How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
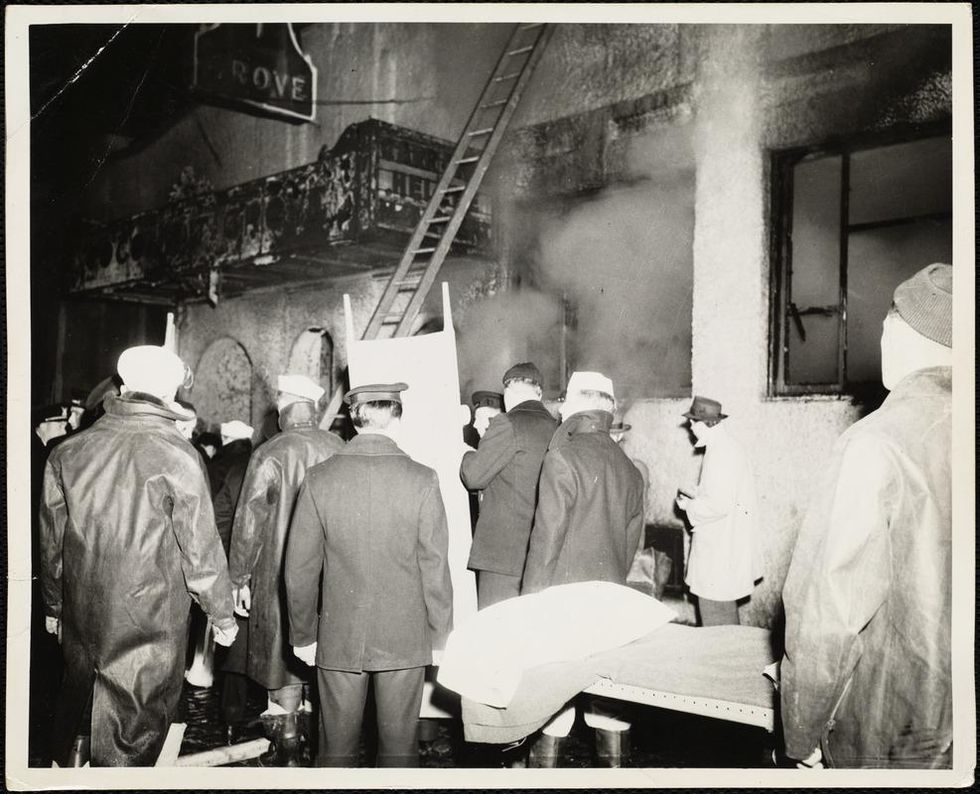
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
Study of the DNA double helix will lead to transformative medical care and increasingly urgent questions about how to responsibly handle genetic engineering technology.
The news last November that a rogue Chinese scientist had genetically altered the embryos of a pair of Chinese twins shocked the world. But although this use of advanced technology to change the human gene pool was premature, it was a harbinger of how genetic science will alter our healthcare, the way we make babies, the nature of the babies we make, and, ultimately, our sense of who and what we are as a species.
The healthcare applications of the genetics revolution are merely stations along the way to the ultimate destination.
But while the genetics revolution has already begun, we aren't prepared to handle these Promethean technologies responsibly.
By identifying the structure of DNA in the 1950s, Watson, Crick, Wilkins, and Franklin showed that the book of life was written in the DNA double helix. When the human genome project was completed in 2003, we saw how this book of human life could be transcribed. Painstaking research paired with advanced computational algorithms then showed what increasing numbers of genes do and how the genetic book of life can be read.
Now, with the advent of precision gene editing tools like CRISPR, we are seeing that the book of life -- and all biology -- can be re-written. Biology is being recognized as another form of readable, writable, and hackable information technology with we humans as the coders.
The impact of this transformation is being first experienced in our healthcare. Gene therapies including those extracting, re-engineering, then reintroducing a person's own cells enhanced into cancer-fighting supercells are already performing miracles in clinical trials. Thousands of applications have already been submitted to regulators across the globe for trials using gene therapies to address a host of other diseases.
