The Science of Why Adjusting to Omicron Is So Tough
A brain expert weighs in on the cognitive biases that hold us back from adjusting to the new reality of Omicron.
We are sticking our heads into the sand of reality on Omicron, and the results may be catastrophic.
Omicron is over 4 times more infectious than Delta. The Pfizer two-shot vaccine offers only 33% protection from infection. A Pfizer booster vaccine does raises protection to about 75%, but wanes to around 30-40 percent 10 weeks after the booster.
The only silver lining is that Omicron appears to cause a milder illness than Delta. Yet the World Health Organization has warned about the “mildness” narrative.
That’s because the much faster disease transmission and vaccine escape undercut the less severe overall nature of Omicron. That’s why hospitals have a large probability of being overwhelmed, as the Center for Disease Control warned, in this major Omicron wave.
Yet despite this very serious threat, we see the lack of real action. The federal government tightened international travel guidelines and is promoting boosters. Certainly, it’s crucial to get as many people to get their booster – and initial vaccine doses – as soon as possible. But the government is not taking the steps that would be the real game-changers.
Pfizer’s anti-viral drug Paxlovid decreases the risk of hospitalization and death from COVID by 89%. Due to this effectiveness, the FDA approved Pfizer ending the trial early, because it would be unethical to withhold the drug from people in the control group. Yet the FDA chose not to hasten the approval process along with the emergence of Omicron in late November, only getting around to emergency authorization in late December once Omicron took over. That delay meant the lack of Paxlovid for the height of the Omicron wave, since it takes many weeks to ramp up production, resulting in an unknown number of unnecessary deaths.
We humans are prone to falling for dangerous judgment errors called cognitive biases.
Widely available at-home testing would enable people to test themselves quickly, so that those with mild symptoms can quarantine instead of infecting others. Yet the federal government did not make tests available to patients when Omicron emerged in late November. That’s despite the obviousness of the coming wave based on the precedent of South Africa, UK, and Denmark and despite the fact that the government made vaccines freely available. Its best effort was to mandate that insurance cover reimbursements for these kits, which is way too much of a barrier for most people. By the time Omicron took over, the federal government recognized its mistake and ordered 500 million tests to be made available in January. However, that’s far too late. And the FDA also played a harmful role here, with its excessive focus on accuracy going back to mid-2020, blocking the widespread availability of cheap at-home tests. By contrast, Europe has a much better supply of tests, due to its approval of quick and slightly less accurate tests.
Neither do we see meaningful leadership at the level of employers. Some are bringing out the tired old “delay the office reopening” play. For example, Google, Uber, and Ford, along with many others, have delayed the return to the office for several months. Those that already returned are calling for stricter pandemic measures, such as more masks and social distancing, but not changing their work arrangements or adding sufficient ventilation to address the spread of COVID.
Despite plenty of warnings from risk management and cognitive bias experts, leaders are repeating the same mistakes we fell into with Delta. And so are regular people. For example, surveys show that Omicron has had very little impact on the willingness of unvaccinated Americans to get a first vaccine dose, or of vaccinated Americans to get a booster. That’s despite Omicron having taken over from Delta in late December.
What explains this puzzling behavior on both the individual and society level? We humans are prone to falling for dangerous judgment errors called cognitive biases. Rooted in wishful thinking and gut reactions, these mental blindspots lead to poor strategic and financial decisions when evaluating choices.
These cognitive biases stem from the more primitive, emotional, and intuitive part of our brains that ensured survival in our ancestral environment. This quick, automatic reaction of our emotions represents the autopilot system of thinking, one of the two systems of thinking in our brains. It makes good decisions most of the time but also regularly makes certain systematic thinking errors, since it’s optimized to help us survive. In modern society, our survival is much less at risk, and our gut is more likely to compel us to focus on the wrong information to make decisions.
