How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
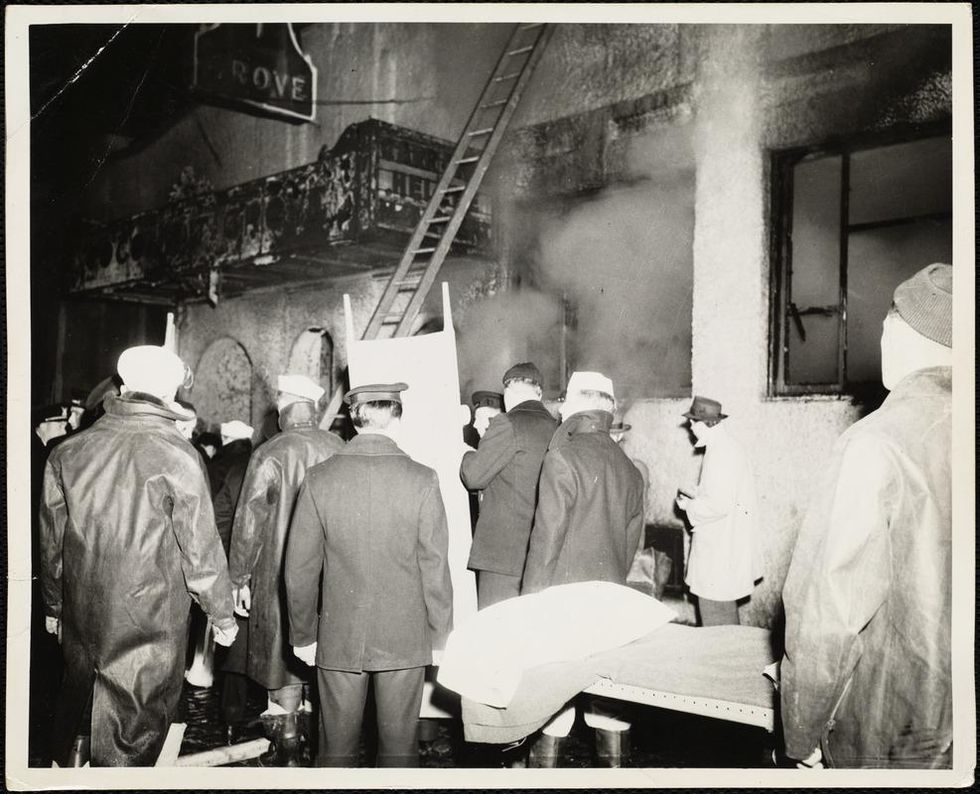
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
A woman gives a DNA sample at a Pheramor-sponsored event.
Brittany Barreto first got the idea to make a DNA-based dating platform nearly 10 years ago when she was in a college seminar on genetics. She joked that it would be called GeneHarmony.com.
Pheramor and startups, like DNA Romance and Instant Chemistry, both based in Canada, claim to match you to a romantic partner based on your genetics.
The idea stuck with her while she was getting her PhD in genetics at Baylor College of Medicine, and in March 2018, she launched Pheramor, a dating app that measures compatibility based on physical chemistry and what the company calls "social alignment."
"I wanted to use genetics and science to help people connect more. Our world is so hungry for connection," says Barreto, who serves as Pheramor's CEO.
With the direct-to-consumer genetic testing market booming, more and more companies are looking to capitalize on the promise of DNA-based services. Pheramor and startups, like DNA Romance and Instant Chemistry, both based in Canada, claim to match you to a romantic partner based on your genetics. It's an intriguing alternative to swiping left or right in hopes of finding someone you're not only physically attracted to but actually want to date. Experts say the science behind such apps isn't settled though.
For $40, Pheramor sends you a DNA kit to swab the inside of your cheek. After you mail in your sample, Pheramor analyzes your saliva for 11 different HLA genes, a fraction of the more than 200 genes that are thought to make up the human HLA complex. These genes make proteins that regulate the immune system by helping protect against invading pathogens.
It takes three to four weeks to get the results backs. In the meantime, users can still download the app and start using it before their DNA results are ready. The app asks users to link their social media accounts, which are fed into an algorithm that calculates a "social alignment." The algorithm takes into account the hashtags you use, your likes, check-ins, posts, and accounts you follow on Facebook, Twitter, and Instagram.