Recently, the first gene editing of cells inside a person's body was deployed to treat the genetically relatively simple metabolic disorder Hunter syndrome, with many more applications to come. These new approaches are only the very first steps in our shift from the current system of generalized medicine based on population averages to precision medicine based on each patient's individual biology to predictive medicine based on AI-generated estimations of a person's future health state.

Jamie Metzl's groundbreaking new book, Hacking Darwin: Genetic Engineering and the Future of Humanity, explores how the genetic revolution is transforming our healthcare, the way we make babies, and the nature of and babies we make, what this means for each of us, and what we must all do now to prepare for what's coming.
This shift in our healthcare will ensure that millions and then billions of people will have their genomes sequenced as the foundation of their treatment. Big data analytics will then be used to compare at scale people's genotypes (what their genes say) to their phenotypes (how those genes are expressed over the course of their lives).
These massive datasets of genetic and life information will then make it possible to go far beyond the simple genetic analysis of today and to understand far more complex human diseases and traits influenced by hundreds or thousands of genes. Our understanding of this complex genetic system within the vaster ecosystem of our bodies and the environment around us will transform healthcare for the better and help us cure terrible diseases that have plagued our ancestors for millennia.
But as revolutionary as this challenge will be for medicine, the healthcare applications of the genetics revolution are merely stations along the way to the ultimate destination – a deep and fundamental transformation of our evolutionary trajectory as a species.
A first inkling of where we are heading can be seen in the direct-to-consumer genetic testing industry. Many people around the world have now sent their cheek swabs to companies like 23andMe for analysis. The information that comes back can tell people a lot about relatively simple genetic traits like carrier status for single gene mutation diseases, eye color, or whether they hate the taste of cilantro, but the information about complex traits like athletic predisposition, intelligence, or personality style today being shared by some of these companies is wildly misleading.
This will not always be the case. As the genetic and health data pools grow, analysis of large numbers of sequenced genomes will make it possible to apply big data analytics to predict some very complex genetic disease risks and the genetic components of traits like height, IQ, temperament, and personality style with increasing accuracy. This process, called "polygenic scoring," is already being offered in beta stage by a few companies and will become an ever bigger part of our lives going forward.
The most profound application of all this will be in our baby-making. Before making a decision about which of the fertilized eggs to implant, women undergoing in vitro fertilization can today elect to have a small number of cells extracted from their pre-implanted embryos and sequenced. With current technology, this can be used to screen for single-gene mutation diseases and other relatively simple disorders. Polygenic scoring, however, will soon make it possible to screen these early stage pre-implanted embryos to assess their risk of complex genetic diseases and even to make predictions about the heritable parts of complex human traits. The most intimate elements of being human will start feeling like high-pressure choices needing to be made by parents.
The limit of our imagination will become the most significant barrier to our recasting biology.
Adult stem cell technologies will then likely make it possible to generate hundreds or thousands of a woman's own eggs from her blood sample or skin graft. This would blow open the doors of reproductive possibility and allow parents to choose embryos with exceptional potential capabilities from a much larger set of options.
The complexity of human biology will place some limits to the extent of possible gene edits that might be made to these embryos, but all of biology, including our own, is extremely flexible. How else could all the diversity of life have emerged from a single cell nearly four billion years ago? The limit of our imagination will become the most significant barrier to our recasting biology.
But while we humans are gaining the powers of the gods, we aren't at all ready to use them.
The same tools that will help cure our worst afflictions, save our children, help us live longer, healthier, more robust lives will also open the door to potential abuses. Prospective parents with the best of intentions or governments with lax regulatory structures or aggressive ideas of how population-wide genetic engineering might be used to enhance national competitiveness or achieve some other goal could propel us into a genetic arms race that could undermine our essential diversity, dangerously divide societies, lead to dangerous, destabilizing, and potentially even deadly conflicts between us, and threaten our very humanity.
