Should egg and sperm donors reveal their identities? The debate pivots on genetics and medical history.

Cassandra Adams performs on stage at the Jersey City Theater Center in March 2019 to raise awareness about traumatic experiences that she and others have had with anonymous donor conception.
Until age 35, Cassandra Adams assumed her mother and father were her biological parents. Then she took saliva tests through two genealogy databases—23andMe and AncestryDNA—and discovered a discrepancy in her heritage. In bringing up the matter with her parents, she learned that fertility issues had led the couple to use a sperm donor.
“Most people my age were not told,” said Adams, now 40 and a stay-at-home mom in Jersey City, New Jersey, who is involved with donor-conception advocacy. “Even now, there’s still a lot of secrecy in the industry. There are still many parents who aren’t truthful or planning not to be truthful with their children.”
While some of those offspring may never know a significant part of their medical history, Adams is grateful that she does. Surprisingly, the DNA test revealed Jewish ancestry.
“There are a lot more genetic conditions that run in Jewish families, so it was really important that I get my medical history, because it’s very different from my dad who raised me,” said Adams, who has met her biological father and two of three known half-siblings. As a result of this experience, she converted to Judaism. “It has been a big journey,” she said.
In an era of advancing assisted reproduction technologies, genetics and medical history have become front and center of the debate as to whether or not egg and sperm donations should be anonymous – and whether secrecy is even possible in many cases.
Obstacles to staying anonymous
People looking to become parents can choose what’s called an “identity-release donor,” meaning their child can receive information about the donor when he or she turns 18. There’s no way to ensure that the donor will consent to a relationship at that time. Instead, if a relationship between the donor and child is a priority, parents may decide to use a known donor.
The majority of donors want to remain anonymous, said reproductive endocrinologist Robert Kiltz, founder and director of CNY Fertility in Syracuse, New York. “In general, egg and sperm donation is mostly anonymous, meaning the recipient doesn’t know the donor and the donor doesn’t know the recipient.”
Even if the donor isn’t disclosed, though, the mystery may become unraveled when a donor-conceived person undergoes direct-to-consumer genetic testing through ancestry databases, which are growing in number and popularity. These services offer DNA testing and links to relatives with identifiable information.
In the future, another obstacle to anonymity could be laws that prohibit anonymous sperm and egg donations, if they catch on. In June, Colorado became the first state in the nation to ban anonymous sperm and egg donations. The law, which takes effect in 2025, will give donor-conceived adults the legal authority to obtain their donor’s identity and medical history. It also requires banks that provide sperm and egg collection to keep current medical records and contact information for all donors. Meanwhile, it prohibits donations from those who won’t consent to identity disclosures.
“The tradition of anonymous sperm or egg donation has created a vast array of problems, most significantly that the people thus created want to know who their mommy and daddy are,” said Kenneth W. Goodman, professor and director of the Institute for Bioethics and Health Policy at the University of Miami Miller School of Medicine.
“There are counter arguments on both sides. But the current situation has led to great uncertainty and, in many cases, grief,” Goodman said.
Donors should bear some moral responsibility for their role in reproduction by allowing their identity to be disclosed to donor-conceived individuals when they turn 18, Goodman added, noting that “there are counter arguments on both sides. But the current situation has led to great uncertainty and, in many cases, grief.”
Adams, the Jersey City woman who learned she was Jewish, has channeled these feelings into several works of art and performances on stage at venues such as the Jersey City Theater Center. During these performances, she describes the trauma of “not knowing where we come from [or] who we look like.”
In the last five years, Kathleen “Casey” DiPaola, a lawyer in Albany, New York, who focuses her practice on adoption, assisted reproduction and surrogacy, has observed a big shift toward would-be parents looking to use known sperm donors. On the other hand, with egg donation, “I’m not seeing a whole lot of change,” she said. Compared to sperm donation, more medical screening is involved with egg donation, so donors are primarily found through fertility clinics and egg donor agencies that prefer anonymity. This leads to fewer options for prospective parents seeking an egg donor with disclosed identity, DiPaola said.
