How 30 Years of Heart Surgeries Taught My Dad How to Live
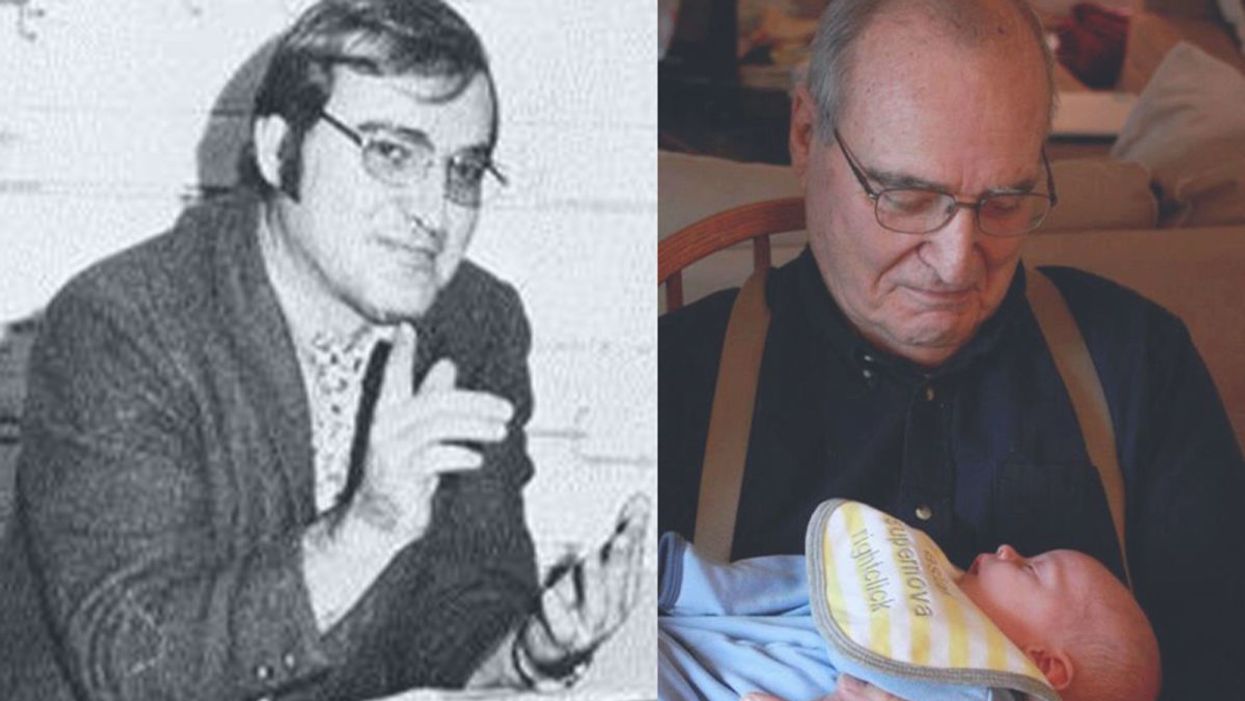
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
A Fierce Mother vs. a Fatal Mutation
Amber Salzman, whose determination to find a cure for her son's rare disease led to a recently successful clinical trial using gene therapy.
Editor's Note: In the year 2000, Amber Salzman was a 39-year-old mom from Philadelphia living a normal life: working as a pharmaceutical executive, raising an infant son, and enjoying time with her family. But when tragedy struck in the form of a ticking time bomb in her son's DNA, she sprang into action. Her staggering triumphs after years of turmoil exemplify how parents today can play a crucial role in pushing science forward. This is her family's story, as told to LeapsMag's Editor-in-Chief Kira Peikoff.
For a few years, my nephew Oliver, suffered from symptoms that first appeared as attention deficit disorder and then progressed to what seemed like Asperger's, and he continued to worsen and lose abilities he once had. After repeated misdiagnoses, he was finally diagnosed at age 8 with adrenoleukodystrophy, or ALD – a degenerative brain disease that puts kids on the path toward death. We learned it was an X-linked disease, so we had to test other family members. Because Oliver had it, that meant his mother, my sister, was carrier, which meant I had a 50-50 chance of being a carrier, and if I was, then my son had a 50-50 chance of getting the bad gene.