But while the advance of genetic technologies is inevitable, how it plays out is anything but. If we don't want the genetic revolution to undermine our species or lead to grave conflicts between genetic haves and have nots or between societies opting in and those opting out, now is the time when we need to make smart decisions based on our individual and collective best values. Although the technology driving the genetic revolution is new, the value systems we will need to optimize the benefits and minimize the harms of this massive transformation are ones we have been developing for thousands of years.
And while some very smart and well-intentioned scientists have been meeting to explore what comes next, it won't be enough for a few of even our wisest prophets to make decisions about the future of our species that will impact everyone. We'll also need smart regulations on both the national and international levels.
Every country will need to have its own regulatory guidelines for human genetic engineering based on both international best practices and the country's unique traditions and values. Because we are all one species, however, we will also ultimately need to develop guidelines that can apply to all of us.
As a first step toward making this possible, we must urgently launch a global, species-wide education effort and inclusive dialogue on the future of human genetic engineering that can eventually inform global norms that will need to underpin international regulations. This process will not be easy, but the alternative of an unregulated genetic arms race would be far worse.
The overlapping genomics and AI revolutions may seem like distant science fiction but are closer than you think. Far sooner than most people recognize, the inherent benefits of these technologies and competition between us will spark rapid adoption. Before that spark ignites, we have a brief moment to come together as a species like we never have before to articulate and translate into action the future we jointly envision. The north star of our best shared values can help us navigate the almost unimaginable opportunities and very real challenges that lie ahead.
Edible water bubble pods, called Ooho, made by Skipping Rock Labs. (Photo credit: Instagram account of Ooho water)
Here's something to chew on. Can a gulp of water help save the planet? If you're drinking *and* eating your water at the same time, the answer may be yes.
The tasteless packaging is made from brown seaweed that biodegrades naturally in four to six weeks.
The Lowdown
A start-up company called Skipping Rocks Lab has created a "water bubble" encased in an edible sachet that you can pop in your mouth whole. Or if you're not into swallowing it, you can tear off the edge, drink up, and toss the rest in a composter. The tasteless packaging is made from brown seaweed that biodegrades naturally in four to six weeks, whereas plastic water bottles can linger for hundreds of years.
The founders of the London-based company are determined to "make plastic packaging disappear." They had two foodie inspirations: molecular gastronomists and fruit. They tried to emulate the way chefs used edible membranes to encase bubbles of liquid to make things like fake caviar and fake egg yolks; and they also considered the peel of an orange or banana, which protects the tasty insides but can be composted.
The sachets can also contain other liquids that come in single-serve plastic containers -- think packets of condiments with takeout meals, specialty cocktails at parties, and especially single servings of water for sporting events. The London Marathon last month gave out the water bubble pods at a station along the route, using them to replace 200,000 plastic bottles that would have likely ended up first in the street, and ultimately in the ocean.
Next Up
The engineers and chemists at Skipping Rocks intend to lease their machines to others who can then manufacture their own sachets on-site to fill with whatever they desire. The new material, which is dubbed "Notpla" (not plastic), also has other applications beyond holding liquids. It can be used to replace the plastic lining in cardboard takeout boxes, for example. And the startup is working on additional materials to replace other types of ubiquitous plastic packaging, like the netting that encases garlic and onions, and the sachets that hold nails and screws.
Edible water bubbles may be the future of drinks at sporting events and festivals.
Open Questions
One hurdle is that the pods are not very hardy, so while they work fine to hand out along a marathon route, they wouldn't really be viable for a hiker to throw in her backpack. Another issue concerns the retail market: to be stable on a shelf, they'd have to be protected from all that handling, which brings us back to the problem the engineers tried to solve in the first place -- disposable packaging.
So while Skipping Rocks may not achieve their ultimate goal of ridding the world of plastic waste, a little progress can still go a long way. If edible water bubbles are the future of drinks at sporting events and festivals, the environment will certainly benefit from their presence -- and absence.