One of the biggest challenges relevant to Omicron is the cognitive bias known as the ostrich effect. Named after the myth that ostriches stick their heads into the sand when they fear danger, the ostrich effect refers to people denying negative reality. Delta illustrated the high likelihood of additional dangerous variants, yet we failed to pay attention to and prepare for such a threat.
We want the future to be normal. We’re tired of the pandemic and just want to get back to pre-pandemic times. Thus, we greatly underestimate the probability and impact of major disruptors, like new COVID variants. That cognitive bias is called the normalcy bias.
When we learn one way of functioning in any area, we tend to stick to that way of functioning. You might have heard of this as the hammer-nail syndrome: when you have a hammer, everything looks like a nail. That syndrome is called functional fixedness. This cognitive bias causes those used to their old ways of action to reject any alternatives, including to prepare for a new variant.
Our minds naturally prioritize the present. We want what we want now, and downplay the long-term consequences of our current desires. That fallacious mental pattern is called hyperbolic discounting, where we excessively discount the benefits of orienting toward the future and focus on the present. A clear example is focusing on the short-term perceived gains of trying to return to normal over managing the risks of future variants.
The way forward into the future is to defeat cognitive biases and avoid denying reality by rethinking our approach to the future.
The FDA requires a serious overhaul. It’s designed for a non-pandemic environment, where the goal is to have a highly conservative, slow-going, and risk-averse approach so that the public feels confident trusting whatever it approved. That’s simply unacceptable in a fast-moving pandemic, and we are bound to face future pandemics in the future.
The federal government needs to have cognitive bias experts weigh in on federal policy. Putting all of its eggs in one basket – vaccinations – is not a wise move when we face the risks of a vaccine-escaping variant. Its focus should also be on expediting and prioritizing anti-virals, scaling up cheap rapid testing, and subsidizing high-filtration masks.
For employers, instead of dictating a top-down approach to how employees collaborate, companies need to adopt a decentralized team-led approach. Each individual team leader of a rank-and-file employee team should determine what works best for their team. After all, team leaders tend to know much more of what their teams need, after all. Moreover, they can respond to local emergencies like COVID surges.
At the same time, team leaders need to be trained to integrate best practices for hybrid and remote team leadership. Companies transitioned to telework abruptly as part of the March 2020 lockdowns. They fell into the cognitive bias of functional fixedness and transposed their pre-existing, in-office methods of collaboration on remote work. Zoom happy hours are a clear example: The large majority of employees dislike them, and research shows they are disconnecting, rather than connecting.
Yet supervisors continue to use them, despite the existence of much better methods of facilitating colalboration, which have been shown to work, such as virtual water cooler discussions, virtual coworking, and virtual mentoring. Leaders also need to facilitate innovation in hybrid and remote teams through techniques such as virtual asynchronous brainstorming. Finally, team leaders need to adjust performance evaluation to adapt to the needs of hybrid and remote teams.
On an individual level, people built up certain expectations during the first two years of the pandemic, and they don't apply with Omicron. For example, most people still think that a cloth mask is a fine source of protection. In reality, you really need an N-95 mask, since Omicron is so much more infectious. Another example is that many people don’t realize that symptom onset is much quicker with Omicron, and they aren’t prepared for the consequences.
Remember that we have a huge number of people who are asymptomatic, often without knowing it, due to the much higher mildness of Omicron. About 8% of people admitted to hospitals for other reasons in San Francisco test positive for COVID without symptoms, which we can assume translates for other cities. That means many may think they're fine and they're actually infectious. The result is a much higher chance of someone getting many other people sick.
During this time of record-breaking cases, you need to be mindful about your internalized assumptions and adjust your risk calculus accordingly. So if you can delay higher-risk activities, January and February might be the time to do it. Prepare for waves of disruptions to continue over time, at least through the end of February.
