How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
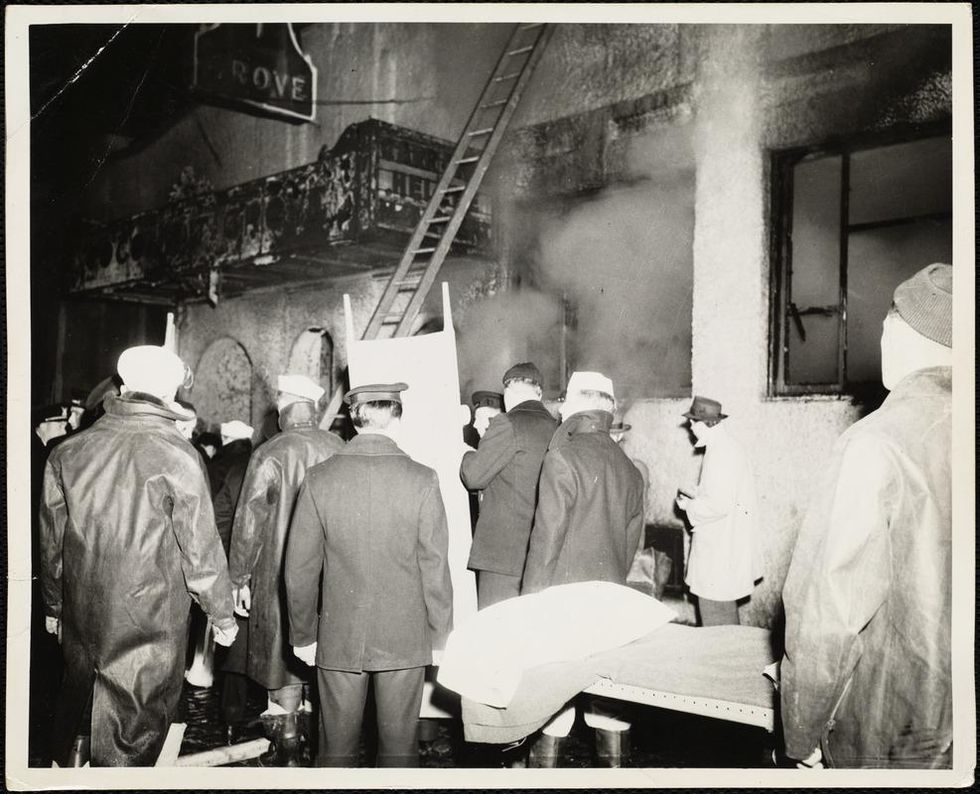
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
This Special Music Helped Preemie Babies’ Brains Develop
Listening to music helped preterm babies' brains develop, according to the results of a new Swiss study.
Move over, Baby Einstein: New research from Switzerland shows that listening to soothing music in the first weeks of life helps encourage brain development in preterm babies.
For the study, the scientists recruited a harpist and a new-age musician to compose three pieces of music.
The Lowdown
Children who are born prematurely, between 24 and 32 weeks of pregnancy, are far more likely to survive today than they used to be—but because their brains are less developed at birth, they're still at high risk for learning difficulties and emotional disorders later in life.
Researchers in Geneva thought that the unfamiliar and stressful noises in neonatal intensive care units might be partially responsible. After all, a hospital ward filled with alarms, other infants crying, and adults bustling in and out is far more disruptive than the quiet in-utero environment the babies are used to. They decided to test whether listening to pleasant music could have a positive, counterbalancing effect on the babies' brain development.
Led by Dr. Petra Hüppi at the University of Geneva, the scientists recruited Swiss harpist and new-age musician Andreas Vollenweider (who has collaborated with the likes of Carly Simon, Bryan Adams, and Bobby McFerrin). Vollenweider developed three pieces of music specifically for the NICU babies, which were played for them five times per week. Each track was used for specific purposes: To help the baby wake up; to stimulate a baby who was already awake; and to help the baby fall back asleep.
