he says.
COVID-19 vaccines mean a significant financial burden for poorer countries, which spend an average of $41 per capita annually on health, while the average cost of every COVID-19 vaccine dose ranges between $2 and $40 in addition to a distribution cost of $3.70 per person for two doses. In December last year, the World Health Organisation (WHO) set a goal of immunizing 70 percent of the population of all countries by mid-2022. This, however, means that low-income countries would have to increase their health expenditure by an average of 56.6 percent to cover the cost, as opposed to 0.8 per cent in high-income countries.
Reflecting on the factors that have driven global inequity in COVID-19 vaccine distribution, Andrea Taylor, assistant director of programs at the Duke Global Health Innovation Center, says that wealthy nations took the risk of investing heavily in the development and scaling up of COVID-19 vaccines – at a time when there was little evidence to show that vaccines would work. This reserved a place for these nations at the front of the queue when doses started rolling off production lines. Lower-income countries, meanwhile, could not afford such investments.
“Now, however, global supply is not the issue,” says Taylor. “We are making plenty of doses to meet global need. The main problem is infrastructure to get the vaccine where it is most needed in a predictable and timely way and to ensure that countries have all the support they need to store, transport, and use the vaccine once it is received.”

Taufique Joarder, vice-chairperson of Bangladesh's Public Health Foundation, sees the need for more trials and data before Corbevax is made available to the general population.
In addition to global inequities in vaccination coverage, there are inequities within nations. Taufique Joarder, vice-chairperson of Bangladesh’s Public Health Foundation, points to the situation in his country, where vaccination coverage in rural and economically disadvantaged communities has suffered owing to weak vaccine-promotion initiatives and the difficulty many people face in registering online for jabs.
Joarder also cites the example of the COVID-19 immunization drive for children aged 12 years and above. “[Children] are given the Pfizer vaccine, which requires an ultralow temperature for storage. This is almost impossible to administer in many parts of the country, especially the rural areas. So, a large proportion of the children are being left out of vaccination,” says Joarder, adding that Corbevax, which is cheaper and requires regular temperature refrigeration “can be an excellent alternative to Pfizer for vaccinating rural children.”
Corbevax vs. mRNA Vaccines
As opposed to most other COVID-19 vaccines, which use the new Messenger RNA (mRNA) vaccine technology, Corbevax is an “old school” vaccine, says Hotez. The vaccine is made through microbial fermentation in yeast, similar to the process used to produce the recombinant hepatitis B vaccine, which has been administered to children in several countries for decades. Hence, says Hotez, the technology to produce Corbevax at large scales is already in place in countries like Vietnam, Bangladesh, India, Indonesia, Brazil, Argentina, among many others.
“So if you want to rapidly develop and produce and empower low- and middle-income countries, this is the technology to do it,” he says.
“Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines," says Andrea Taylor.
The COVID-19 vaccines created by Pfizer-BioNTech and Moderna marked the first time that mRNA vaccine technology was approved for use. However, scientists like Young feel that there is “a need to be pragmatic and not seduced by new technologies when older, tried and tested approaches can also be effective.” Taylor, meanwhile, says that although mRNA vaccines have dominated the COVID-19 vaccine market in the U.S., “there is no clear grounding for this preference in the data we have so far.” She adds that there is also growing evidence that the immunity from these shots may not hold up as well over time as that of vaccines using different platforms.
“The mRNA vaccines are well suited to wealthy countries with sufficient ultra-cold storage and transportation infrastructure, but these vaccines are divas and do not travel well in the rest of the world,” says Taylor. “Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines, such as the protein subunit platform used by Novavax and Corbevax. These require only standard refrigeration, can be manufactured using existing facilities all over the world, and are easy to transport.”
Joarder adds that Corbevax is cheaper due to the developers’ waived intellectual rights. It could also be used as a booster vaccine in Bangladesh, where only five per cent of the population has currently received booster doses. “If this vaccine is proved effective for heterologous boosting, [meaning] it works well and is well tolerated as a booster with other vaccines that are available in Bangladesh, this can be useful,” says Joarder.
According to Hotez, Corbevax can play several important roles - as a standalone adult or paediatric vaccine, and as a booster for other vaccines. Studies are underway to determine Corbevax’s effectiveness in these regards, he says.