Some donors want to keep in touch
Rachel Lemmons, 32, who lives in Denver, grew interested in becoming an egg donor when, as a graduate student in environmental sciences, she saw an online advertisement. “It seemed like a good way to help pay off my student loan debt,” said Lemmons, who is married and has a daughter who will turn 2-years-old in December. She didn’t end up donating until many years later, after she’d paid off the debt. “The primary motivation at that point wasn’t financial,” she said. “Instead, it felt like a really wonderful way to help someone else have a family in a few weeks’ time.”
Lemmons originally donated anonymously because she didn’t know open donations existed. She was content with that until she became aware of donor-conceived individuals’ struggles. “It concerned me that I could potentially be contributing to this,” she said, adding that the egg donor and surrogacy agency and fertility clinic wouldn’t allow her to disclose her identity retroactively.
Since then, she has donated as an open donor, and kept in touch with the recipients through email and video calls. Knowing that they were finally able to have children is “incredibly rewarding,” Lemmons said.
When to tell the kids
Stanton Honig, professor of urology and division chief of sexual and reproductive medicine at Yale School of Medicine, said for years his team has recommended that couples using donor sperm inform children about the role of the donor and their identity. “Honesty is always the best policy, and it is likely that when they become of age, they might or will be able to find out about their biological sperm donor,” he said. “Hiding it creates more of a complicated situation for children in the long run.”
Amy Jones, a 45-year-old resident of Syracuse, N.Y., has three children, including twins, who know they were conceived with anonymous donor eggs from the same individual, so they share the same genetics. Jones, who is a registered nurse and asked for her real name not to be published, told them around age seven.
“The thought of using a known donor brought more concerns—what if she wanted my babies after they were born, or how would I feel if she treated them as her own every time I saw her?” said Jones.
“I did a lot of reading, and all psychologists said that it is best to start the conversation early,” she recalled. “They understood very little of what I was telling them, but through the years, I have brought it up in discussion and encouraged them to ask questions. To this day, they don't seem to be all that interested, but I expect that later on in life they may have more questions.”
Jones and her husband opted to use a donor because premature ovarian failure at age 27 had rendered her infertile. “The decision to use an egg donor was hard enough,” she said. “The thought of using a known donor brought more concerns—what if she wanted my babies after they were born, or how would I feel if she treated them as her own every time I saw her?”
Susan C. Klock, a clinical psychologist in the section of fertility and reproductive medicine at Northwestern University Feinberg School of Medicine, said, “Anonymity is virtually impossible in the age of direct-to-consumer genetic testing.” In addition, “selecting an identity-release donor is typically not the first thing parents are looking at when they select a donor. First and foremost, they are looking for a donor with a healthy medical background. Then they may consider donor characteristics that resemble the parents.”
The donor’s medical history can be critical
Donor agencies rely on the self-reported medical history of egg and sperm donors, which can lead to gaps in learning important information. Knowing a donor’s medical history may have led some families to make different or more well-informed choices.
After Steven Gunner, a donor-conceived adult, suffered from schizophrenia and died of a drug overdose at age 27 in 2020, his parents, who live in New York, learned of a potential genetic link to his mental illness. A website, Donor Sibling Registry, revealed that the sperm donor the couple had used, a college student at the time of donation, had been hospitalized during childhood for schizophrenia and died of a drug overdose at age 46. Gunner’s story inspired Steven’s Law, a bill that was introduced in Congress in July. If passed, it would mandate sperm banks to collect information on donors’ medical conditions, and donors would have to disclose medical information the banks weren’t able to find.
With limited exceptions, the U.S. Food and Drug Administration requires donors to be screened and tested for relevant communicable disease agents and diseases such as HIV, hepatitis viruses B and C, the Zika virus and several STDs. With current technology, it is also impossible to screen for thousands of rare genetic diseases. “If a couple is using IVF (in vitro fertilization) to conceive with the donor gamete, some may opt for pre-implantation genetic testing to assess for chromosomal abnormalities,” Klock said.
