Isaac Asimov on the History of Infectious Disease—and How Humanity Learned to Fight Back

Children in Mississippi get vaccinated against polio with the Salk vaccine in 1956.
[EDITOR'S FORWARD: Humanity has always faced existential threats from dangerous microbes, and though this is the first pandemic in our lifetimes, it won't be the last our species will ever face. This newly relevant work by beloved sci-fi writer Isaac Asimov, an excerpt from his 1979 book, A Choice of Catastrophes, establishes that reality in its historical context and makes clear how far we have come since ancient times. But by some measures, we are still in the earliest stages of figuring out how to effectively neutralize such threats. Advancing progress as fast as we can—by leveraging all the insights of modern science—offers our best hope for containing this pandemic and those that will inevitably follow.]
Infectious Disease
An even greater danger to humanity than the effect of small, fecund pests on human beings, their food, and their possessions, is their tendency to spread some forms of infectious disease.
Every living organism is subject to disease of various sorts, where disease is defined in its broadest sense as "dis-ease," that is, as any malfunction or alteration of the physiology or biochemistry that interferes with the smooth workings of the organism. In the end, the cumulative effect of malfunctions, misfunctions, nonfunctions, even though much of it is corrected or patched up, produces irreversible damage—we call it old age—and, even with the best care in the world, brings on inevitable death.
Civilization has meant the development and growth of cities and the crowding of people into close quarters.
There are some individual trees that may live five thousand years, some cold-blooded animals that may live two hundred years, some warm-blooded animals that may live one hundred years, but for each multicellular individual death comes as the end.
This is an essential part of the successful functioning of life. New individuals constantly come into being with new combinations of chromosomes and genes, and with mutated genes, too. These represent new attempts, so to speak, at fitting the organism to the environment. Without the continuing arrival of new organisms that are not mere copies of the old, evolution would come to a halt. Naturally, the new organisms cannot perform their role properly unless the old ones are removed from the scene after they have performed their function of producing the new. In short, the death of the individual is essential to the life of the species.
It is essential, however, that the individual not die before the new generation has been produced; at least, not in so many cases as to ensure the population dwindling to extinction.
The human species cannot have the relative immunity to harm from individual death possessed by the small and fecund species. Human beings are comparatively large, long-lived, and slow to reproduce, so that too rapid individual death holds within it the specter of catastrophe. The rapid death of unusually high numbers of human beings through disease can seriously dent the human population. Carried to an extreme, it is not too hard to imagine it wiping out the human species.
Most dangerous in this respect is that class of malfunction referred to as "infectious disease." There are many disorders that affect a particular human being for one reason or another and may kill him or her, too, but which will not, in itself, offer a danger to the species, because it is strictly confined to the suffering individual. Where, however, a disease can, in some way travel from one human being to another, and where its occurrence in a single individual may lead to the death of not that one alone but of millions of others as well, then there is the possibility of catastrophe.
And indeed, infectious disease has come closer to destroying the human species in historic times than have the depredations of any animals. Although infectious disease, even at its worst, has never yet actually put an end to human beings as a living species (obviously), it can seriously damage a civilization and change the course of history. It has, in fact, done so not once, but many times.
What's more, the situation has perhaps grown worse with the coming of civilization. Civilization has meant the development and growth of cities and the crowding of people into close quarters. Just as fire can spread much more rapidly from tree to tree in a dense forest than in isolated stands, so can infectious disease spread more quickly in crowded quarters than in sparse settlements.
To mention a few notorious cases in history:
In 431 B.C., Athens and its allies went to war with Sparta and its allies. It was a twenty-seven-year war that ruined Athens and, to a considerable extent, all of Greece. Since Sparta controlled the land, the entire Athenian population crowded into the walled city of Athens. There they were safe and could be provisioned by sea, which was controlled by the Athenian navy. Athens would very likely have won a war of attrition before long and Greece might have avoided ruin, but for disease.
In 430 B.C., an infectious plague struck the crowded Athenian population and killed 20 percent of them, including the charismatic leader, Pericles. Athens kept on fighting but it never recovered its population or its strength and in the end it lost.
