How 30 Years of Heart Surgeries Taught My Dad How to Live
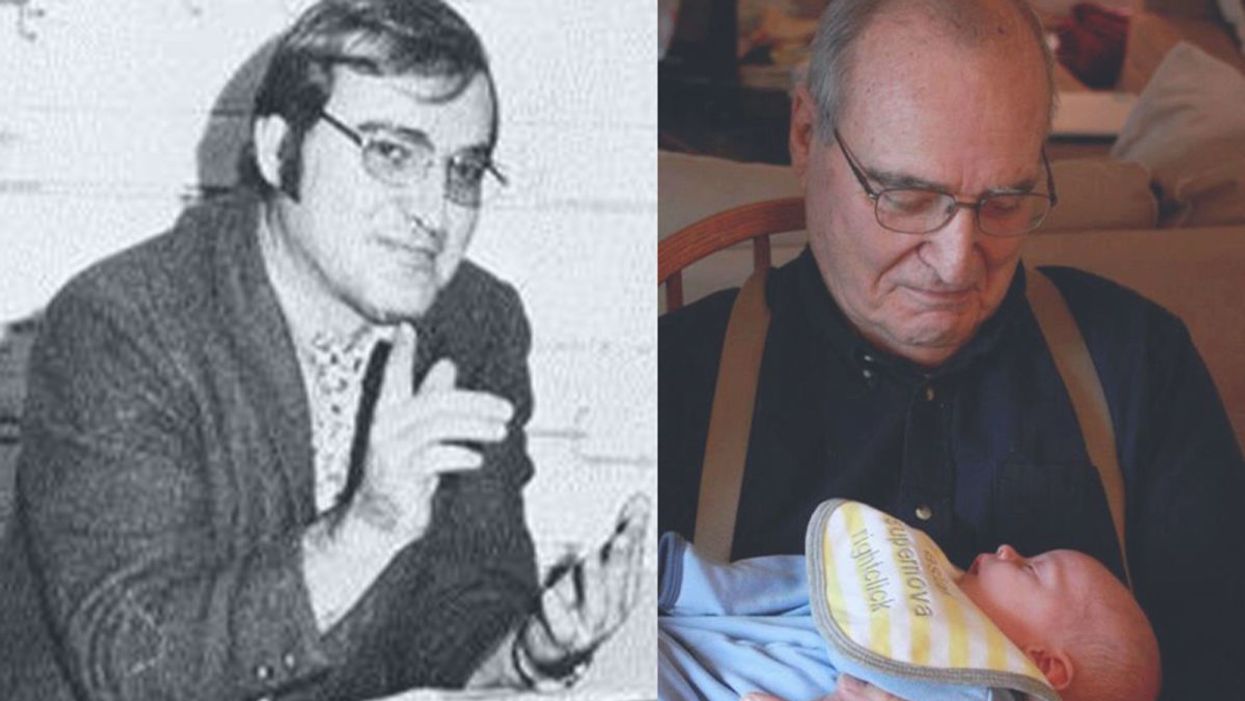
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
Can tech help prevent the insect apocalypse?
Declining numbers of insects, coupled with climate change, can have devastating effects for people in more ways than one. But clever use of technologies like AI could keep them buzzing.
This article originally appeared in One Health/One Planet, a single-issue magazine that explores how climate change and other environmental shifts are making us more vulnerable to infectious diseases by land and by sea - and how scientists are working on solutions.
On a warm summer day, forests, meadows, and riverbanks should be abuzz with insects—from butterflies to beetles and bees. But bugs aren’t as abundant as they used to be, and that’s not a plus for people and the planet, scientists say. The declining numbers of insects, coupled with climate change, can have devastating effects for people in more ways than one. “Insects have been around for a very long time and can live well without humans, but humans cannot live without insects and the many services they provide to us,” says Philipp Lehmann, a researcher in the Department of Zoology at Stockholm University in Sweden. Their decline is not just bad, Lehmann adds. “It’s devastating news for humans.