Need for More Data
Biological E conducted two clinical trials involving 3000 subjects in India, and found Corbevax to be “safe and immunogenic,” with 90 percent effectiveness in preventing symptomatic infections from the original strain of COVID-19 and over 80 percent effectiveness against the Delta variant. The vaccine is currently in use in India, and according to Hotez, it’s in the pipeline at different stages in Indonesia, Bangladesh and Botswana.
However, Corbevax is yet to receive emergency use approval from the WHO. Experts such as Joarder see the need for more trials and data before it is made available to the general population. He says that while the WHO’s emergency approval is essential for global scale-up of the vaccine, we need data to determine age-stratified efficacy of the vaccine and whether it can be used for heterologous boosting with other vaccines. “According to the most recent data, the 100 percent circulating variant in Bangladesh is Omicron. We need to know how effective is Corbevax against the Omicron variant,” says Joarder.
Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of the African Local Initiative for Vaccinology Expertise, says that a majority of people in Africa have now developed immunity through natural infection. “This has come at a high cost of loss of lives."
Shivan Parusnath
Others, meanwhile, believe that availing vaccines to poorer countries is not enough to resolve the inequity. Young, the Warwick virologist, says that the global vaccination rollout has also suffered from a degree of vaccine hesitancy, echoing similar observations by President Biden and Pfizer’s CEO. The problem can be blamed on poor communication about the benefits of vaccination. “The Corbevax vaccine [helps with the issues of] patent protection, vaccine storage and distribution, but governments need to ensure that their people are clearly informed.” Notably, however, some research has found higher vaccine willingness in lower-income countries than in the U.S.
Young also emphasized the importance of establishing local vaccination stations to improve access. For some countries, meanwhile, it may be too late. Speaking about the African continent, Madhi says that Corbevax has arrived following the peak of the crisis and won’t reverse the suffering and death that has transpired because of vaccine hoarding by high-income countries.
“The same goes for all the sudden donations from countries such as France - pretty much of little to no value when the pandemic is at its tail end,” says Madhi. “This, unfortunately, is a repeat of the swine flu pandemic in 2009, when vaccines only became available to Africa after the pandemic had very much subsided.”
Companies such as Wave and Magment offer a variety of approaches for charging vehicles without plugs while they're being stored or even used, but costs stand in the way of broader adoption.
Starting this summer, the public buses in the Oberhaching suburb of Munich, Germany, won’t have to be plugged in to charge overnight anymore. Stefan Schelle, the mayor of Oberhaching, is taking advantage of the fact that an innovative startup has its offices in his community: Magment, short for “magnetizing cement,” will install its underground charging pad in the coming months. As soon as that happens, the buses will charge while they wait at the city’s main station or while stored at their overnight quarters.
In his light-filled office, Magment’s co-founder and CEO, Mauricio Esguerra, demonstrates how the new technology works: The lights on his black model car only flash when he puts the miniature Porsche directly atop the induction plate. “This works just like when you charge your iPhone on its charging pad or heat a pot on an induction range. People don’t have to be afraid of magnetic fields or anything like that,” says the 60-year-old Colombia-born entrepreneur. “The induction only gets activated when the storage battery is placed directly on top.
Patented by Esguerra, the “magnetizing concrete” is able to target the charge quite precisely. The batteries will be mounted in a box underneath the vehicles such as the retrofitted public buses. “Look, here’s one passing by,” says Esguerra, pointing out the window as a blue city bus rides past his office.
An invention finds its purpose
Esguerra grew up in Bogotá, studied physics at the Technical University Munich where he fell in love with a German woman, and started a family in her home country. For 15 years, he developed magnetic products, including the magnetizing cement, for Siemens, Europe’s largest industrial manufacturing company. The patent belonged to Siemens, of course. “But there were hardly any electric vehicles yet,” Esguerra says, “and Siemens didn’t quite know what to do with this invention.”
Esguerra changed companies a few times but, in 2015, he got an offer from Siemens. The patent for the magnetizing cement was expiring and Siemens wasn’t interested in keeping it. Would he, as the inventor, want it back? “I did not hesitate a second,” Esguerra remembers with a smile. “I’m a magnetician at heart.” That same year, he founded Magment to finally make use of the technology he created 20 years ago.