Plagues very frequently started in eastern and southern Asia, where population was densest, and spread westward. In A.D. 166, when the Roman Empire was at its peak of strength and civilization under the hard-working philosopher-emperor Marcus Aurelius, the Roman armies, fighting on the eastern borders in Asia Minor, began to suffer from an epidemic disease (possibly smallpox). They brought it back with them to other provinces and to Rome itself. At its height, 2,000 people were dying in the city of Rome each day. The population began to decline and did not reach its preplague figure again until the twentieth century. There are a great many reasons advanced for the long, slow decline of Rome that followed the reign of Marcus Aurelius, but the weakening effect of the plague of 166 surely played a part.
Even after the western provinces of the empire were torn away by invasions of the German tribes, and Rome itself was lost, the eastern half of the Roman Empire continued to exist, with its capital at Constantinople. Under the capable emperor Justinian I, who came to the throne in 527, Africa, Italy, and parts of Spain were taken and, for a while, it looked as though the empire might be reunited. In 541, however, the bubonic plague struck. It was a disease that attacked rats primarily, but one that fleas could spread to human beings by biting first a sick rat and then a healthy human being. Bubonic disease was fast-acting and often quickly fatal. It may even have been accompanied by a more deadly variant, pneumonic plague, which can leap directly from one person to another.
For two years the plague raged, and between one-third and one-half of the population of the city of Constantinople died, together with many people in the countryside outside the city. There was no hope of uniting the empire thereafter and the eastern portion, which came to be known as the Byzantine Empire, continued to decline thereafter (with occasional rallies).
The very worst epidemic in the history of the human species came in the fourteenth century. Sometime in the 1330s, a new variety of bubonic plague, a particularly deadly one, appeared in central Asia. People began to die and the plague spread outward, inexorably, from its original focus.
Eventually, it reached the Black Sea. There on the Crimean peninsula, jutting into the north-central coast of that sea, was a seaport called Kaffa where the Italian city of Genoa had established a trading post. In October, 1347, a Genoese ship just managed to make it back to Genoa from Kaffa. The few men on board who were not dead of the plague were dying. They were carried ashore and thus the plague entered Europe and began to spread rapidly.
Sometimes one caught a mild version of the disease, but often it struck violently. In the latter case, the patient was almost always dead within one to three days after the onset of the first symptoms. Because the extreme dangers were marked by hemorrhagic spots that turned dark, the disease was called the "Black Death."
The Black Death spread unchecked. It is estimated to have killed some 25 million people in Europe before it died down and many more than that in Africa and Asia. It may have killed a third of all the human population of the planet, perhaps 60 million people altogether or even more. Never before or after do we know of anything that killed so large a percentage of the population as did the Black Death.
It is no wonder that it inspired abject terror among the populace. Everyone walked in fear. A sudden attack of shivering or giddiness, a mere headache, might mean that death had marked one for its own and that no more than a couple of dozen hours were left in which to die. Whole towns were depopulated, with the first to die lying unburied while the survivors fled to spread the disease. Farms lay untended; domestic animals wandered uncared for. Whole nations—Aragon, for instance, in what is now eastern Spain—were afflicted so badly that they never truly recovered.
Distilled liquors had been first developed in Italy about 1100. Now, two centuries later they grew popular. The theory was that strong drink acted as a preventive against contagion. It didn't, but it made the drinker less concerned which, under the circumstances, was something. Drunkenness set in over Europe and it stayed even after the plague was gone; indeed, it has never left. The plague also upset the feudal economy by cutting down on the labor supply very drastically. This did as much to destroy feudalism as did the invention of gunpowder. (Perhaps the most distressing sidelight of the Black Death is the horrible insight into human nature that it offers. England and France were in the early decades of the Hundred Years War at the time. Although the Black Death afflicted both nations and nearly destroyed each, the war continued right on. There was no thought of peace in this greatest of all crises faced by the human species.)
There have been other great plagues since, though none to match the Black Death in unrivaled terror and destruction. In 1664 and 1665, the bubonic plague struck London and killed 75,000.
Cholera, which always simmered just below the surface in India (where it is "endemic") would occasionally explode and spread outward into an "epidemic." Europe was visited by deadly cholera epidemics in 1831 and again in 1848 and 1853. Yellow fever, a tropical disease, would be spread by sailors to more northern seaports, and periodically American cities would be decimated by it. Even as late as 1905, there was a bad yellow fever epidemic in New Orleans.
The most serious epidemic since the Black Death, was one of "Spanish influenza" which struck the world in 1918 and in one year killed 30 million people the world over, and about 600,000 of them in the United States. In comparison, four years of World War I, just preceding 1918, had killed 8 million. However, the influenza epidemic killed less than 2 percent of the world's population, so that the Black Death remains unrivaled.