The DNA test results and social alignment algorithm are used to calculate a compatibility percentage between zero and 100. Barreto said she couldn't comment on how much of that score is influenced by the algorithm and how much comes from what the company calls genetic attraction. "DNA is not destiny," she says. "It's not like you're going to swab and I'll send you your soulmate."
Despite its name, Pheramor doesn't actually measure pheromones, chemicals released by animals that affect the behavior of others of the same species. That's because human pheromones have yet to be identified, though they've been discovered throughout the animal kingdom in moths, mice, rabbits, pigs, and many other insects and mammals. The HLA genes Pheramor analyzes instead are the human version of the major histocompatibility complex (MHC), a gene group found in many species.
The connection between HLA type and attraction goes back to the 1970s, when researchers found that inbred male mice preferred to mate with female mice with a different MHC rather than inbred female mice with similar immune system genes. The researchers concluded that this mating preference was linked to smell. The idea is that choosing a mate with different MHC genes gives animals an evolutionary advantage in terms of immune system defense.
The couples who had more dissimilar HLA types reported a more satisfied sex life and satisfied partnership, but it was a small effect.
In the 1990s, Swiss scientists wanted to see if body odor also had an effect on human attraction. In a famous experiment known as the "sweaty T-shirt study", they recruited 49 women to sniff sweaty, unwashed T-shirts from 44 men and put each in a box with a smelling hole and describe the odors of every shirt. The study found that women preferred the scents of T-shirts worn by men who were immunologically different from them compared to men whose HLA genes were similar to their own.
"The idea is, if you are very similar with your partner in HLA type then your offspring is similar in terms of HLA. This reduces your resistance against pathogens," says Illona Croy, a psychologist at the Technical University of Dresden who has studied HLA type in relation to sexual attraction in humans.
In a 2016 study Pheramor cites on its website, Croy and her colleagues tested the HLA types of 250 couples—all of them university students—and asked them how satisfied they were with their partnerships, with their sex lives, and with the odors of their partners. The couples who had more dissimilar HLA types reported a more satisfied sex life and satisfied partnership, but Croy cautions that it was a small effect. "It's not like they were super satisfied or not satisfied at all. It's a slight difference," she says.
Croy says we're much more likely to choose a partner based on appearance, sense of humor, intelligence and common interests.
Other studies have reported no preference for HLA difference in sexual attraction. Tristram Wyatt, a zoologist at the University of Oxford in the U.K. who studies animal pheromones, says it's been difficult to replicate the original T-shirt study. And one of the caveats of the original study is that women who were taking birth control pills preferred men who were more immunologically similar.
"Certainly, we learn to really like the smell of our partners," Wyatt says. "Whether it's the reason for choosing them in the first place, we really don't know."
Wyatt says he's skeptical of DNA-based dating apps because there are many subtypes of HLA genes, meaning there's a fairly low chance that your HLA type and your romantic partner's would be an exact match, anyway. It's why finding a suitable match for a bone marrow transplant is difficult; a donor's HLA type has to be the same as the recipient's.
"What it means is that since we're all different, it's hard statistically to say who the best match will be," he says.
DNA-based dating apps haven't yet gone mainstream, but some people seem willing to give them a try. Since Pheramor's launch a little over a year ago, about 10,000 people have signed up to use the app, about half of which have taken the DNA test, Barreto says. By comparison, an estimated 50 million people use Tinder, which has been around since 2012, and about 40 million people are on Bumble, which was released in 2014.
In April, Barreto launched a second service, this one for couples, called WeHaveChemistry.com. A $139 kit includes two genetic tests, one for you and your partner, and a detailed DNA report on your sexual compatibility.
Unlike the Phermor app, WeHaveChemistry doesn't provide users with a numeric combability score but instead makes personalized recommendations based on your genetic results. For instance, if the DNA test shows that your HLA genes are similar, Barreto says, "We might recommend pheromone colognes, working out together, or not showering before bed to get your juices running."
Despite her own research on HLA and sexual compatibility, Croy isn't sure how knowing HLA type will help couples. However, some researchers are doing studies on whether HLA types are related to certain cases of infertility, and this is where a genetic test might be very useful, says Croy.