You know how some people win prizes all the time? I don't have that kind of luck. I had a sick feeling when we drew my son's blood. It was almost late December in the year 2000. Spencer was 1 and climbing around like a monkey, starting to talk—a very rambunctious kid. He tested positive, along with Oliver's younger brother, Elliott.
"The only treatment at the time was an allogenic stem cell transplant from cord blood or bone marrow."
You can imagine the dreadful things that go through your mind. Everything was fine then, but he had a horrific chance that in about 3 or 4 years, a bomb would go off. It was so tough thinking that we were going to lose Oliver, and then Spencer and Elliott were next in line. The only treatment at the time was an allogenic stem cell transplant from cord blood or bone marrow, which required finding a perfect match in a donor and then undergoing months of excruciating treatment. The mortality rate can be as high as 40 percent. If your kid was lucky enough to find a donor, he would then be lucky to leave the hospital 100 days after a transplant with a highly fragile immune system.
At the time, I was at GlaxoSmithKline in Research and Development, so I did have a background in working with drug development and I was fortunate to report to the chairman of R&D, Tachi Yamada.
I called Tachi and said, "I need your advice, I have three or four years to find a cure. What do I do?" He did some research and said it's a monogenic disease—meaning it's caused by only one errant gene—so my best bet was gene therapy. This is an approach to treatment that involves taking a sample of the patient's own stem cells, treating them outside the body with a viral vector as a kind of Trojan Horse to deliver the corrected gene, and then infusing the solution back into the patient, in the hopes that the good gene will proliferate throughout the body and stop the disease in its tracks.
Tachi said to call his friend Jim Wilson, who was a leader in the field at UPenn.
Since I live in Philadelphia I drove to see Jim as soon as possible. What I didn't realize was how difficult a time it was. This was shortly after Jesse Gelsinger died in a clinical trial for gene therapy run by UPenn—the first death for the field—and research had abruptly stopped. But when I met with Jim, he provided a road map for what it would take to put together a gene therapy trial for ALD.
Meanwhile, in parallel, I was dealing with my son's health.
After he was diagnosed, we arranged a brain MRI to see if he had any early lesions, because the only way you can stop the disease is if you provide a bone marrow transplant before the disease evolves. Once it is in full force, you can't reverse it, like a locomotive that's gone wild.
"He didn't recover like other kids because his brain was not a normal brain; it was an ALD brain."
We found he had a brain tumor that had nothing to do with ALD. It was slow growing, and we would have never found it otherwise until it was much bigger and caused symptoms. Long story short, he ended up getting the tumor removed, and when he was healing, he didn't recover like other kids because his brain was not a normal brain; it was an ALD brain. We knew we needed a transplant soon, and the gene therapy trial was unfortunately still years away.
At the time, he was my only child, and I was thinking of having additional kids. But I didn't want to get pregnant with another ALD kid and I wanted a kid who could provide a bone marrow transplant for my son. So while my son was still OK, I went through 5 cycles of in vitro fertilization, a process in which hormone shots stimulated my ovaries to produce multiple eggs, which were then surgically extracted and fertilized in a lab with my husband's sperm. After the embryos grew in a dish for three to five days, doctors used a technique called preimplantation genetic diagnosis, screening those embryos to determine which genes they carry, in order to try to find a match for Spencer. Any embryo that had ALD, we saved for research. Any that did not have ALD but were not a match for Spencer, we put in the freezer. We didn't end up with a single one that was a match.
So he had a transplant at Duke Children's Hospital at age 2, using cord blood donated from a public bank. He had to be in the hospital a long time, infusing meds multiple times a day to prevent the donor cells from rejecting his body. We were all excited when he made it out after 100 days, but then we quickly had to go back for an infection he caught.
We were still bent on moving forward with the gene therapy trials.
Jim Wilson at Penn explained what proof of concept we needed in animals to go forward to humans, and a neurologist in Paris, Patrick Aubourg, had already done that using a vector to treat ALD mice. But he wasn't sure which vector to use in humans.
The next step was to get Patrick and a team of gene therapy experts together to talk about what they knew, and what needed to be done to get a trial started. There was a lot of talk about viral vectors. Because viruses efficiently transport their own genomes into the cells they infect, they can be useful tools for sending good genes into faulty cells. With some sophisticated tinkering, molecular biologists can neuter normally dangerous viruses to make them into delivery trucks, nothing more. The biggest challenge we faced then was: How do we get a viral vector that would be safe in humans?