What stands between such a catastrophe and us is the new knowledge we have gained in the last century and a half concerning the causes of infectious disease and methods for fighting it.
[…] Infectious disease is clearly more dangerous to human existence than any animal possibly could be, and we might be right to wonder whether it might not produce a final catastrophe before the glaciers ever have a chance to invade again and certainly before the sun begins to inch its way toward red gianthood.
What stands between such a catastrophe and us is the new knowledge we have gained in the last century and a half concerning the causes of infectious disease and methods for fighting it.
Microorganisms
People, throughout most of history, had no defense whatever against infectious disease. Indeed, the very fact of infection was not recognized in ancient and medieval times. When people began dying in droves, the usual theory was that an angry god was taking vengeance for some reason or other. Apollo's arrows were flying, so that one death was not responsible for another; Apollo was responsible for all, equally.
The Bible tells of a number of epidemics and in each case it is the anger of God kindled against sinners, as in 2 Samuel 24. In New Testament times, the theory of demonic possession as an explanation of disease was popular, and both Jesus and others cast our devils. The biblical authority for this has caused the theory to persist to this day, as witness by the popularity of such movies as The Exorcist.
As long as disease was blamed on divine or demonic influences, something as mundane as contagion was overlooked. Fortunately, the Bible also contains instructions for isolating those with leprosy (a name given not only to leprosy itself, but to other, less serious skin conditions). The biblical practice of isolation was for religious rather than hygienic reasons, for leprosy has a very low infectivity. On biblical authority, lepers were isolated in the Middle Ages, while those with really infectious disease were not. The practice of isolation, however, caused some physicians to think of it in connection with disease generally. In particular, the ultimate terror of the Black Death helped spread the notion of quarantine, a name which referred originally to isolation for forty (quarante in French) days.
The fact that isolation did slow the spread of a disease made it look as though contagion was a factor. The first to deal with this possibility in detail was an Italian physician, Girolamo Fracastoro (1478–1553). In 1546, he suggested that disease could be spread by direct contact of a well person with an ill one or by indirect contact of a well person with infected articles or even through transmission over a distance. He suggested that minute bodies, too small to be seen, passed from an ill person to a well one and that the minute bodies had the power of self-multiplication.
It was a remarkable bit of insight, but Fracastoro had no firm evidence to support his theory. If one is going to accept minute unseen bodies leaping from one body to another and do it on nothing more than faith, one might as well accept unseen demons.
Minute bodies did not, however, remain unseen. Already in Fracastoro's time, the use of lenses to aid vision was well established. By 1608, combinations of lenses were used to magnify distant objects and the telescope came into existence. It didn't take much of a modification to have lenses magnify tiny objects. The Italian physiologist Marcello Malpighi (1628–94) was the first to use a microscope for important work, reporting his observations in the 1650s.
The Dutch microscopist Anton van Leeuwenhoek (1632–1723) laboriously ground small but excellent lenses, which gave him a better view of the world of tiny objects than anyone else in his time had had. In 1677, he placed ditch water at the focus of one of his small lenses and found living organisms too small to see with the naked eye but each one as indisputably alive as a whale or an elephant—or as a human being. These were the one-celled animals we now call "protozoa."
In 1683, van Leeuwenhoek discovered structures still tinier than protozoa. They were at the limit of visibility with even his best lenses, but from his sketches of what he saw, it is clear that he had discovered bacteria, the smallest cellular creatures that exist.
To do any better than van Leeuwenhoek, one had to have distinctly better microscopes and these were slow to be developed. The next microscopist to describe bacteria was the Danish biologist Otto Friedrich Müller (1730–84) who described them in a book on the subject, published posthumously, in 1786.
In hindsight, it seems that one might have guessed that bacteria represented Fracastoro's infectious agents, but there was no evidence of that and even Müller's observations were so borderline that there was no general agreement that bacteria even existed, or that they were alive if they did.
The English optician Joseph Jackson Lister (1786–1869) developed an achromatic microscope in in 1830. Until then, the lenses used had refracted light into rainbows so that tiny objects were rimmed in color and could not be seen clearly. Lister combined lenses of different kinds of glass in such a way as to remove the colors.
With the colors gone, tiny objects stood out sharply and in the 1860s, the German botanist Ferdinand Julius Cohn (1828–98) saw and described bacteria with the first really convincing success. It was only with Cohn's work that the science of bacteriology was founded and that there came to be general agreement that bacteria existed.