Of course, you might also choose to not worry about getting infected. If you are vaccinated and boosted, and do not have any additional health risks, you are very unlikely to have a serious illness due to Omicron. You can just take the small risk of a serious illness – which can happen – and go about your daily life. If doing so, watch out for those you care about who do have health concerns, since if you infect them, they might not have a mild case even with Omicron.
In short, instead of trying to turn back the clock to the lost world of January 2020, consider how we might create a competitive advantage in our new future. COVID will never go away: we need to learn to live with it. That means reacting appropriately and thoughtfully to new variants and being intentional about our trade-offs.
A movie still from the 1966 film "Fantastic Voyage"
In the 1966 movie "Fantastic Voyage," actress Raquel Welch and her submarine were shrunk to the size of a cell in order to eliminate a blood clot in a scientist's brain. Now, 55 years later, the scenario is becoming closer to reality.
California-based startup Bionaut Labs has developed a nanobot about the size of a grain of rice that's designed to transport medication to the exact location in the body where it's needed. If you think about it, the conventional way to deliver medicine makes little sense: A painkiller affects the entire body instead of just the arm that's hurting, and chemotherapy is flushed through all the veins instead of precisely targeting the tumor.
"Chemotherapy is delivered systemically," Bionaut-founder and CEO Michael Shpigelmacher says. "Often only a small percentage arrives at the location where it is actually needed."
But what if it was possible to send a tiny robot through the body to attack a tumor or deliver a drug at exactly the right location?
Several startups and academic institutes worldwide are working to develop such a solution but Bionaut Labs seems the furthest along in advancing its invention. "You can think of the Bionaut as a tiny screw that moves through the veins as if steered by an invisible screwdriver until it arrives at the tumor," Shpigelmacher explains. Via Zoom, he shares the screen of an X-ray machine in his Culver City lab to demonstrate how the half-transparent, yellowish device winds its way along the spine in the body. The nanobot contains a tiny but powerful magnet. The "invisible screwdriver" is an external magnetic field that rotates that magnet inside the device and gets it to move and change directions.
The current model has a diameter of less than a millimeter. Shpigelmacher's engineers could build the miniature vehicle even smaller but the current size has the advantage of being big enough to see with bare eyes. It can also deliver more medicine than a tinier version. In the Zoom demonstration, the micorobot is injected into the spine, not unlike an epidural, and pulled along the spine through an outside magnet until the Bionaut reaches the brainstem. Depending which organ it needs to reach, it could be inserted elsewhere, for instance through a catheter.
"The hope is that we can develop a vehicle to transport medication deep into the body," says Max Planck scientist Tian Qiu.
Imagine moving a screw through a steak with a magnet — that's essentially how the device works. But of course, the Bionaut is considerably different from an ordinary screw: "At the right location, we give a magnetic signal, and it unloads its medicine package," Shpigelmacher says.
To start, Bionaut Labs wants to use its device to treat Parkinson's disease and brain stem gliomas, a type of cancer that largely affects children and teenagers. About 300 to 400 young people a year are diagnosed with this type of tumor. Radiation and brain surgery risk damaging sensitive brain tissue, and chemotherapy often doesn't work. Most children with these tumors live less than 18 months. A nanobot delivering targeted chemotherapy could be a gamechanger. "These patients really don't have any other hope," Shpigelmacher says.
Of course, the main challenge of the developing such a device is guaranteeing that it's safe. Because tissue is so sensitive, any mistake could risk disastrous results. In recent years, Bionaut has tested its technology in dozens of healthy sheep and pigs with no major adverse effects. Sheep make a good stand-in for humans because their brains and spines are similar to ours.

The Bionaut device is about the size of a grain of rice.
Bionaut Labs
"As the Bionaut moves through brain tissue, it creates a transient track that heals within a few weeks," Shpigelmacher says. The company is hoping to be the first to test a nanobot in humans. In December 2022, it announced that a recent round of funding drew $43.2 million, for a total of 63.2 million, enabling more research and, if all goes smoothly, human clinical trials by early next year.