Jim introduced us to Inder Verma, chair of the scientific advisory board of Cell Genesys, a gene therapy company in California that was focused on oncology. They were the closest to making a viral vector that could go into humans, based on a disabled form of HIV. When I spoke to Inder, he said, "Let's review the data, but you will need to convince the company to give you the vector." So I called the CEO and basically asked him, "Would you be willing to use the vector in this horrific disease?" I told him that our trial would be the fastest way to test their vector in humans. He said, "If you can convince my scientists this is ready to go, we will put the vector forward." Mind you, this was a multi-million-dollar commitment, pro bono.
I kept thinking every day, the clock is ticking, we've got to move quickly. But we convinced the scientists and got the vector.
Then, before we could test it, an unrelated clinical trial in gene therapy for a severe immunodeficiency disease, led to several of the kids developing leukemia in 2003. The press did a bad number and scared everyone away from the field, and the FDA put studies on hold in the U.S. That was one of those moments where I thought it was over. But we couldn't let it stop. Nothing's an obstacle, just a little bump we have to overcome.
Patrick wanted to do the study in France with the vector. This is where patient advocacy is important in providing perspective on the risks vs. benefits of undergoing an experimental treatment. What nobody seemed to realize was that the kids in the 2003 trial would have died if they were not first given the gene therapy, and luckily their leukemia was a treatable side effect.
Patrick and I refused to give up pushing for approval of the trial in France. Meanwhile, I was still at GSK, working full time, and doing this at night, nonstop. Because my day job did require travel to Europe, I would stop by Paris and meet with him. Another sister of mine who did not have any affected children was a key help and we kept everything going. You really need to continually stay engaged and press the agenda forward, since there are so many things that pop up that can derail the program.
Finally, Patrick was able to treat four boys with the donated vector. The science paper came out in 2009. It was a big deal. That's when the venture money came in—Third Rock Ventures was the first firm to put big money behind gene therapy. They did a deal with Patrick to get access to the Intellectual Property to advance the trial, brought on scientists to continue the study, and made some improvements to the vector. That's what led to the new study reported recently in the New England Journal of Medicine. Of 17 patients, 15 of them are still fine at least two years after treatment.
You know how I said we felt thrilled that my son could leave the hospital after 100 days? When doing the gene therapy treatment, the hospital stay needed is much quicker. Shortly after one kid was treated, a physician in the hospital remarked, "He is fine, he's only here because of the trial." Since you get your own cells, there is no risk of graft vs. host disease. The treatment is pretty anticlimactic: a bag of blood, intravenously infused. You can bounce back within a few weeks.
Now, a few years out, approximately 20 percent of patients' cells have been corrected—and that's enough to hold off the disease. That's what the data is showing. I was blown away when it worked in the first two patients.
The formerly struggling field is now making a dramatic comeback.
Just last month, the first two treatments involving gene therapy were approved by the FDA to treat a devastating type of leukemia in children and an aggressive blood cancer in adults.
Now I run a company, Adverum Biotechnologies, that I wish existed back when my son was diagnosed, because I want people who are like me, coming to me, saying: "I have proof of concept in an animal, I need to get a vector suitable for human trials, do the work needed to file with the FDA, and move it into humans." Our company knows how to do that and would like to work with such patient advocates.
Often parents feel daunted to partake in similar efforts, telling me, "Well, you worked in pharma." Yes, I had advantages, but if you don't take no for an answer, people will help you. Everybody is one degree of separation from people who can help them. You don't need a science or business background. Just be motivated, ask for help, and have your heart in the right place.
Having said that, I don't want to sound judgmental of families who are completely paralyzed. When you get a diagnosis that your child is dying, it is hard to get out of bed in the morning and face life. My sister at a certain point had one child dying, one in the hospital getting a transplant, and a healthy younger child. To expect someone like that to at the same time be flying to an FDA meeting, it's hard. Yet, she made critical meetings, and she and her husband graciously made themselves available to talk to parents of recently diagnosed boys. But it is really tough and my heart goes out to anyone who has to live through such devastation.