Even these precautions wouldn't cover every disease, and some would-be parents don't get the genetic screening. In a situation where one donor has a large number of offspring, it is concerning that he or she can spread a rare disease to multiple people, said Nick Isel, 37, of Yorkville, Illinois, who was conceived with donor sperm due to his parents’ fertility issues. They told him the truth when he was a teenager, and he found his biological father with a journalist’s help.
Since 2016, Isel, who owns a roofing company, has been petitioning the FDA to extend the retention of medical records, requiring the fertility establishment to maintain information on sperm and egg donors for 50 years instead of the current 10-year mandate.
“The lack of family health information,” he said, “is an ongoing, slow-motion public health crisis since donor conception began being regulated by the FDA as a practice.”
Tech-related injuries are becoming more common as many people depend on - and often develop addictions for - smart phones and computers.
In the 1990s, a mysterious virus spread throughout the Massachusetts Institute of Technology Artificial Intelligence Lab—or that’s what the scientists who worked there thought. More of them rubbed their aching forearms and massaged their cricked necks as new computers were introduced to the AI Lab on a floor-by-floor basis. They realized their musculoskeletal issues coincided with the arrival of these new computers—some of which were mounted high up on lab benches in awkward positions—and the hours spent typing on them.
Today, these injuries have become more common in a society awash with smart devices, sleek computers, and other gadgets. And we don’t just get hurt from typing on desktop computers; we’re massaging our sore wrists from hours of texting and Facetiming on phones, especially as they get bigger in size.
In 2007, the first iPhone measured 3.5-inches diagonally, a measurement known as the display size. That’s been nearly doubled by the newest iPhone 13 Pro, which has a 6.7-inch display. Other phones, too, like the Google Pixel 6 and the Samsung Galaxy S22, have bigger screens than their predecessors. Physical therapists and orthopedic surgeons have had to come up with names for a variety of new conditions: selfie elbow, tech neck, texting thumb. Orthopedic surgeon Sonya Sloan says she sees selfie elbow in younger kids and in women more often than men. She hears complaints related to technology once or twice a day.
The addictive quality of smartphones and social media means that people spend more time on their devices, which exacerbates injuries. According to Statista, 68 percent of those surveyed spent over three hours a day on their phone, and almost half spent five to six hours a day. Another report showed that people dedicate a third of their day to checking their phones, while the Media Effects Research Laboratory at Pennsylvania State University has found that bigger screens, ideal for entertainment purposes, immerse their users more than smaller screens. Oversized screens also provide easier navigation and more space for those with bigger hands or trouble seeing.
But others with conditions like arthritis can benefit from smaller phones. In March of 2016, Apple released the iPhone SE with a display size of 4.7 inches—an inch smaller than the iPhone 7, released that September. Apple has since come out with two more versions of the diminutive iPhone SE, one in 2020 and another in 2022.
These devices are now an inextricable part of our lives. So where does the burden of responsibility lie? Is it with consumers to adjust body positioning, get ergonomic workstations, and change habits to abate tech-related pain? Or should tech companies be held accountable?
Kavin Senapathy, a freelance science journalist, has the Google Pixel 6. She was drawn to the phone because Google marketed the Pixel 6’s camera as better at capturing different skin tones. But this phone boasts one of the largest display sizes on the market: 6.4 inches.
Senapathy was diagnosed with carpal and cubital tunnel syndromes in 2017 and fibromyalgia in 2019. She has had to create a curated ergonomic workplace setup, otherwise her wrists and hands get weak and tingly, and she’s had to adjust how she holds her phone to prevent pain flares.
Recently, Senapathy underwent an electromyography, or an EMG, in which doctors insert electrodes into muscles to measure their electrical activity. The electrical response of the muscles tells doctors whether the nerve cells and muscles are successfully communicating. Depending on her results, steroid shots and even surgery might be required. Senapathy wants to stick with her Pixel 6, but the pain she’s experiencing may push her to buy a smaller phone. Unfortunately, options for these modestly sized phones are more limited.