Once the technique has been perfected, further applications could include addressing other kinds of brain disorders that are considered incurable now, such as Alzheimer's or Huntington's disease. "Microrobots could serve as a bridgehead, opening the gateway to the brain and facilitating precise access of deep brain structure – either to deliver medication, take cell samples or stimulate specific brain regions," Shpigelmacher says.
Robot-assisted hybrid surgery with artificial intelligence is already used in state-of-the-art surgery centers, and many medical experts believe that nanorobotics will be the instrument of the future. In 2016, three scientists were awarded the Nobel Prize in Chemistry for their development of "the world's smallest machines," nano "elevators" and minuscule motors. Since then, the scientific experiments have progressed to the point where applicable devices are moving closer to actually being implemented.
Bionaut's technology was initially developed by a research team lead by Peer Fischer, head of the independent Micro Nano and Molecular Systems Lab at the Max Planck Institute for Intelligent Systems in Stuttgart, Germany. Fischer is considered a pioneer in the research of nano systems, which he began at Harvard University more than a decade ago. He and his team are advising Bionaut Labs and have licensed their technology to the company.
"The hope is that we can develop a vehicle to transport medication deep into the body," says Max Planck scientist Tian Qiu, who leads the cooperation with Bionaut Labs. He agrees with Shpigelmacher that the Bionaut's size is perfect for transporting medication loads and is researching potential applications for even smaller nanorobots, especially in the eye, where the tissue is extremely sensitive. "Nanorobots can sneak through very fine tissue without causing damage."
In "Fantastic Voyage," Raquel Welch's adventures inside the body of a dissident scientist let her swim through his veins into his brain, but her shrunken miniature submarine is attacked by antibodies; she has to flee through the nerves into the scientist's eye where she escapes into freedom on a tear drop. In reality, the exit in the lab is much more mundane. The Bionaut simply leaves the body through the same port where it entered. But apart from the dramatization, the "Fantastic Voyage" was almost prophetic, or, as Shpigelmacher says, "Science fiction becomes science reality."
This article was first published by Leaps.org on April 12, 2021.
How the Human Brain Project Built a Mind of its Own
In 2013, the Human Brain Project set out to build a realistic computer model of the brain over ten years. Now, experts are reflecting on HBP's achievements with an eye toward the future.
In 2009, neuroscientist Henry Markram gave an ambitious TED talk. “Our mission is to build a detailed, realistic computer model of the human brain,” he said, naming three reasons for this unmatched feat of engineering. One was because understanding the human brain was essential to get along in society. Another was because experimenting on animal brains could only get scientists so far in understanding the human ones. Third, medicines for mental disorders weren’t good enough. “There are two billion people on the planet that are affected by mental disorders, and the drugs that are used today are largely empirical,” Markram said. “I think that we can come up with very concrete solutions on how to treat disorders.”
Markram's arguments were very persuasive. In 2013, the European Commission launched the Human Brain Project, or HBP, as part of its Future and Emerging Technologies program. Viewed as Europe’s chance to try to win the “brain race” between the U.S., China, Japan, and other countries, the project received about a billion euros in funding with the goal to simulate the entire human brain on a supercomputer, or in silico, by 2023.
Now, after 10 years of dedicated neuroscience research, the HBP is coming to an end. As its many critics warned, it did not manage to build an entire human brain in silico. Instead, it achieved a multifaceted array of different goals, some of them unexpected.
Scholars have found that the project did help advance neuroscience more than some detractors initially expected, specifically in the area of brain simulations and virtual models. Using an interdisciplinary approach of combining technology, such as AI and digital simulations, with neuroscience, the HBP worked to gain a deeper understanding of the human brain’s complicated structure and functions, which in some cases led to novel treatments for brain disorders. Lastly, through online platforms, the HBP spearheaded a previously unmatched level of global neuroscience collaborations.