Tragically, my nephew Oliver passed away 13 years ago at age 12. My other nephew was 8 when he had a cord blood transplant; our trial wasn't available yet. He had some bad graft vs. host disease and he is now navigating life using a wheelchair, but thank goodness, it stopped the disease. He graduated Stanford a year ago and is now a sports writer for the Houston Chronicle.
As for my son, today he is 17, a precocious teenager applying to colleges. He also volunteers for an organization called the Friendship Circle, providing friends for kids with special needs. He doesn't focus on disability and accepts people for who they are – maybe he would have been like that anyway, but it's part of who he is. He lost his cousin and knows he is alive today because Oliver's diagnosis gave us a head start on his.
My son's story is a good one in that he had a successful transplant and recovered.
Once we knew he would make it and we no longer needed our next child to be a match, we had a daughter using one of our healthy IVF embryos in storage. She is 14 now, but she jokes that she is technically 17, so she should get to drive. I tell her, they don't count the years in the freezer. You have to joke about it.
I am so lucky to have two healthy kids today based on advances in science.
And I often think of Oliver. We always try to make him proud and honor his name.
[Editor's Note: This story was originally published in November 2017. We are resurfacing archive hits while our staff is on vacation.]

Salzman and her son Spencer, 17, who is now healthy.
(Courtesy of Salzman)
So-Called “Puppy Mills” Are Not All As Bad As We Think, Pioneering Research Suggests
New research challenges the popular notion that all commercial breeding kennels are inhumane.
Candace Croney joined the faculty at Purdue University in 2011, thinking her job would focus on the welfare of livestock and poultry in Indiana. With bachelor's, master's, and doctoral degrees in animal sciences, her work until then had centered on sheep, cattle, and pigs. She'd even had the esteemed animal behaviorist Temple Grandin help shape her master's research project.
Croney's research has become the first of its kind in the world—and it's challenging our understanding of how dog breeding is being done.
Then came an email from a new colleague asking Croney to discuss animal welfare with some of Indiana's commercial dog breeders, the kind who produce large quantities of puppies for sale in pet stores.
"I didn't even know the term commercial breeders," Croney says. "I'd heard the term 'puppy millers.' That's pretty much what I knew."
She went to the first few kennels and braced herself for an upsetting experience. She's a dog lover who has fostered shelter mutts and owned one, and she'd seen the stories: large-scale breeders being called cruel and evil, lawmakers trying to ban the sale of commercially bred puppies, and constant encouragement to rescue a dog instead of paying into a greedy, heartless "puppy mill" industry.
But when she got to the kennels, she was surprised. While she encountered a number of things she didn't like about the infrastructure at the older facilities—a lack of ventilation, a lot of noise, bad smells—most of the dogs themselves were clean. The majority didn't have physical problems. No open sores. No battered bodies. Nothing like what she'd seen online.
But still, the way the dogs acted gave her pause.
"Things were, in many regards, better than I thought they would be," Croney says. "Google told me the dogs would be physically a mess, and they weren't, but behaviorally, things were jumping out at me."
While she did note that some of the breeders had play yards for their pups, a number of the dogs feared new people and things like leashes because they hadn't been exposed to enough of them. Some of the dogs also seemed to lack adequate toys, activities, and games to keep them mentally and physically stimulated.
But she was there strictly as a representative of the university to ask questions and offer feedback, no more or less. A few times, she says, she felt like the breeders wanted her to endorse what they were doing, "and I immediately got my back up about that. I did not want my name used to validate things that I could tell I didn't agree with. It was uncomfortable from that perspective."
After sharing the animal-welfare information her colleague had requested, Croney figured that was that. She never expected to be in a commercial kennel again. But six months later, her phone rang. Some of the people she'd met were involved in legislative lobbying, and they were trying to write welfare standards for Indiana's commercial breeders to follow.
In the continuing battle over what is, and is not, a "puppy mill," they wanted somebody with a strong research background to set a baseline standard, somebody who would actually bring objectivity to the breeder-activist conflict without being on one side or the other.
In other words, they wanted Croney's help to figure out not only appropriate enclosure sizes, but also requirements for socialization and enrichment activities—stimulation she knew the dogs desperately needed.
"I thought, crap, how am I not going to help?" she recalls. "And they said, 'Well how long will that take? A couple of weeks? A month?'"