Meanwhile, even without a clear indication of the existence of Fracastoro's agents, some physicians were discovering methods of reducing infection.
The Hungarian physician Ignaz Philipp Semmelweiss (1818–65) insisted that childbed fever which killed so many mothers in childbirth, was spread by the doctors themselves, since they went from autopsies straight to women in labor. He fought to get the doctors to wash their hands before attending the women, and when he managed to enforce this, in 1847, the incidence of childbed fever dropped precipitously. The insulted doctors, proud of their professional filth, revolted at this, however and finally managed to do their work with dirty hands again. The incidence of childbed fever climbed as rapidly as it had fallen—but that didn't bother the doctors.
The crucial moment came with the work of the French chemist Louis Pasteur (1822–95). Although he was a chemist his work had turned him more and more toward microscopes and microorganisms, and in 1865 he set to work studying a silkworm disease that was destroying France's silk industry. Using his microscope, he discovered a tiny parasite infesting the silkworms and the mulberry leaves that were fed to them. Pasteur's solution was drastic but rational. All infested worms and infested food must be destroyed. A new beginning must be made with healthy worms and the disease would be wiped out. His advice was followed and it worked. The silk industry was saved.
This turned Pasteur's interest to contagious diseases. It seemed to him that if the silkworm disease was the product of microscopic parasites other diseases might be, and thus was born the "germ theory of disease." Fracastoro's invisible infectious agents were microorganisms, often the bacteria that Cohn was just bringing clearly into the light of day.
It now became possible to attack infectious disease rationally, making use of a technique that had been introduced to medicine over half a century before. In 1798, the English physician Edward Jenner (1749–1823) had shown that people inoculated with the mild disease, cowpox, or vaccinia in Latin, acquired immunity not only to cowpox itself but also to the related but very virulent and dreaded disease, smallpox. The technique of "vaccination" virtually ended most of the devastation of smallpox.
Unfortunately, no other diseases were found to occur in such convenient pairs, with the mild one conferring immunity from the serious one. Nevertheless, with the notion of the germ theory the technique could be extended in another way.
Pasteur located specific germs associated with specific diseases, then weakened those germs by heating them or in other ways, and used the weakened germs for inoculation. Only a very mild disease was produced but immunity was conferred against the dangerous one. The first disease treated in this way was the deadly anthrax that ravaged herds of domestic animals.
Similar work was pursued even more successfully by the German bacteriologist Robert Koch (1843–1910). Antitoxins designed to neutralize bacterial poisons were also developed.
Meanwhile, the English surgeon Joseph Lister (1827–1912), the son of the inventor of the achromatic microscope, had followed up Semmelweiss's work. Once he learned of Pasteur's research he had a convincing rationale as excuse and began to insist that, before operating, surgeons wash their hands in solutions of chemicals known to kill bacteria. From 1867 on, the practice of "antiseptic surgery" spread quickly.
The germ theory also sped the adoption of rational preventive measures—personal hygiene, such as washing and bathing; careful disposal of wastes; the guarding of the cleanliness of food and water. Leaders in this were the German scientist Max Joseph von Pettenkofer (1818–1901) and Rudolph Virchow (1821–1902). They themselves did not accept the germ theory of disease but their recommendations would not have been followed as readily were it not that others did.
In addition, it was discovered that diseases such as yellow fever and malaria were transmitted by mosquitoes, typhus fever by lice, Rocky Mountain spotted fever by ticks, bubonic plague by fleas and so on. Measures against these small germ-transferring organisms acted to reduce the incidence of the diseases. Men such as the Americans Walter Reed (1851–1902) and Howard Taylor Ricketts (1871–1910) and the Frenchman Charles J. Nicolle (1866–1936) were involved in such discoveries.
The German bacteriologist Paul Ehrlich (1854–1915) pioneered the use of specific chemicals that would kill particular bacteria without killing the human being in which it existed. His most successful discovery came in 1910, when he found an arsenic compound that was active against the bacterium that causes syphilis.
This sort of work culminated in the discovery of the antibacterial effect of sulfanilamide and related compounds, beginning with the work of the German biochemist Gerhard Domagk (1895–1964) in 1935 and of antibiotics, beginning with the work of the French-American microbiologist René Jules Dubos (1901–[1982]) in 1939.