When they reached an age equivalent to a full-term baby, the infants underwent an MRI. The researchers focused on connections within the salience network, which determines how relevant information is, and then processes and acts on it—crucial components of healthy social behavior and emotional regulation. The neural networks of preemies who had listened to Vollenweider's pieces were stronger than preterm babies who had not received the intervention, and were instead much more similar to full-term babies.
Next Up
The first infants in the study are now 6 years old—the age when cognitive problems usually become diagnosable. Researchers plan to follow up with more cognitive and socio-emotional assessments, to determine whether the effects of the music intervention have lasted.
The first infants in the study are now 6 years old—the age when cognitive problems usually become diagnosable.
The scientists note in their paper that, while they saw strong results in the babies' primary auditory cortex and thalamus connections—suggesting that they had developed an ability to recognize and respond to familiar music—there was less reaction in the regions responsible for socioemotional processing. They hypothesize that more time spent listening to music during a NICU stay could improve those connections as well; but another study would be needed to know for sure.
Open Questions
Because this initial study had a fairly small sample size (only 20 preterm infants underwent the musical intervention, with another 19 studied as a control group), and they all listened to the same music for the same amount of time, it's still undetermined whether variations in the type and frequency of music would make a difference. Are Vollenweider's harps, bells, and punji the runaway favorite, or would other styles of music help, too? (Would "Baby Shark" help … or hurt?) There's also a chance that other types of repetitive sounds, like parents speaking or singing to their children, might have similar effects.
But the biggest question is still the one that the scientists plan to tackle next: Whether the intervention lasts as the children grow up. If it does, that's great news for any family with a preemie — and for the baby-sized headphone industry.
Couples Facing Fertility Treatments Should Beware of This
Couples facing infertility should be savvy about the add-on procedures offered by some fertility clinics.
When Jane Stein and her husband used in-vitro fertilization in 2001 to become pregnant with twins, her fertility clinic recommended using a supplemental procedure called intracytoplasmic sperm injection (ICSI), known in fertility lingo as "ix-see."
'Add-on' fertility procedures are increasingly coming under scrutiny for having a high cost and low efficacy rate.
During IVF, an egg and sperm are placed in a petri dish together with the hope that a sperm will seek out and fertilize the egg. With ICSI, doctors inject sperm directly into the egg.
Stein, whose name has been changed to protect her privacy, agreed to try it. Her twins are now 16, but while 17 years have gone by since that procedure, the efficacy of ICSI is still unclear. In other words, while Stein succeeded in having children, it may not have been because of ICSI. It may simply have been because she did IVF.
The American Society for Reproductive Medicine has concluded, "There are no data to support the routine use of ICSI for non-male factor infertility." That is, ICSI can help couples have a baby when the issue is male infertility. But when it's not, the evidence of its effectiveness is lacking. And yet the procedure is being used more and more, even when male infertility is not the issue. Some 40 percent of fertility treatments in Europe, Asia and the Middle East now use ICSI, according to a world report released in 2016 by the International Committee for Monitoring Assisted Reproductive Technologies. In the Middle East, the figure is actually 100 percent, the report said.
ICSI is just one of many supplemental procedures, or 'add-ons,' increasingly coming under scrutiny for having a high cost and low efficacy rate. They cost anywhere from a couple of hundred dollars to several thousand – ICSI costs $2,000 to $3,000 -- hiking up the price of what is already a very costly endeavor. And many don't even work. Worse, some actually cause harm.
It's no surprise couples use them. They promise to increase the chance of conceiving. For patients who desperately want a child, money is no object. The Human Fertilization and Embryology Authority (HFEA) in the U.K. found that some 74 percent of patients who received fertility treatments over the last two years were given at least one type of add-on. Now, fertility associations in the U.S. and abroad have begun issuing guidance about which add-ons are worth the extra cost and which are not.
"Many IVF add-ons have little in the way of conclusive evidence supporting their role in successful IVF treatment," said Professor Geeta Nargund, medical director of CREATE Fertility and Lead Consultant for reproductive medicine at St George's Hospital, London.