Dr. Croney with Theo, whom she calls "a beloved family member of our research team."
(Photo credit: Purdue University/Vincent Walter)
Six years later, Croney's research remains ongoing. It has become the first of its kind in the world—and it's challenging our understanding of how dog breeding is being done, and how it could and should be done for years to come.
How We Got Here
Americans have been breeding pet dogs in large-scale kennels since World War II. The federal standard that regulates those kennels is the Animal Welfare Act, which President Johnson signed into law in 1966. Back then, people thought it was OK to treat dogs a lot differently than they do today. The law has been updated, but it still allows a dog the size of a Beagle to be kept in a cage the size of a dishwasher all day, every day because for some dogs, when the law was written, having a cage that size meant an improvement in living conditions.
Countless commercial breeders, who are regularly inspected under the Animal Welfare Act, have long believed that as long as they followed the law, they were doing things right. And they've seen sales for their puppies go up and up over the years. About 38 percent of U.S. households now own one or more dogs, the highest rate since the American Veterinary Medical Association began measuring the statistic in 1982.
Consumers now demand eight million dogs per year, which has reinforced breeders' beliefs that despite what activists shout at protests, the breeders are actually running businesses the public supports. As one Ohio commercial breeder—long decried by activists as a "puppy mill" owner—told The Washington Post in 2016, "This is a customer-driven industry. If we weren't satisfying the customer, we'd starve to death. I've never seen prices like the ones we're seeing now, in my whole career."
That breeder, though, is also among leading industry voices who say they understand that public perception of what's acceptable and what's not in a breeding kennel has changed. Regardless of what the laws are, they say, kennels must change along with the public's wishes if the commercial breeding industry is going to survive. The question is how, exactly, to move from the past to the future, at a time when demands for change have reached a fever pitch.
"The Animal Welfare Act, that was gospel. It meant you were taking care of dogs," says Bob Vetere, former head of the American Pet Products Association and now chairman of the Pet Leadership Council. "That was, what, 40 years ago? Things have evolved. People understand much more since then—and back then, there were maybe 20 million dogs in the country. Now, there's 90 million. It's that dramatic. People love their dogs, and everybody is going to get one."
Vetere became an early supporter of Croney's research, which, unbelievably, became the first ever to focus on what it actually means to run a good commercial breeding kennel. At the start of her research, Croney found that the scientific literature underpinning many existing laws and opinions was not just lacking, but outright nonexistent.
"We kept finding it over and over," she says of the literature gaps, citing common but uninformed beliefs about appropriate kennel size as just one example. "I can't find any research about how much space they're supposed to have. People said, 'Yeah, we had a meeting and a bunch of people made some recommendations.'"
She started filling in the research gaps with her team at Purdue, building relationships with dog breeders until she had more than 100 kennels letting her methodically figure out what was actually working for the dogs.
"The measurable successes in animal welfare over the past 50 years began from a foundation in science."
Creating Standards from Scratch
Other industry players soon took notice. One was Ed Sayres, who had served as CEO of the ASPCA for nearly a decade before turning his attention to lobbying efforts regarding the "puppy mill" issue. He recognized that what Croney was doing for commercial breeding mirrored the early work researchers started a half-century ago in the effort that led to better shelters all across America today.
"The measurable successes in animal welfare over the past 50 years began from a foundation in science," Sayres says. "Whether it was the transition to more humane euthanasia methods or how to manage dog and cat overpopulation, we found success from rigorous examination of facts and emerging science."
Sayres, Vetere, and others began pushing for the industry to support Croney's work, moving the goalposts beyond Indiana to the entire United States.
"If you don't have commercial breeding, you have people importing dogs from overseas with no restrictions, or farming in their backyards to make money," Vetere says. "You need commercial breeders with standards—and that's what Candace is trying to create, those standards."
Croney ended up with a $900,000 grant from three industry organizations: the World Pet Association, Pet Food Institute, and the Pet Industry Joint Advisory Council. With their support, she created a nationwide program called Canine Care Certified, like a Good Housekeeping Seal of Approval for a kennel. The program focuses on outcome-based standards, meaning she looks at what the dogs tell her about how well they are doing through their health and behavior. For the most part, beyond baseline requirements, the program lets a breeder achieve those goals in whatever ways work for the dogs.