As late as 1955 came a victory over poliomyelitis, thanks to a vaccine prepared by the American microbiologist Jonas Edward Salk (1914–[1995]).
And yet victory is not total. Right now, the once ravaging disease of smallpox seems to be wiped out. Not one case exists, as far as we know, in the entire world. There are however infectious diseases such as a few found in Africa that are very contagious, virtually 100 percent fatal, and for which no cure exists. Careful hygienic measures have made it possible for such diseases to be studied without their spreading, and no doubt effective countermeasures will be worked out.
New Disease
It would seem, then, that as long as our civilization survives and our medical technology is not shattered there is no longer any danger that infectious disease will produce catastrophe or even anything like the disasters of the Black Death and the Spanish influenza. Yet, old familiar diseases have, within them, the potentiality of arising in new forms.
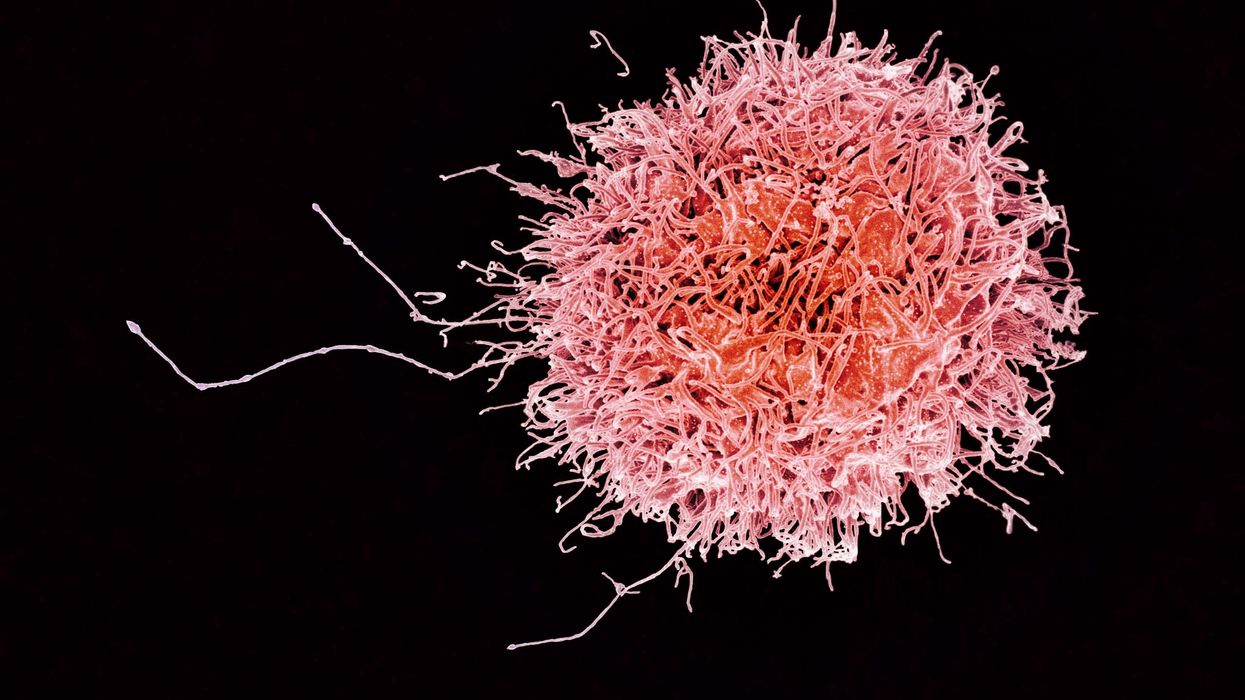
The human body (and all living organisms) have natural defenses against the invasion of foreign organisms. Antibodies are developed in the bloodstream that neutralize toxins or the microorganisms themselves. White cells in the blood stream physically attack bacteria.
Every few years a new strain of flu rises to pester us. It is possible, however, to produce vaccines against such a new strain once it makes an appearance.
Evolutionary processes generally make the fight an even one. Those organisms more efficient at self-protection against microorganisms tend to survive and pass on their efficiency to their offspring. Nevertheless, microorganisms are far smaller even than insects and far more fecund. They evolve much more quickly, with individual microorganisms almost totally unimportant in the scheme of things.