Simulating a human brain stirs up controversy
Right from the start, the project was plagued with controversy and condemnation. One of its prominent critics was Yves Fregnac, a professor in cognitive science at the Polytechnic Institute of Paris and research director at the French National Centre for Scientific Research. Fregnac argued in numerous articles that the HBP was overfunded based on proposals with unrealistic goals. “This new way of over-selling scientific targets, deeply aligned with what modern society expects from mega-sciences in the broad sense (big investment, big return), has been observed on several occasions in different scientific sub-fields,” he wrote in one of his articles, “before invading the field of brain sciences and neuromarketing.”
"A human brain model can simulate an experiment a million times for many different conditions, but the actual human experiment can be performed only once or a few times," said Viktor Jirsa, a professor at Aix-Marseille University.
Responding to such critiques, the HBP worked to restructure the effort in its early days with new leadership, organization, and goals that were more flexible and attainable. “The HBP got a more versatile, pluralistic approach,” said Viktor Jirsa, a professor at Aix-Marseille University and one of the HBP lead scientists. He believes that these changes fixed at least some of HBP’s issues. “The project has been on a very productive and scientifically fruitful course since then.”
After restructuring, the HBP became a European hub on brain research, with hundreds of scientists joining its growing network. The HBP created projects focused on various brain topics, from consciousness to neurodegenerative diseases. HBP scientists worked on complex subjects, such as mapping out the brain, combining neuroscience and robotics, and experimenting with neuromorphic computing, a computational technique inspired by the human brain structure and function—to name just a few.
Simulations advance knowledge and treatment options
In 2013, it seemed that bringing neuroscience into a digital age would be farfetched, but research within the HBP has made this achievable. The virtual maps and simulations various HBP teams create through brain imaging data make it easier for neuroscientists to understand brain developments and functions. The teams publish these models on the HBP’s EBRAINS online platform—one of the first to offer access to such data to neuroscientists worldwide via an open-source online site. “This digital infrastructure is backed by high-performance computers, with large datasets and various computational tools,” said Lucy Xiaolu Wang, an assistant professor in the Resource Economics Department at the University of Massachusetts Amherst, who studies the economics of the HBP. That means it can be used in place of many different types of human experimentation.
Jirsa’s team is one of many within the project that works on virtual brain models and brain simulations. Compiling patient data, Jirsa and his team can create digital simulations of different brain activities—and repeat these experiments many times, which isn’t often possible in surgeries on real brains. “A human brain model can simulate an experiment a million times for many different conditions,” Jirsa explained, “but the actual human experiment can be performed only once or a few times.” Using simulations also saves scientists and doctors time and money when looking at ways to diagnose and treat patients with brain disorders.
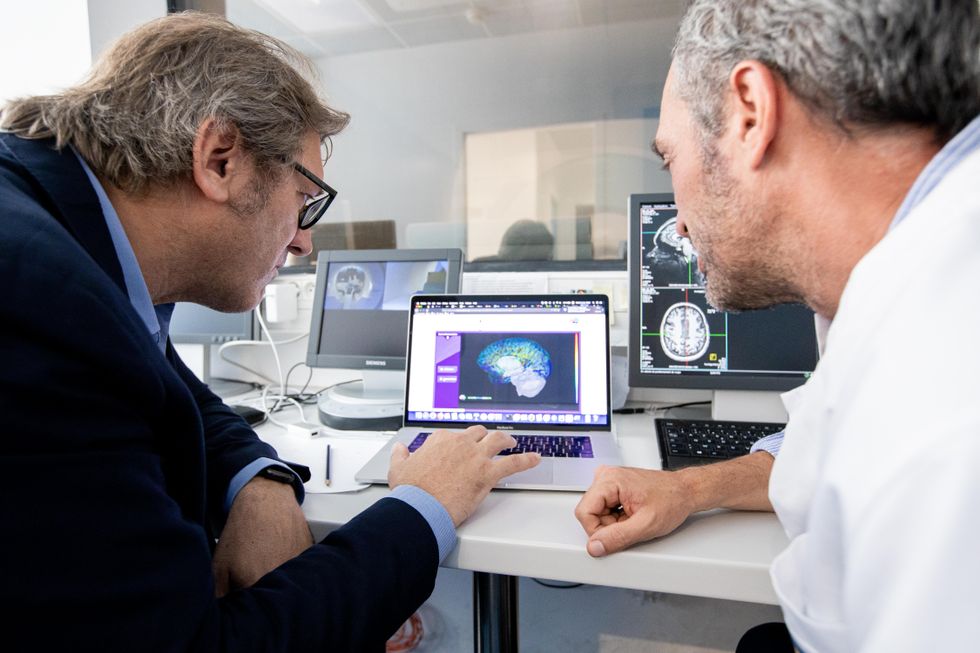
Compiling patient data, scientists can create digital simulations of different brain activities—and repeat these experiments many times.