These devices are now an inextricable part of our lives. So where does the burden of responsibility lie? Is it with consumers like Senapathy to adjust body positioning, get ergonomic workstations, and change habits to abate tech-related pain? Or should tech companies be held accountable for creating addictive devices that lead to musculoskeletal injury?

Kavin Senapathy, a freelance journalist, bought the Google Pixel 6 because of its high-quality camera, but she’s had to adjust how she holds the oversized phone to prevent pain flares.
Kavin Senapathy
A one-size-fits-all mentality for smartphones will continue to lead to injuries because every user has different wants and needs. S. Shyam Sundar, the founder of Penn State’s lab on media effects and a communications professor, says the needs for mobility and portability conflict with the desire for greater visibility. “The best thing a company can do is offer different sizes,” he says.
Joanna Bryson, an AI ethics expert and professor at The Hertie School of Governance in Berlin, Germany, echoed these sentiments. “A lot of the lack of choice we see comes from the fact that the markets have consolidated so much,” she says. “We want to make sure there’s sufficient diversity [of products].”
Consumers can still maintain some control despite the ubiquity of tech. Sloan, the orthopedic surgeon, has to pester her son to change his body positioning when using his tablet. Our heads get heavier as they bend forward: at rest, they weigh 12 pounds, but bent 60 degrees, they weigh 60. “I have to tell him, ‘Raise your head, son!’” she says. It’s important, Sloan explains, to consider that growth and development will affect ligaments and bones in the neck, potentially making kids even more vulnerable to injuries from misusing gadgets. She recommends that parents limit their kids’ tech time to alleviate strain. She also suggested that tech companies implement a timer to remind us to change our body positioning.
In 2017, Nan-Wei Gong, a former contractor for Google, founded Figur8, which uses wearable trackers to measure muscle function and joint movement. It’s like physical therapy with biofeedback. “Each unique injury has a different biomarker,” says Gong. “With Figur8, you are comparing yourself to yourself.” This allows an individual to self-monitor for wear and tear and strengthen an injury in a way that’s efficient and designed for their body. Gong noticed that the work-from-home model during the COVID-19 pandemic created a new set of ergonomic problems that resulted in injuries. Figur8 provides real-time data for these injuries because “behavioral change requires feedback.”
Gong worked on a project called Jacquard while at Google. Textile experts weave conductive thread into their fabric, and the result is a patch of the fabric—like the cuff of a Levi’s jacket—that responds to commands on your smartphone. One swipe can call your partner or check the weather. It was designed with cyclists in mind who can’t easily check their phones, and it’s part of a growing movement in the tech industry to deliver creative, hands-free design. Gong thinks that engineers at large corporations like Google have accessibility in mind; it’s part of what drives their decisions for new products.