Considering the uncounted numbers of microorganisms of any particular species that are continually multiplying by cell fission, large numbers of mutations must be produced just as continually. Every once in a while such a mutation may act to make a particular disease far more infectious and deadly. Furthermore, it may sufficiently alter the chemical nature of the microorganism so that the antibodies which the host organism is capable of manufacturing are no longer usable. The result is the sudden onslaught of an epidemic. The Black Death was undoubtedly brought about by a mutant strain of the microorganism causing it.
Eventually, though, those human beings who are most susceptible die, and the relatively resistant survive, so that the virulence of the diseases dies down. In that case, is the human victory over the pathogenic microorganism permanent? Might not new strains of germs arise? They might and they do. Every few years a new strain of flu rises to pester us. It is possible, however, to produce vaccines against such a new strain once it makes an appearance. Thus, when a single case of "swine flu" appeared in 1976, a full scale mass-vaccination was set in action. It turned out not to be needed, but it showed what could be done.
Copyright © 1979 by Isaac Asimov, A Choice of Catastrophes: The Disasters That Threaten Our World, originally published by Simon & Schuster. Reprinted with permission from the Asimov estate.
[This article was originally published on June 8th, 2020 as part of a standalone magazine called GOOD10: The Pandemic Issue. Produced as a partnership among LeapsMag, The Aspen Institute, and GOOD, the magazine is available for free online.]
Dr. May Edward Chinn, Kizzmekia Corbett, PhD., and Alice Ball, among others, have been behind some of the most important scientific work of the last century.
If you look back on the last century of scientific achievements, you might notice that most of the scientists we celebrate are overwhelmingly white, while scientists of color take a backseat. Since the Nobel Prize was introduced in 1901, for example, no black scientists have landed this prestigious award.
The work of black women scientists has gone unrecognized in particular. Their work uncredited and often stolen, black women have nevertheless contributed to some of the most important advancements of the last 100 years, from the polio vaccine to GPS.
Here are five black women who have changed science forever.
Dr. May Edward Chinn
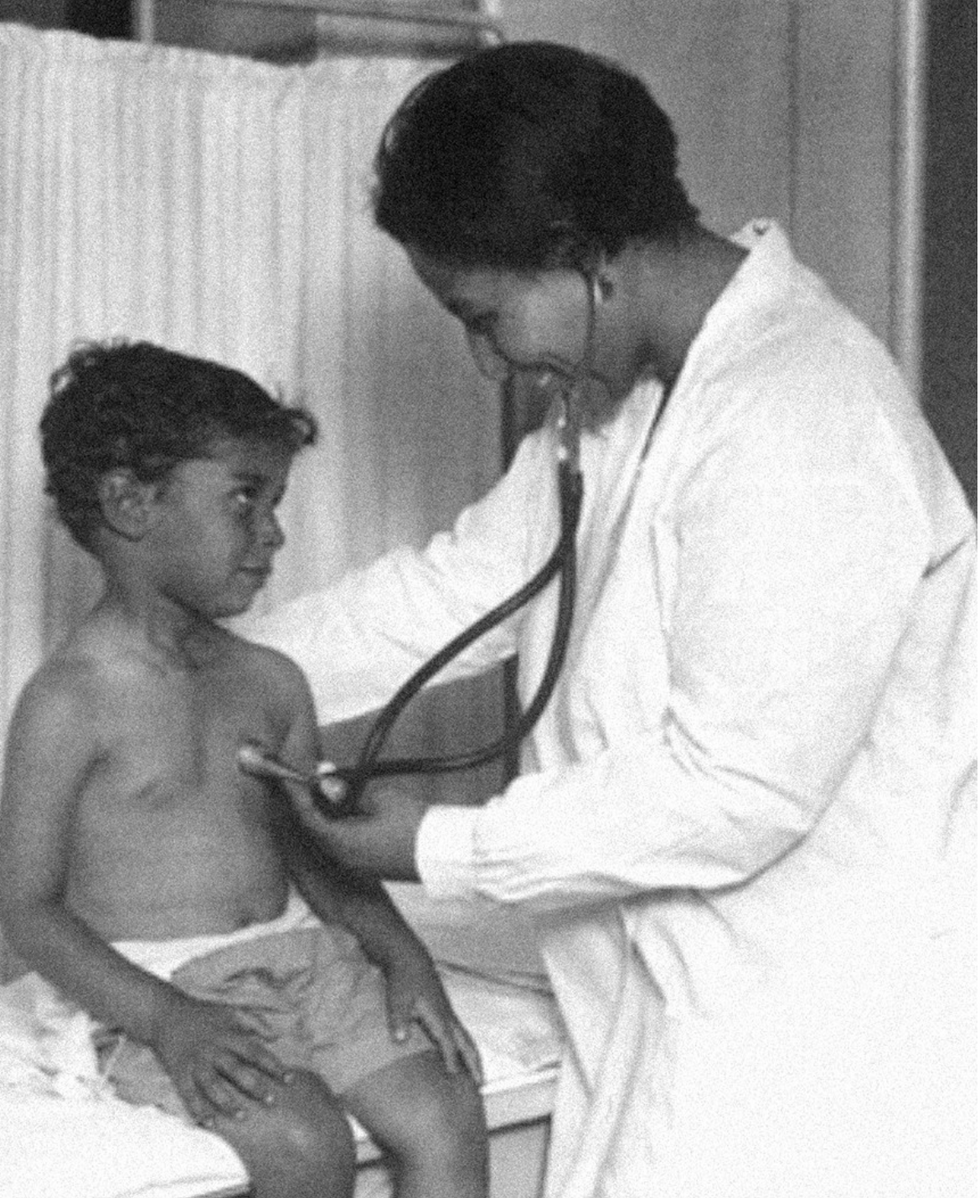
Dr. May Edward Chinn practicing medicine in Harlem
George B. Davis, PhD.