”Insects and other invertebrates are the most diverse organisms on the planet. They fill most niches in terrestrial and aquatic environments and drive ecosystem functions. Many insects are also economically vital because they pollinate crops that humans depend on for food, including cereals, vegetables, fruits, and nuts. A paper published in PNAS notes that insects alone are worth more than $70 billion a year to the U.S. economy. In places where pollinators like honeybees are in decline, farmers now buy them from rearing facilities at steep prices rather than relying on “Mother Nature.”
And because many insects serve as food for other species—bats, birds and freshwater fish—they’re an integral part of the ecosystem’s food chain. “If you like to eat good food, you should thank an insect,” says Scott Hoffman Black, an ecologist and executive director of the Xerces Society for Invertebrate Conservation in Portland, Oregon. “And if you like birds in your trees and fish in your streams, you should be concerned with insect conservation.”
Deforestation, urbanization, and agricultural spread have eaten away at large swaths of insect habitat. The increasingly poorly controlled use of insecticides, which harms unintended species, and the proliferation of invasive insect species that disrupt native ecosystems compound the problem.
“There is not a single reason why insects are in decline,” says Jessica L. Ware, associate curator in the Division of Invertebrate Zoology at the American Museum of Natural History in New York, and president of the Entomological Society of America. “There are over one million described insect species, occupying different niches and responding to environmental stressors in different ways.”

Jessica Ware, an entomologist at the American Museum of Natural History, is using DNA methods to monitor insects.
Credit:D.Finnin/AMNH
In addition to habitat loss fueling the decline in insect populations, the other “major drivers” Ware identified are invasive species, climate change, pollution, and fluctuating levels of nitrogen, which play a major role in the lifecycle of plants, some of which serve as insect habitants and others as their food. “The causes of world insect population declines are, unfortunately, very easy to link to human activities,” Lehmann says.
Climate change will undoubtedly make the problem worse. “As temperatures start to rise, it can essentially make it too hot for some insects to survive,” says Emily McDermott, an assistant professor in the Department of Entomology and Plant Pathology at the University of Arkansas. “Conversely in other areas, it could potentially also allow other insects to expand their ranges.”
Without Pollinators Humans Will Starve
We may not think much of our planet’s getting warmer by only one degree Celsius, but it can spell catastrophe for many insects, plants, and animals, because it’s often accompanied by less rainfall. “Changes in precipitation patterns will have cascading consequences across the tree of life,” says David Wagner, a professor of ecology and evolutionary biology at the University of Connecticut. Insects, in particular, are “very vulnerable” because “they’re small and susceptible to drying.”
For instance, droughts have put the monarch butterfly at risk of being unable to find nectar to “recharge its engine” as it migrates from Canada and New England to Mexico for winter, where it enters a hibernation state until it journeys back in the spring. “The monarch is an iconic and a much-loved insect,” whose migration “is imperiled by climate change,” Wagner says.
Warming and drying trends in the Western United States are perhaps having an even more severe impact on insects than in the eastern region. As a result, “we are seeing fewer individual butterflies per year,” says Matt Forister, a professor of insect ecology at the University of Nevada, Reno.
There are hundreds of butterfly species in the United States and thousands in the world. They are pollinators and can serve as good indicators of other species’ health. “Although butterflies are only one group among many important pollinators, in general we assume that what’s bad for butterflies is probably bad for other insects,” says Forister, whose research focuses on butterflies. Climate change and habitat destruction are wreaking havoc on butterflies as well as plants, leading to a further indirect effect on caterpillars and butterflies.
Different insect species have different levels of sensitivity to environmental changes. For example, one-half of the bumblebee species in the United States are showing declines, whereas the other half are not, says Christina Grozinger, a professor of entomology at the Pennsylvania State University. Some species of bumble bees are even increasing in their range, seemingly resilient to environmental changes. But other pollinators are dwindling to the point that farmers have to buy from the rearing facilities, which is the case for the California almond industry. “This is a massive cost to the farmer, which could be provided for free, in case the local habitats supported these pollinators,” Lehmann says.
For bees and other insects, climate change can harm the plants they depend on for survival or have a negative impact on the insects directly. Overly rainy and hot conditions may limit flowering in plants or reduce the ability of a pollinator to forage and feed, which then decreases their reproductive success, resulting in dwindling populations, Grozinger explains.