To demonstrate how his cement is made, he opens the lid of a plastic bucket filled with cement powder. Mixed in are fingernail-sized black pieces, so-called ferrites, mainly consisting of three ceramic oxides: iron, nickel and zinc. Conventionally, they are used in electronics such as cell phones, computers and cables. Molded in concrete, ferrites create a magnetic field that can transport charge to a vehicle, potentially eliminating range anxiety for EV drivers.

Molded in concrete, ferrites create a magnetic field that can transport charge to a vehicle, potentially eliminating range anxiety for EV drivers.
Magment
“Ferrites have extremely high rejection rates,” Esguerra adds. “It’s comparable to other ceramics: As soon as there is a small tear or crack, the material is rejected. We are talking about a rejection pile of 500,000 tons per year worldwide. There are mountains of unused materials.”
Exactly this fact was the starting point of his research at Siemens: “What can we do with this energy-intensive material? Back then, it was crushed up and mixed into the cement for building streets, without adding any function.” Today, too, the Magment material can simply be mixed with the conventional material and equipment of the cement industry. “We take advantage of the fact that we don’t have to build factories and don’t have high transportation costs."
In addition to saving resources, recycled ferrite also makes concrete more durable.
No plugs, no charging breaks
A young intern in the office next door winds cables around a new coil. These coils will later be lowered underground in a box, connected to the grid and encased in magnetizing concrete. The recipient box looks similar; it’s another coil but smaller, and it will be mounted underneath the carriage of the vehicle. For a car, the battery box would be 25 by 25 centimeters (about 10 inches), for a scooter five by five centimeters (about two inches).
Esguerra pushes an electric scooter into a cemented scooter rack next to his office. The charging pad is invisible. A faint beep is the only sign that it has started charging. “Childs play!” Esguerra says. “Even when someone puts in the scooter a little crooked, the charge still works. Our efficiency rate is up to 96 percent.” From this summer on, hotel chains in Munich will try out this system with their rental scooters, at a price of about 500 Euros per charging station.
Compared to plug-in charging, Magment’s benefits include smaller batteries that charge slower and, therefore, gentler, so they may last longer. Nobody needs to plug in the vehicles manually anymore. “Personally, I’ve had an EV for six years,” Esguerra says, “and how often does it happen that I forgot to plug it in overnight and then start out with a low charge in the morning? Once people get used to the invisible charging system, it will become the norm.“
There are also downsides: Most car companies aren’t ready for the new technology. Hyundai is the first carmaker that announced plans to equip some new models with inductive charging capability. “How many cars are electrified worldwide?” Esguerra asks and gives the answer himself: “One percent. And how many forklifts are electrified? More than 70 percent!” Therefore, Magment focuses on charging forklifts, e-scooters and buses.

Magment has focused most of its efforts on charging forklifts and other vehicle types that are entirely or predominantly electric, unlike cars.
Magment
On the morning of my visit to Esguerra’s office, a developer of the world’s third-biggest forklift manufacturer is there to inspect how the technology works on the ground. In the basement, a Magment engineer drives an electric forklift over a testbed with invisible charging coils, turning on the green charging light. Esguerra opens the interior of the forklift and points out the two batteries. “With our system, the forklift will only need one battery.” The savings, about 7,000 Euro per forklift, will pay for the installation of Magment’s charging system in warehouses, Esguerra calculates. “Less personnel and no unnecessary wait times for charging will lead to further savings,” he says.
To implement the new technology as efficiently as possible, Magment engineers began recording the transport routes of forklifts in warehouses. “It looks like spaghetti diagrams,” Esguerra explains. “Soon you get the areas where the forklifts pass or wait most frequently. This is where you install the chargers underground.” The forklifts will charge while in use, without having to pause for charging breaks. The method could also work for robots, for instance, in warehouses and distribution centers.
Roads of the future could be electric
Potential disadvantages might become apparent once the technology is more broadly in use. Therefore investors were initially reluctant, Esguerra admits. “Some are eager to be the first but most prefer to wait until the technology has been extensively used in real life.”
A clear hurdle today is that electrifying entire freeways with induction coils would cost at least 1 to 1.5 million Euros per kilometer. The German Department for Transportation even calculates overall costs of 14 to 47 million Euros per kilometer. So, the technology may only make sense for areas where vehicles pass or dwell the longest, like the Oberhaching train station or a busy interstate toll booth.