Chinn was born to poor parents in New York City just before the start of the 20th century. Although she showed great promise as a pianist, playing with the legendary musician Paul Robeson throughout the 1920s, she decided to study medicine instead. Chinn, like other black doctors of the time, were barred from studying or practicing in New York hospitals. So Chinn formed a private practice and made house calls, sometimes operating in patients’ living rooms, using an ironing board as a makeshift operating table.
Chinn worked among the city’s poor, and in doing this, started to notice her patients had late-stage cancers that often had gone undetected or untreated for years. To learn more about cancer and its prevention, Chinn begged information off white doctors who were willing to share with her, and even accompanied her patients to other clinic appointments in the city, claiming to be the family physician. Chinn took this information and integrated it into her own practice, creating guidelines for early cancer detection that were revolutionary at the time—for instance, checking patient health histories, checking family histories, performing routine pap smears, and screening patients for cancer even before they showed symptoms. For years, Chinn was the only black female doctor working in Harlem, and she continued to work closely with the poor and advocate for early cancer screenings until she retired at age 81.
Alice Ball

Pictorial Press Ltd/Alamy
Alice Ball was a chemist best known for her groundbreaking work on the development of the “Ball Method,” the first successful treatment for those suffering from leprosy during the early 20th century.
In 1916, while she was an undergraduate student at the University of Hawaii, Ball studied the effects of Chaulmoogra oil in treating leprosy. This oil was a well-established therapy in Asian countries, but it had such a foul taste and led to such unpleasant side effects that many patients refused to take it.
So Ball developed a method to isolate and extract the active compounds from Chaulmoogra oil to create an injectable medicine. This marked a significant breakthrough in leprosy treatment and became the standard of care for several decades afterward.
Unfortunately, Ball died before she could publish her results, and credit for this discovery was given to another scientist. One of her colleagues, however, was able to properly credit her in a publication in 1922.
Henrietta Lacks

onathan Newton/The Washington Post/Getty
The person who arguably contributed the most to scientific research in the last century, surprisingly, wasn’t even a scientist. Henrietta Lacks was a tobacco farmer and mother of five children who lived in Maryland during the 1940s. In 1951, Lacks visited Johns Hopkins Hospital where doctors found a cancerous tumor on her cervix. Before treating the tumor, the doctor who examined Lacks clipped two small samples of tissue from Lacks’ cervix without her knowledge or consent—something unthinkable today thanks to informed consent practices, but commonplace back then.
As Lacks underwent treatment for her cancer, her tissue samples made their way to the desk of George Otto Gey, a cancer researcher at Johns Hopkins. He noticed that unlike the other cell cultures that came into his lab, Lacks’ cells grew and multiplied instead of dying out. Lacks’ cells were “immortal,” meaning that because of a genetic defect, they were able to reproduce indefinitely as long as certain conditions were kept stable inside the lab.
Gey started shipping Lacks’ cells to other researchers across the globe, and scientists were thrilled to have an unlimited amount of sturdy human cells with which to experiment. Long after Lacks died of cervical cancer in 1951, her cells continued to multiply and scientists continued to use them to develop cancer treatments, to learn more about HIV/AIDS, to pioneer fertility treatments like in vitro fertilization, and to develop the polio vaccine. To this day, Lacks’ cells have saved an estimated 10 million lives, and her family is beginning to get the compensation and recognition that Henrietta deserved.