“Nutritional deprivation can also make pollinators more sensitive to viruses and parasites and therefore cause disease spread,” she says. “There are many ways that climate change can reduce our pollinator populations and make it more difficult to grow the many fruit, vegetable and nut crops that depend on pollinators.”
Disease-Causing Insects Can Bring More Outbreaks
While some much-needed insects are declining, certain disease-causing species may be spreading and proliferating, which is another reason for human concern. Many mosquito types spread malaria, Zika virus, West Nile virus, and a brain infection called equine encephalitis, along with other diseases as well as heartworms in dogs, says Michael Sabourin, president of the Vermont Entomological Society. An animal health specialist for the state, Sabourin conducts vector surveys that identify ticks and mosquitoes.
Scientists refer to disease-carrying insects as vector species and, while there’s a limited number of them, many of these infections can be deadly. Fleas were a well-known vector for the bubonic plague, while kissing bugs are a vector for Chagas disease, a potentially life-threatening parasitic illness in humans, dogs, and other mammals, Sabourin says.
As the planet heats up, some of the creepy crawlers are able to survive milder winters or move up north. Warmer temperatures and a shorter snow season have spawned an increasing abundance of ticks in Maine, including the blacklegged tick (Ixodes scapularis), known to transmit Lyme disease, says Sean Birkel, an assistant professor in the Climate Change Institute and Cooperative Extension at the University of Maine.
Coupled with more frequent and heavier precipitation, rising temperatures bring a longer warm season that can also lead to a longer period of mosquito activity. “While other factors may be at play, climate change affects important underlying conditions that can, in turn, facilitate the spread of vector-borne disease,” Birkel says.
For example, if mosquitoes are finding fewer of their preferred food sources, they may bite humans more. Both male and female mosquitoes feed on sugar as part of their normal behavior, but if they aren’t eating their fill, they may become more bloodthirsty. One recent paper found that sugar-deprived Anopheles gambiae females go for larger blood meals to stay in good health and lay eggs. “More blood meals equals more chances to pick up and transmit a pathogen,” McDermott says, He adds that climate change could reduce the number of available plants to feed on. And while most mosquitoes are “generalist sugar-feeders” meaning that they will likely find alternatives, losing their favorite plants can make them hungrier for blood.
Similar to the effect of losing plants, mosquitoes may get turned onto people if they lose their favorite animal species. For example, some studies found that Culex pipiens mosquitoes that transmit the West Nile virus feed primarily on birds in summer. But that changes in the fall, at least in some places. Because there are fewer birds around, C. pipiens switch to mammals, including humans. And if some disease-carrying insect species proliferate or increase their ranges, that increases chances for human infection, says McDermott. “A larger concern is that climate change could increase vector population sizes, making it more likely that people or animals would be bitten by an infected insect.”
Science Can Help Bring Back the Buzz
To help friendly insects thrive and keep the foes in check, scientists need better ways of trapping, counting, and monitoring insects. It’s not an easy job, but artificial intelligence and molecular methods can help. Ware’s lab uses various environmental DNA methods to monitor freshwater habitats. Molecular technologies hold much promise. The so-called DNA barcodes, in which species are identified using a short string of their genes, can now be used to identify birds, bees, moths and other creatures, and should be used on a larger scale, says Wagner, the University of Connecticut professor. “One day, something akin to Star Trek’s tricorder will soon be on sale down at the local science store.”
Scientists are also deploying artificial intelligence, or AI, to identify insects in agricultural systems and north latitudes where there are fewer bugs, Wagner says. For instance, some automated traps already use the wingbeat frequencies of mosquitoes to distinguish the harmless ones from the disease-carriers. But new technology and software are needed to further expand detection based on vision, sound, and odors.
“Because of their ubiquity, enormity of numbers, and seemingly boundless diversity, we desperately need to develop molecular and AI technologies that will allow us to automate sampling and identification,” says Wagner. “That would accelerate our ability to track insect populations, alert us to the presence of new disease vectors, exotic pest introductions, and unexpected declines.”