And yet, Magment is ramping up to compete with other companies that build larger inductive charging pads. The company just finished the first 20 meters of a testbed in Indiana, in partnership with the Purdue University and the Indiana Department of Transportation. Magment is poised to build “the world’s first contactless wireless-charging concrete pavement highway segment,” Purdue University announced.
The project, part of Purdue’s ASPIRE (Advancing Sustainability through Powered Infrastructure for Roadway Electrification) program, is financed by the National Science Foundation. “Indiana is known as the Crossroads of America, and we’re committed to fortifying our position as a transportation leader by innovating to support the emerging vehicle technology,” Governor Eric J. Holcomb said. If testing is successful, including the concrete’s capacity to charge heavy trucks operating at higher power (200 kilowatts and above), Indiana plans to identify a highway segment to install Magment’s charging pads. The earliest would be 2023 at best.
In the meantime, buses in the Californian Antelope Valley, trams at Hollywood's Universal Studios and transit buses in Tampa, Florida, are already charging with inductive technology developed by Wave, a company spun out of Utah State University. In Michigan, Governor Gretchen Whitmer announced plans to build a test route for vehicles to charge while driving, in collaboration with the Israel-based company Electreon, and this year contracted to build the first road-based charging system in the U.S. The state is providing support through an innovative grant program.
Costs remain one of the biggest obstacles, but Esguerra’s vision includes the potential that toll roads could charge a premium for inductive charging capabilities. “And in reverse, a driver who has too much energy could feed his surplus into the grid while driving,” Esguerra dreams.
Meanwhile, Wave’s upcoming big projects are moving trucks along a route in Southern California and running a UPS route between Seattle and Portland. Wave CTO Michael Masquelier describes the inductive power transfer his company champions as “similar to a tuning fork. By vibrating that fork, you sent energy through the air and it is received by another tuning fork across the room. So it’s similar to that, but it’s magnetic energy versus sound energy.”
He hopes to partner with Magment, saying that “the magnetizing cement makes installation easier and improves the energy efficiency.” More research is needed to evaluate which company’s technology will prove to be the most efficient, practical, and cost-effective.
Esguerra’s vision includes the potential that toll roads could charge a premium for inductive charging capabilities. “And in reverse, a driver who has too much energy could feed his surplus into the grid while driving,” Esguerra dreams.
The future will soon arrive in the idyllic town of Bad Staffelstein, a quaint tourist destination in the Upper Franconia region of Germany. Visitors will be taken to and from the main station and the popular thermal bath by driverless shuttles. Together with the University of Wuppertal, the regional government of Upper Franconia wants to turn its district into “the center of autonomous driving.” Magment is about to install inductive charging pads at the shuttle stations and the thermal bath, eliminating the need for the shuttles to stop for charging times. No more drivers, no cable, no range anxiety. Masquelier believes that “wireless and autonomous driving go hand in hand.” Science fiction? It will become science reality in spring 2023.
CORRECTION: An earlier version of the story erroneously mentioned that Electreon required overhead cables.
Smartwatches can track COVID-19 symptoms, study finds
University of Michigan researchers found that new signals embedded in heart rate indicated when individuals were infected with COVID-19 and how ill they became.
If a COVID-19 infection develops, a wearable device may eventually be able to clue you in. A study at the University of Michigan found that a smartwatch can monitor how symptoms progress.
The study evaluated the effects of COVID-19 with various factors derived from heart-rate data. This method also could be employed to detect other diseases, such as influenza and the common cold, at home or when medical resources are limited, such as during a pandemic or in developing countries.
Tracking students and medical interns across the country, the University of Michigan researchers found that new signals embedded in heart rate indicated when individuals were infected with COVID-19 and how ill they became.
For instance, they discovered that individuals with COVID-19 experienced an increase in heart rate per step after the onset of their symptoms. Meanwhile, people who reported a cough as one of their COVID-19 symptoms had a much more elevated heart rate per step than those without a cough.
“We previously developed a variety of algorithms to analyze data from wearable devices. So, when the COVID-19 pandemic hit, it was only natural to apply some of these algorithms to see if we can get a better understanding of disease progression,” says Caleb Mayer, a doctoral student in mathematics at the University of Michigan and a co-first author of the study.
People may not internally sense COVID-19’s direct impact on the heart, but “heart rate is a vital sign that gives a picture of overall health," says Daniel Forger, a University of Michigan professor.