The HFEA has actually rated these add-ons, indicating which procedures are effective and safe. Some treatments were rated 'red' because they were considered to have insufficient evidence to justify their use. These include assisted hatching, which uses acid or lasers to make a hole in the surrounding layer of proteins to help the embryo hatch; intrauterine culture, where a device is inserted into the womb to collect and incubate the embryo; and reproductive immunology, which suppresses the body's natural immunity so that it accepts the embryo.
"Fertility care is a highly competitive market. In a private system, offering add-ons may discern you from your neighboring clinic."
For some treatments, the HFEA found there is evidence that they don't just fail to work, but can even be harmful. These procedures include ICSI used when male infertility is not at issue, as well as a procedure called endometrial scratching, where the uterus is scratched, not unlike what would happen with a biopsy, to stimulate the local uterine immune system.
And then for some treatments, there is conflicting evidence, warranting further research. These include artificial egg activation by calcium ionophore, elective freezing in all cycles, embryo glue, time-lapse imaging and pre-implantation genetic testing for abnormal chromosomes on day 5.
"Currently, there is very little evidence to suggest that many of the add-ons could increase success rates," Nargund said. "Indeed, the HFEA's assessment of add-on treatments concluded that none of the add-ons could be given a 'green' rating, due to a lack of conclusive supporting research."
So why do fertility clinics offer them?
"Fertility care is a highly competitive market," said Professor Hans Evers, editor-in-chief of the journal Human Reproduction. "In a private system, offering add-ons may discern you from your neighboring clinic. The more competition, the more add-ons. Hopefully the more reputable institutions will only offer add-ons (for free) in the context of a randomized clinical trial."
The only way for infertile couples to know which work and which don't is the guidance released by professional organizations like the ASRM, and through government regulation in countries that have a public health care system.
The problem is, infertile couples will sometimes do anything to achieve a pregnancy.
"They will stand on their heads if this is advocated as helpful. Someone has to protect them," Evers said.
In the Netherlands, where Evers is based, the national health care system tries to make the best use of the limited resources it has, so it makes sure the procedures it's funding actually work, Evers said.
"We have calculated that to serve a population of 17 million, we need 13 IVF clinics, and we have 13," he said. "We as professionals discuss and try to agree on the value of newly proposed add-ons, and we will implement only those that are proven effective and safe."
Likewise, in the U.K., there's been a lot of squawking about speculative add-ons because the government, or National Health Service, pays for them. In the U.S., it's private insurers or patients' own cash.
"The [U.K.] government takes a very close look at what therapies they are offering and what the evidence is around offering the therapy," said Alan Penzias, who chairs the Practice Committee of the ASRM. It wants to make sure the treatments it is funding are at least worth the money.
ICSI is a case in point. Originally intended for male infertility, it's now being applied across the board because fertility clinics didn't want couples to pay $10,000 to $15,000 and wind up with no embryos.
"It is so disastrous to have no fertilization whatsoever, clinics started to make this bargain with their patients, saying, 'Well, listen, even though it's not indicated, what we would like to do is to take half of your eggs and do the ICSI procedure, and half we'll do conventional insemination just to make sure,'" he said. "It's a disaster if you have no embryos, and now you're out 10 to 12 thousand dollars, so for a small added fee, we can do the injection just to guard against that."
In the Netherlands, the national health care system tries to make the best use of its limited resources, so it makes sure the procedures it's funding actually work.
Clinics offer it where they see lower rates of fertilization, such as with older women or in cases where induced ovulation results in just two or three eggs instead of, say, 13. Unfortunately, ICSI may result in a higher fertilization rate, but it doesn't result in a higher live birth rate, according to a study last year in Human Reproduction, so couples wind up paying for a procedure that doesn't even result in a child.
Private insurers in the U.S. are keen to it. Penzia, who is also an associate professor of obstetrics, gynecology and reproductive biology at Harvard Medical School and works as a reproductive endocrinology and infertility specialist at Boston IVF, said Massachusetts requires that insurers cover infertility treatments. But when he submits claims for ICSI, for instance, insurers now want to see two sperm counts and proof that the man has seen a urologist.
"They want to make sure we're doing it for male factor (infertility)," he said. "That's not unreasonable, because the insurance company is taking the burden of this."