The Human Brain Project
Simulations can help scientists get a full picture that otherwise is unattainable. “Another benefit is data completion,” added Jirsa, “in which incomplete data can be complemented by the model. In clinical settings, we can often measure only certain brain areas, but when linked to the brain model, we can enlarge the range of accessible brain regions and make better diagnostic predictions.”
With time, Jirsa’s team was able to move into patient-specific simulations. “We advanced from generic brain models to the ability to use a specific patient’s brain data, from measurements like MRI and others, to create individualized predictive models and simulations,” Jirsa explained. He and his team are working on this personalization technique to treat patients with epilepsy. According to the World Health Organization, about 50 million people worldwide suffer from epilepsy, a disorder that causes recurring seizures. While some epilepsy causes are known others remain an enigma, and many are hard to treat. For some patients whose epilepsy doesn’t respond to medications, removing part of the brain where seizures occur may be the only option. Understanding where in the patients’ brains seizures arise can give scientists a better idea of how to treat them and whether to use surgery versus medications.
“We apply such personalized models…to precisely identify where in a patient’s brain seizures emerge,” Jirsa explained. “This guides individual surgery decisions for patients for which surgery is the only treatment option.” He credits the HBP for the opportunity to develop this novel approach. “The personalization of our epilepsy models was only made possible by the Human Brain Project, in which all the necessary tools have been developed. Without the HBP, the technology would not be in clinical trials today.”
Personalized simulations can significantly advance treatments, predict the outcome of specific medical procedures and optimize them before actually treating patients. Jirsa is watching this happen firsthand in his ongoing research. “Our technology for creating personalized brain models is now used in a large clinical trial for epilepsy, funded by the French state, where we collaborate with clinicians in hospitals,” he explained. “We have also founded a spinoff company called VB Tech (Virtual Brain Technologies) to commercialize our personalized brain model technology and make it available to all patients.”
The Human Brain Project created a level of interconnectedness within the neuroscience research community that never existed before—a network not unlike the brain’s own.
Other experts believe it’s too soon to tell whether brain simulations could change epilepsy treatments. “The life cycle of developing treatments applicable to patients often runs over a decade,” Wang stated. “It is still too early to draw a clear link between HBP’s various project areas with patient care.” However, she admits that some studies built on the HBP-collected knowledge are already showing promise. “Researchers have used neuroscientific atlases and computational tools to develop activity-specific stimulation programs that enabled paraplegic patients to move again in a small-size clinical trial,” Wang said. Another intriguing study looked at simulations of Alzheimer’s in the brain to understand how it evolves over time.
Some challenges remain hard to overcome even with computer simulations. “The major challenge has always been the parameter explosion, which means that many different model parameters can lead to the same result,” Jirsa explained. An example of this parameter explosion could be two different types of neurodegenerative conditions, such as Parkinson’s and Huntington’s diseases. Both afflict the same area of the brain, the basal ganglia, which can affect movement, but are caused by two different underlying mechanisms. “We face the same situation in the living brain, in which a large range of diverse mechanisms can produce the same behavior,” Jirsa said. The simulations still have to overcome the same challenge.