Millions of people are tracking their heart rate through wearable devices. This information is already generating a tremendous amount of data for researchers to analyze, says co-author Daniel Forger, professor of mathematics and research professor of computational medicine and bioinformatics at the University of Michigan.
“Heart rate is affected by many different physiological signals,” Forger explains. “For instance, if your lungs aren’t functioning properly, your heart may need to beat faster to meet metabolic demands. Your heart rate has a natural daily rhythm governed by internal biological clocks.” While people may not internally sense COVID-19’s direct impact on the heart, he adds that “heart rate is a vital sign that gives a picture of overall health.”
Among the total of 2,164 participants who enrolled in the student study, 72 undergraduate and graduate students contracted COVID-19, providing wearable data from 50 days before symptom onset to 14 days after. The researchers also analyzed this type of data for 43 medical interns from the Intern Health Study by the Michigan Neuroscience Institute and 29 individuals (who are not affiliated with the university) from the publicly available dataset.
Participants could wear the device on either wrist. They also documented their COVID-19 symptoms, such as fever, shortness of breath, cough, runny nose, vomiting, diarrhea, body aches, loss of taste, loss of smell, and sore throat.
Experts not involved in the study found the research to be productive. “This work is pioneering and reveals exciting new insights into the many important ways that we can derive clinically significant information about disease progression from consumer-grade wearable devices,” says Lisa A. Marsch, director of the Center for Technology and Behavioral Health and a professor in the Geisel School of Medicine at Dartmouth College. “Heart-rate data are among the highest-quality data that can be obtained via wearables.”
Beyond the heart, she adds, “Wearable devices are providing novel insights into individuals’ physiology and behavior in many health domains.” In particular, “this study beautifully illustrates how digital-health methodologies can markedly enhance our understanding of differences in individuals’ experience with disease and health.”
Previous studies had demonstrated that COVID-19 affects cardiovascular functions. Capitalizing on this knowledge, the University of Michigan endeavor took “a giant step forward,” says Gisele Oda, a researcher at the Institute of Biosciences at the University of Sao Paulo in Brazil and an expert in chronobiology—the science of biological rhythms. She commends the researchers for developing a complex algorithm that “could extract useful information beyond the established knowledge that heart rate increases and becomes more irregular in COVID patients.”
Wearable devices open the possibility of obtaining large-scale, long, continuous, and real-time heart-rate data on people performing everyday activities or while sleeping. “Importantly, the conceptual basis of this algorithm put circadian rhythms at the center stage,” Oda says, referring to the physical, mental, and behavioral changes that follow a 24-hour cycle. “What we knew before was often based on short-time heart rate measured at any time of day,” she adds, while noting that heart rate varies between day and night and also changes with activity.
However, without comparison to a control group of people having the common flu, it is difficult to determine if the heart-rate signals are unique to COVID-19 or also occur with other illnesses, says John Torous, an assistant professor of psychiatry at Harvard Medical School who has researched wearable devices. In addition, he points to recent data showing that many wearables, which work by beaming light through the skin, may be less accurate in people with darker skin due to variations in light absorption.
While the results sound interesting, they lack the level of conclusive evidence that would be needed to transform how physicians care for patients. “But it is a good step in learning more about what these wearables can tell us,” says Torous, who is also director of digital psychiatry at Beth Israel Deaconess Medical Center, a Harvard affiliate, in Boston. A follow-up step would entail replicating the results in a different pool of people to “help us realize the full value of this work.”
It is important to note that this research was conducted in university settings during the early phases of the pandemic, with remote learning in full swing amid strict isolation and quarantine mandates in effect. The findings demonstrate that physiological monitoring can be performed using consumer-grade wearable sensors, allowing research to continue without in-person contact, says Sung Won Choi, a professor of pediatrics at the University of Michigan who is principal investigator of the student study.
“The worldwide COVID-19 pandemic interrupted a lot of activities that relied on face-to-face interactions, including clinical research,” Choi says. “Mobile technology proved to be tremendously beneficial during that time, because it allowed us to collect detailed physiological data from research participants remotely over an entire semester.” In fact, the researchers did not have any in-person contact with the students involved in the study. “Everything was done virtually," Choi explains. "Importantly, their willingness to participate in research and share data during this historical time, combined with the capacity of secure cloud storage and novel mathematical analytics, enabled our research teams to identify unique patterns in heart-rate data associated with COVID-19.”