Dr. Gladys West

Andre West
Gladys West was a mathematician who helped invent something nearly everyone uses today. West started her career in the 1950s at the Naval Surface Warfare Center Dahlgren Division in Virginia, and took data from satellites to create a mathematical model of the Earth’s shape and gravitational field. This important work would lay the groundwork for the technology that would later become the Global Positioning System, or GPS. West’s work was not widely recognized until she was honored by the US Air Force in 2018.
Dr. Kizzmekia "Kizzy" Corbett

TIME Magazine
At just 35 years old, immunologist Kizzmekia “Kizzy” Corbett has already made history. A viral immunologist by training, Corbett studied coronaviruses at the National Institutes of Health (NIH) and researched possible vaccines for coronaviruses such as SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome).
At the start of the COVID pandemic, Corbett and her team at the NIH partnered with pharmaceutical giant Moderna to develop an mRNA-based vaccine against the virus. Corbett’s previous work with mRNA and coronaviruses was vital in developing the vaccine, which became one of the first to be authorized for emergency use in the United States. The vaccine, along with others, is responsible for saving an estimated 14 million lives.On today’s episode of Making Sense of Science, I’m honored to be joined by Dr. Paul Song, a physician, oncologist, progressive activist and biotech chief medical officer. Through his company, NKGen Biotech, Dr. Song is leveraging the power of patients’ own immune systems by supercharging the body’s natural killer cells to make new treatments for Alzheimer’s and cancer.
Whereas other treatments for Alzheimer’s focus directly on reducing the build-up of proteins in the brain such as amyloid and tau in patients will mild cognitive impairment, NKGen is seeking to help patients that much of the rest of the medical community has written off as hopeless cases, those with late stage Alzheimer’s. And in small studies, NKGen has shown remarkable results, even improvement in the symptoms of people with these very progressed forms of Alzheimer’s, above and beyond slowing down the disease.
In the realm of cancer, Dr. Song is similarly setting his sights on another group of patients for whom treatment options are few and far between: people with solid tumors. Whereas some gradual progress has been made in treating blood cancers such as certain leukemias in past few decades, solid tumors have been even more of a challenge. But Dr. Song’s approach of using natural killer cells to treat solid tumors is promising. You may have heard of CAR-T, which uses genetic engineering to introduce cells into the body that have a particular function to help treat a disease. NKGen focuses on other means to enhance the 40 plus receptors of natural killer cells, making them more receptive and sensitive to picking out cancer cells.
Paul Y. Song, MD is currently CEO and Vice Chairman of NKGen Biotech. Dr. Song’s last clinical role was Asst. Professor at the Samuel Oschin Cancer Center at Cedars Sinai Medical Center.
Dr. Song served as the very first visiting fellow on healthcare policy in the California Department of Insurance in 2013. He is currently on the advisory board of the Pritzker School of Molecular Engineering at the University of Chicago and a board member of Mercy Corps, The Center for Health and Democracy, and Gideon’s Promise.
Dr. Song graduated with honors from the University of Chicago and received his MD from George Washington University. He completed his residency in radiation oncology at the University of Chicago where he served as Chief Resident and did a brachytherapy fellowship at the Institute Gustave Roussy in Villejuif, France. He was also awarded an ASTRO research fellowship in 1995 for his research in radiation inducible gene therapy.
With Dr. Song’s leadership, NKGen Biotech’s work on natural killer cells represents cutting-edge science leading to key findings and important pieces of the puzzle for treating two of humanity’s most intractable diseases.
Show links
- Paul Song LinkedIn
- NKGen Biotech on Twitter - @NKGenBiotech
- NKGen Website: https://nkgenbiotech.com/
- NKGen appoints Paul Song
- Patient Story: https://pix11.com/news/local-news/long-island/promising-new-treatment-for-advanced-alzheimers-patients/
- FDA Clearance: https://nkgenbiotech.com/nkgen-biotech-receives-ind-clearance-from-fda-for-snk02-allogeneic-natural-killer-cell-therapy-for-solid-tumors/Q3 earnings data: https://www.nasdaq.com/press-release/nkgen-biotech-inc.-reports-third-quarter-2023-financial-results-and-business