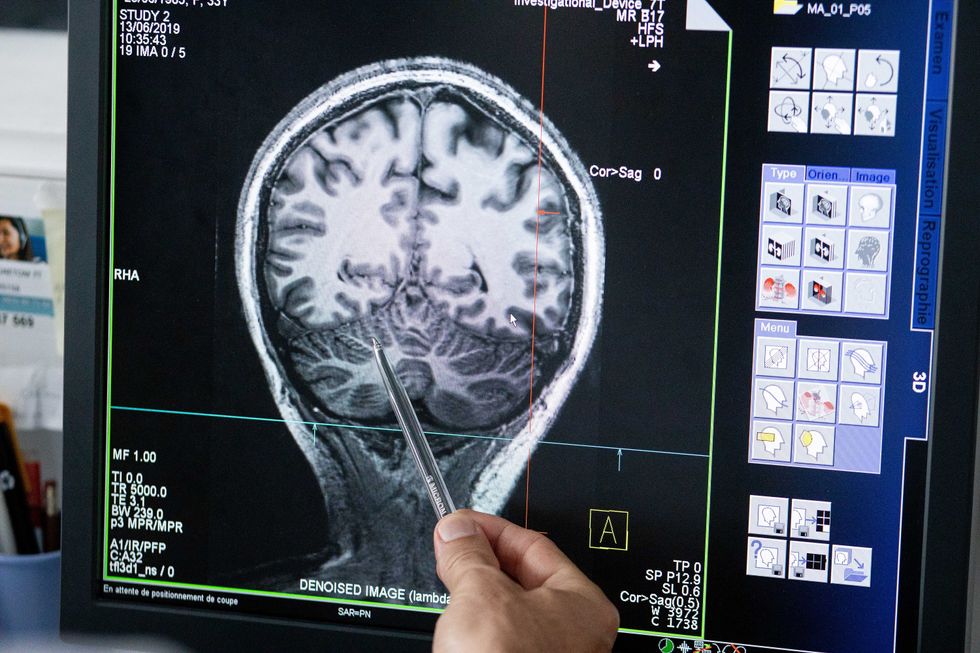
Understanding where in the patients’ brains seizures arise can give scientists a better idea of how to treat them and whether to use surgery versus medications.
The Human Brain Project
A network not unlike the brain’s own
Though the HBP will be closing this year, its legacy continues in various studies, spin-off companies, and its online platform, EBRAINS. “The HBP is one of the earliest brain initiatives in the world, and the 10-year long-term goal has united many researchers to collaborate on brain sciences with advanced computational tools,” Wang said. “Beyond the many research articles and projects collaborated on during the HBP, the online neuroscience research infrastructure EBRAINS will be left as a legacy even after the project ends.”
Those who worked within the HBP see the end of this project as the next step in neuroscience research. “Neuroscience has come closer to very meaningful applications through the systematic link with new digital technologies and collaborative work,” Jirsa stated. “In that way, the project really had a pioneering role.” It also created a level of interconnectedness within the neuroscience research community that never existed before—a network not unlike the brain’s own. “Interconnectedness is an important advance and prerequisite for progress,” Jirsa said. “The neuroscience community has in the past been rather fragmented and this has dramatically changed in recent years thanks to the Human Brain Project.”
According to its website, by 2023 HBP’s network counted over 500 scientists from over 123 institutions and 16 different countries, creating one of the largest multi-national research groups in the world. Even though the project hasn’t produced the in-silico brain as Markram envisioned it, the HBP created a communal mind with immense potential. “It has challenged us to think beyond the boundaries of our own laboratories,” Jirsa said, “and enabled us to go much further together than we could have ever conceived going by ourselves.”