"Otherwise, I think it doesn't matter whether we're HLA compatible or not," she says. "It might give you one possible explanation about why your sexual life isn't as satisfactory as it could be, but there are many other factors that play a role."
On left, the fungus (the whitish, fluffy material) of the Fungi Mutarium growing within the agar cups and degrading the plastic (the black/gray material in the center).
Between the ever-growing Great Pacific Garbage Patch, the news that over 90% of plastic isn't recycled, and the likely state of your personal trash can, it's clear that the world has a plastic problem.
Scientists around the world have continued to discover different types of fungus that can degrade specific types of plastic.
We now have 150 million tons of plastic in our oceans, according to estimates; by 2050, there could be more plastic than fish. And every new batch of trash compounds the issue: Plastic is notorious for its longevity and resistance to natural degradation.
The Lowdown
Enter the humble mushroom. In 2011, Yale students made headlines with the discovery of a fungus in Ecuador, Pestalotiopsis microspora, that has the ability to digest and break down polyurethane plastic, even in an air-free (anaerobic) environment—which might even make it effective at the bottom of landfills. Although the professor who led the research trip cautioned for moderate expectations, there's an undeniable appeal to the idea of a speedier, cleaner, side effect-free, and natural method of disposing of plastic.
A few years later, this particular application for fungus got a jolt of publicity from designer Katharina Unger, of LIVIN Studio, when she collaborated with the microbiology faculty at Utrecht University to create a project called the Fungi Mutarium. They used the mycelium—which is the threadlike, vegetative part of a mushroom—of two very common types of edible mushrooms, Pleurotus ostreatus (Oyster mushrooms) and Schizophyllum commune (Split gill mushrooms). Over the course of a few months, the fungi fully degraded small pieces of plastic while growing around pods of edible agar. The result? In place of plastic, a small mycelium snack.
Other researchers have continued to tackle the subject. In 2017, scientist Sehroon Khan and his research team at the World Agroforestry Centre in Kunming, China discovered another biodegrading fungus in a landfill in Islamabad, Pakistan: Aspergillus tubingensis, which turns out to be capable of colonizing polyester polyurethane (PU) and breaking it down it into smaller pieces within the span of two months. (PU often shows up in the form of packing foam—the kind of thing you might find cushioning a microwave or a new TV.)
Next Up
Utrecht University has continued its research, and scientists around the world have continued to discover different types of fungus that can degrade different, specific types of plastic. Khan and his team alone have discovered around 50 more species since 2017. They are currently working on finding the optimal conditions of temperature and environment for each strain of fungus to do its work.
Their biggest problem is perhaps the most common obstacle in innovative scientific research: Cash. "We are developing these things for large-scale," Khan says. "But [it] needs a lot of funding to get to the real application of plastic waste." They plan to apply for a patent soon and to publish three new articles about their most recent research, which might help boost interest and secure more grants.
Is there a way to get the fungi to work faster and to process bigger batches?
Khan's team is working on the breakdown process at this point, but researchers who want to continue in Unger's model of an edible end product also need to figure out how to efficiently and properly prepare the plastic input. "The fungi is sensitive to infection from bacteria," Unger says—which could turn it into a destructive mold. "This is a challenge for industrialization—[the] sterilization of the materials, and making the fungi resistant, strong, and faster-growing, to allow for a commercial process."
Open Questions
Whether it's Khan's polyurethane-chomping fungus or the edible agar pods from the Fungi Mutarium, the biggest question is still about scale. Both projects took several months to fully degrade a small amount of plastic. That's much shorter than plastic's normal lifespan, but still won't be enough to keep up with the global production of plastic. Is there a way to get the fungi to work faster and to process bigger batches?
We'd also need to figure out where these plastic recyclers would live. Could individuals keep a small compost-like heap, feeding in their own plastic and harvesting the mushrooms? Or could this be a replacement for local recycling centers?
There are still only these few small experiments for reference. But taken together, they suggest a fascinating future for waste disposal: An army of mycelium chewing quietly and methodically through our plastic bags and foam coffee cups—and potentially even creating a new food source along the way. We could have our trash and eat it, too.