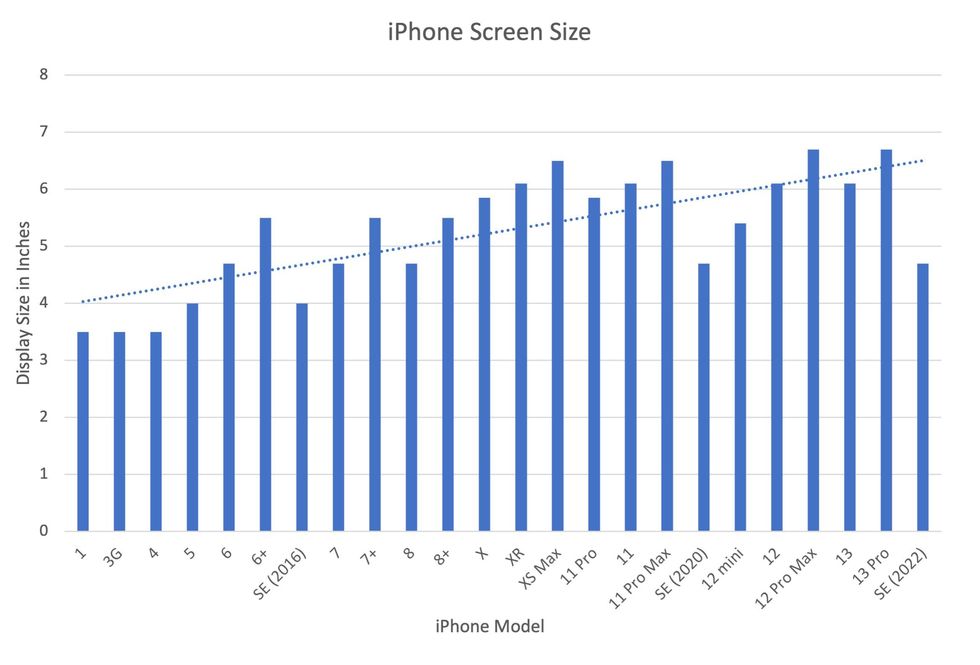
Display sizes of iPhones have become larger over time.
Sourced from Screenrant https://screenrant.com/iphone-apple-release-chronological-order-smartphone/ and Apple Tech Specs: https://www.apple.com/iphone-se/specs/
Back in Germany, Joanna Bryson reminds us that products like smartphones should adhere to best practices. These rules may be especially important for phones and other products with AI that are addictive. Disclosure, accountability, and regulation are important for AI, she says. “The correct balance will keep changing. But we have responsibilities and obligations to each other.” She was on an AI Ethics Council at Google, but the committee was disbanded after only one week due to issues with one of their members.
Bryson was upset about the Council’s dissolution but has faith that other regulatory bodies will prevail. OECD.AI, and international nonprofit, has drafted policies to regulate AI, which countries can sign and implement. “As of July 2021, 46 governments have adhered to the AI principles,” their website reads.
Sundar, the media effects professor, also directs Penn State’s Center for Socially Responsible AI. He says that inclusivity is a crucial aspect of social responsibility and how devices using AI are designed. “We have to go beyond first designing technologies and then making them accessible,” he says. “Instead, we should be considering the issues potentially faced by all different kinds of users before even designing them.”
Entomologist Jessica Ware is using new technologies to identify insect species in a changing climate. She shares her suggestions for how we can live harmoniously with creeper crawlers everywhere.
Jessica Ware is obsessed with bugs.
My guest today is a leading researcher on insects, the president of the Entomological Society of America and a curator at the American Museum of Natural History. Learn more about her here.
You may not think that insects and human health go hand-in-hand, but as Jessica makes clear, they’re closely related. A lot of people care about their health, and the health of other creatures on the planet, and the health of the planet itself, but researchers like Jessica are studying another thing we should be focusing on even more: how these seemingly separate areas are deeply entwined. (This is the theme of an upcoming event hosted by Leaps.org and the Aspen Institute.)
Listen to the Episode
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google

Entomologist Jessica Ware
D. Finnin / AMNH
Maybe it feels like a core human instinct to demonize bugs as gross. We seem to try to eradicate them in every way possible, whether that’s with poison, or getting out our blood thirst by stomping them whenever they creep and crawl into sight.
But where did our fear of bugs really come from? Jessica makes a compelling case that a lot of it is cultural, rather than in-born, and we should be following the lead of other cultures that have learned to live with and appreciate bugs.
The truth is that a healthy planet depends on insects. You may feel stung by that news if you hate bugs. Reality bites.
Jessica and I talk about whether learning to live with insects should include eating them and gene editing them so they don’t transmit viruses. She also tells me about her important research into using genomic tools to track bugs in the wild to figure out why and how we’ve lost 50 percent of the insect population since 1970 according to some estimates – bad news because the ecosystems that make up the planet heavily depend on insects. Jessica is leading the way to better understand what’s causing these declines in order to start reversing these trends to save the insects and to save ourselves.