Your surgery could harm yourself and the planet. Here's what some doctors are doing about it.
Certain gases used for anesthesia are 3,000 times more damaging for the climate than CO2. Some anesthesiologists are pointing to other solutions.
This is part 1 of a three part series on a new generation of doctors leading the charge to make the health care industry more sustainable - for the benefit of their patients and the planet. Read part 2 here and part 3 here.
Susanne Koch, an anesthesiologist and neurologist, reached a pivot point when she was up to her neck in water, almost literally. The basement of her house in Berlin had flooded in the summer of 2018, when Berlin was pummeled by unusually strong rains. After she drained the house, “I wanted to dig into facts, to understand how exactly these extreme weather events are related to climate change,” she says.
Studying the scientific literature, she realized how urgent the climate crisis is, but the biggest shock was to learn that her profession contributed substantially to the problem: Inhalation gases used during medical procedures are among the most damaging greenhouse gases. Some inhalation gases are 3,000 times more damaging for the climate than CO2, Koch discovered. “Spending seven hours in the surgery room is the equivalent of driving a car for four days nonstop,” she says. Her job of helping people at Europe’s largest university hospital, the Charité in Berlin, was inadvertently damaging both the people and the planet.
“Nobody had ever even mentioned a word about that during my training,” Koch says.
On the whole, the medical sector is responsible for a disproportionally large percentage of greenhouse gas emissions, with the U.S. as the biggest culprit. According to a key paper published in 2020 in Health Affairs, the health industry “is among the most carbon-intensive service sectors in the industrialized world,” accounting for between 4.4 percent and 4.6 percent of greenhouse gas emissions. “It’s not just anesthesia but health care that has a problem,” says Jodi Sherman, anesthesiology professor and Medical Director of the Program on Healthcare Environmental Sustainability at Yale University as well as co-director of the Lancet Planetary Health Commission on Sustainable Healthcare. In the U.S., health care greenhouse gas emissions make up about 8.5 percent of domestic greenhouse gas emissions. They rose 6 percent from 2010 to 2018, to nearly 1,700 kilograms per person, more than in any other nation.
Of course, patients worry primarily about safety, not sustainability. Yet, Koch emphasizes that “as doctors, we have the responsibility to do no harm, and this includes making sure that we use resources as sustainably as possible.” Studies show that 2018 greenhouse gas and toxic air pollutant emissions resulted in the loss of 388,000 disability-adjusted life years in the U.S. alone. “Disease burden from health care pollution is of the same order of magnitude as deaths from preventable medical errors, and should be taken just as seriously,” Sherman cautions.
When Koch, the anesthesiologist, started discussing sustainable options with colleagues, the topic was immediately met with plenty of interest. Her experience is consistent with the latest representative poll of the nonprofit Foundation Health in Germany. Nine out of ten doctors were interested in urgently finding sustainable solutions for medical services but lacked knowhow and resources. For teaching purposes, Sherman and her team have developed the Yale Gassing Greener app that allows anesthesiologists to compare how much pollution they can avoid through choosing different anesthesia methods. Sherman also published professional guidelines intended to help her colleagues better understand how various methods affect carbon emissions.
Significant traces of inhalation gases have been found in Antarctica and the Himalayas, far from the vast majority of surgery rooms.
A solution espoused by both Sherman and Koch is comparatively simple: They stopped using desflurane, which is by far the most damaging of all inhalation gases to the climate. Its greenhouse effect is 2,590 times stronger than carbon dioxide. The Yale New Haven Hospital already stopped using desflurane in 2013, becoming the first known healthcare organization to eliminate a drug based on environmental grounds. Sherman points out that this resulted in saving more than $1.2 million in costs and 1,600 tons of CO2 equivalents, about the same as the exhaust from 360 passenger vehicles per year.