The approach is different from many legislative efforts, with laws stating a cage must be made three feet larger to be considered humane. Instead, Croney walks through kennels with breeders and points out, for instance, which puppies in a litter seem to be shy or fearful, and then teaches the breeders how to give those puppies better socialization. She helps the breeders find ways to introduce dogs to strangers and objects like umbrellas that may not be part of regular kennel life, but will need to become familiar when the breeding dog retires and gets adopted into a home as a pet. She helps breeders understand that dogs need mental as well as physical stimulation, whether it comes from playing with balls and toys or running up and down slides.
The breeders can't learn fast enough, Croney says, and she remains stunned at how they constantly ask for more information—an attitude that made her stop using the term "puppy mill" to describe them at all.
"Now, full disclosure: Given that all of these kennels had volunteered, the odds were that we were seeing a skewed population, and that it skewed positive," she says. "But if you read what was in the media at the time, we shouldn't have been able to find any. We're told that all these kennels are terrible. Clearly, it was possible to get a positive outcome."
To Buy or Not to Buy?
Today, she says, she's shocked at how quickly some of the kennels have improved. Facilities that appalled her at first sight now have dogs greeting people with wagging tails.
"Not only would I get a dog from them, but would I put my dog there in that kennel temporarily? Yeah, I would."
"The most horrifying thing I learned was that some of these people weren't doing what I'd like to see, not because they didn't care or only wanted money, but because nobody had ever told them," she says. "As it turned out, they didn't know any different, and no one would help them."
For Americans who want to know whether it's OK to get a commercially bred puppy, Croney says she thinks about her own dogs. When she started working with the breeders, there were plenty of kennels that, she says, she would not have wanted to patronize. But now she's changing her mind about more and more of them.
"I'm just speaking as somebody who loves dogs and wants to make sure I'm not subsidizing anything inhumane or cruel," she says. "Not only would I get a dog from them, but would I put my dog there in that kennel temporarily? Yeah, I would."
She says the most important thing is for consumers to find out how a pup was raised, and how the pup's parents were raised. As with most industries, commercial breeders run the gamut, from barely legal to above and beyond.
Not everyone agrees with Croney's take on the situation, or with her approach to improving commercial breeding kennels. In its publication "Puppy Mills and the Animal Welfare Act," the Humane Society of the United States writes that while Croney's Canine Care Certified program supports "common areas of agreement" with animal-welfare lobbyists, her work has been funded by the pet industry—suggesting that it's impure—and a voluntary program is not enough to incentivize breeders to improve.
New laws, the Humane Society states, must be enacted to impose change: "Many commercial dog breeding operators will not raise their standards voluntarily, and even if they were to agree to do so it is not clear whether there would be any independent mechanism for enforcement or transparency for the public's sake. ... The logical conclusion is that improved standards must be codified."
Croney says that type of attitude has long created resentment between breeders and animal-welfare activists, as opposed to actual kennel improvements. Both sides have a point; for years, there have been examples of bottom-of-the-barrel kennels that changed their ways or shut down only after regulators smacked them with violations, or after lawmakers raised operating standards in ways that required improvements for the kennels to remain legally in business.
At the same time, though, powerful organizations including the Humane Society—which had revenue of more than $165 million in 2018 alone—have routinely pushed for bans on stores that sell commercially bred puppies, and have decried "puppy mills" in marketing and fund-raising literature, without offering financial grants or educational programs to kennels that are willing to improve.
Croney believes that the reflexive demonization of all commercial breeders is a mistake. Change is more effective, she says, when breeders "want to do better, want to learn, want to grow, and you treat them as advocates and allies in doing something good for animal welfare, as opposed to treating them like they're your enemies."
"If you're watching undercover videos about people treating animals in bad ways, I'm telling you, change is happening."
She adds that anyone who says all commercial breeders are "puppy mills" needs to take a look at the kennels she's seen and the changes her work has brought—and is continuing to bring.
"The ones we work with are working really, really hard to improve and open their doors so that if somebody wants to get a dog from them, they can be assured that those dogs were treated with a level of care and compassion that wasn't there five or 10 years ago, but that is there now and will be better in a year and will be much better in five years," she says. "If you're watching undercover videos about people treating animals in bad ways, I'm telling you, change is happening. It is so much better than people realize, and it continues to get even better yet."