At the Charité, Koch claims that switching to other anesthesiology choices, such as propofol, has eliminated 90 percent of the climate gas emissions in the anesthesiology department since 2016. Young anesthesiologists are still taught to use desflurane as the standard because desflurane is absorbed less into the patients’ bodies, and they wake up faster. However, Koch who has worked as an anesthesiologist since 2006, says that with a little bit of experience, you can learn when to stop giving the propofol so it's timed just as well with a person’s wake-up process. In addition, “patients are less likely to feel nauseous after being given propofol,” Koch says. Intravenous drugs might require more skill, she adds, "but there is nothing unique to the drug desflurane that cannot be accomplished with other medications.”
Desflurane isn’t the only gas to be concerned about. Nitrous oxide is the second most damaging because it’s extremely long-lived in the environment, and it depletes the ozone layer. Climate-conscious anesthesiologists are phasing out this gas, too, or have implemented measures to decrease leaks.
Internationally, 192 governments agreed in the Kyoto protocol of 2005 to reduce halogenated hydrocarbons – resulting from inhalation gases, including desflurane and nitrous oxide – because of their immense climate-warming potential, and in 2016, they pledged to eliminate them by 2035. However, the use of inhalation anesthetics continues to increase worldwide, not least because more people access healthcare in developing countries, and because people in industrialized countries live longer and therefore need more surgeries. Significant traces of inhalation gases have been found in Antarctica and the Himalayas, far from the vast majority of surgery rooms.
Certain companies are now pushing new technology to capture inhalation gases before they are released into the atmosphere, but both Sherman and Koch believe marketing claims of 99 percent efficiency amount to greenwashing. After investigating the technology first-hand and visiting the company that is producing such filters in Germany, Koch concluded that such technology only reduces emissions by 25 percent. And Sherman believes such initiatives are akin to the fallacy of recycling plastic. In addition to questioning their efficiency, Sherman fears such technology “gives the illusion there is a magical solution that means I don’t need to change my behavior, reduce my waste and choose less harmful options.”
Financial interests are at play, too. “Desflurane is the most expensive inhalation gas, and some think, the most expensive must be the best,” Koch says. Both Koch and Sherman lament that efforts to increase sustainability in the medical sector are entirely voluntary in their countries and led by a few dedicated individual professionals while industry-wide standards and transparency are needed, a notion expressed in the American Hospital Association’s Sustainability Roadmap.

Susanne Koch, an anesthesiologist in Berlin, wants her colleagues to stop using a gas called desflurane, which is by far the most damaging of all inhalation gases to the climate.
Adobe Stock
Other countries have done more. The European Union recommends reducing inhalation gases and even contemplated a ban of desflurane, except in medical emergencies. In 2008, the National Health Service (NHS) created a Sustainable Development Unit, which measures CO2 emissions in the U.K. health sector. NHS is the first national health service that pledged to reach net zero carbon by 2040. The carbon footprint of the NHS fell by 26 percent from 1990 to 2019, mostly due to reduced use of certain inhalers and the switch to renewable energy for heat and power. “The evidence that the climate emergency is a health emergency is overwhelming,” said Nick Watts, the NHS Chief Sustainability Officer, in a press release, “with health professionals already needing to manage its symptoms.”
Sherman is a leading voice in demanding action in the U.S. To her, comprehensive solutions start with the mandatory, transparent measurement of emissions in the health sector to tackle the biggest sources of pollution. While the Biden administration highlighted its efforts to reduce these kinds of emissions during the United Nations Climate Conference (COP27) in November 2022 and U.S. delegates announced that more than 100 health care organizations signed the voluntary Health Sector Climate Pledge, with the aim to reduce emissions by 50 percent in the next eight years, Sherman is convinced that voluntary pledges are not enough. “Voluntary measures are insufficient,” she testified in congress. “The vast majority of U.S. health care organizations remain uncommitted to timely action. Those that are committed lack policies and knowledge to support necessary changes; even worse, existing policies drive inappropriate consumption of resources and pollution.”
Both Sherman and Koch look at the larger picture. “Health care organizations have an obligation to their communities to protect public health,” Sherman says. “We must lead by example. That includes setting ambitious, science-based carbon reduction targets to achieve net zero emissions before 2050. We must quantify current emissions and their sources, particularly throughout the health care supply chains.”

