How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
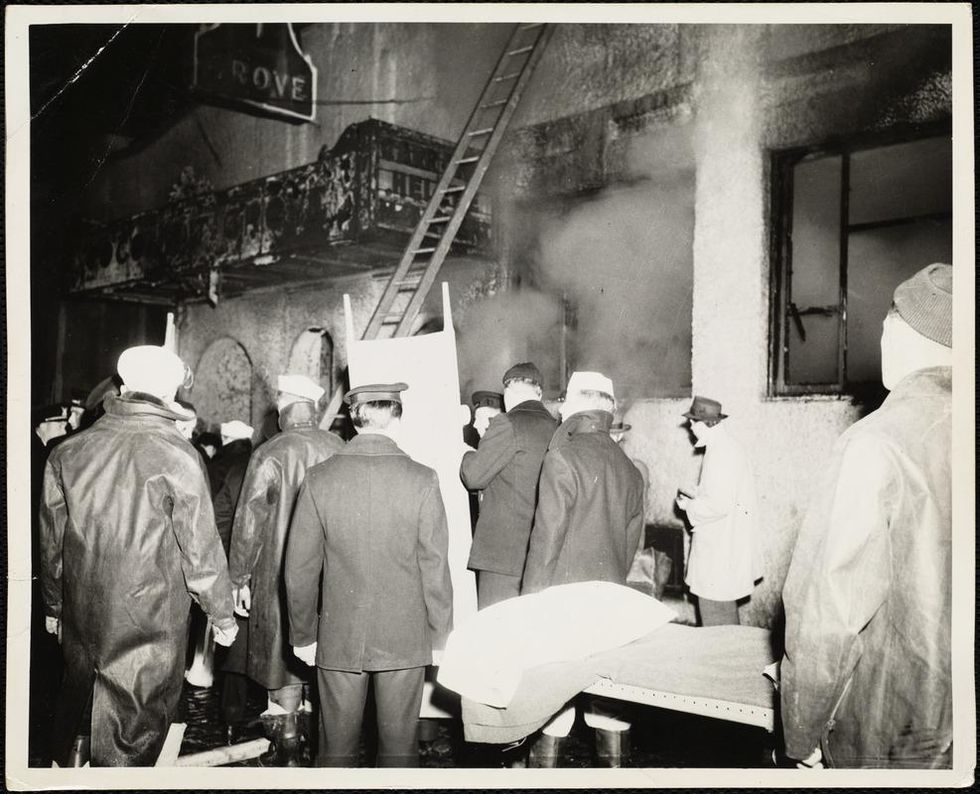
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
Six Questions about the Kids' COVID Vaccine, Answered by an Infectious Disease Doctor
The author, an infectious disease physician, pictured with his two daughters who are getting vaccinated against COVID-19.
I enthusiastically support the vaccination against COVID for children aged 5-11 years old. As an infectious disease doctor who took care of hundreds of COVID-19 patients over the past 20 months, I have seen the immediate and long-term consequences of COVID-19 on patients – and on their families. As a father of two daughters, I have lived through the fear and anxiety of protecting my kids at all cost from the scourges of the pandemic and worried constantly about bringing the virus home from work.
It is imperative that we vaccinate as many children in the community as possible. There are several reasons why. First children do get sick from COVID-19. Over the course of the pandemic in the U.S, more than 2 million children aged 5-11 have become infected, more than 8000 have been hospitalized, and more than 100 have died, making COVID one of the top 10 causes of pediatric deaths in this age group over the past year. Children are also susceptible to chronic consequences of COVID such as long COVID and multisystem inflammatory syndrome in children (MIS-C). Most studies demonstrate that 10-30% of children will develop chronic symptoms following COVID-19. These include complaints of brain fog, fatigue, trouble breathing, fever, headache, muscle and joint pains, abdominal pain, mood swings and even psychiatric disorders. Symptoms typically last from 4-8 weeks in children, with some reporting symptoms that persist for many months.
Second, children are increasingly recognized as vectors who can bring infection into the house, potentially transmitting infection to vulnerable household members. Finally, we have all seen the mayhem that results when one child in the classroom becomes infected with COVID and the other students get sent home to quarantine – across the U.S., more than 2000 schools have been affected this way.
We now have an extraordinarily effective vaccine with more than 90 percent efficacy at preventing symptomatic infection. Vaccinating children will boost our countrywide vaccination rate which is trailing many countries after an early start. Nevertheless, there are still many questions and concerns that parents have as the vaccine gets rolled out. I will address six of them here.
"Novel Vaccine Technology"
Even though this is a relatively new vaccine, the technology is not new. Scientists had worked on mRNA vaccines for decades prior to the COVID mRNA vaccine breakthrough. Furthermore, experience with the Pfizer COVID vaccine is rapidly growing. By now it has been more than a year and a half since the Pfizer trials began in March 2020, and more than 7 billion doses have already been administered globally, including in 13.7 million adolescents in the U.S. alone.
"Will This Vaccine Alter My Child's DNA?"
No. This is not how mRNA works. DNA is present in the cell's nucleus. The mRNA only stays in the outside cytoplasm, gets destroyed and never enters the inner sanctum of the nucleus. Furthermore, for the mRNA to be ever integrated into DNA, it requires a special enzyme called reverse transcriptase which humans don't have. Proteins (that look like the spike proteins on SARS-CoV-2) are made directly from this mRNA message without involvement of our DNA at any time. Pieces of spike proteins get displayed on the outside of our cells and our body makes protective antibodies that then protects us handily against the future real virus if it were ever to enter our (or our children's) bodies. Our children's DNA or genes can never be affected by an mRNA vaccine.
"Lack of Info on Long-Term Side Effects"
Unlike medications that are taken daily or periodically and can build up over time, the mRNA in the Pfizer vaccine is evanescent. It literally is just the messenger (that is what the "m" in mRNA stands for) and the messenger quickly disappears. mRNA is extremely fragile and easily inactivated – that's why we need to encase it in a special fatty bubble and store the vaccines at extremely cold temperatures. Our cells break down and destroy the mRNA within a few days after receiving the instructions to make the virus spike proteins. The presence of these fragments of the virus (note this is not "live" virus) prompts our immune system to generate protective antibodies to the real thing. Our bodies break down mRNA all the time in normal cellular processes – this is nothing new.
What the transience of the delivery system means is that most of the effects of the mRNA vaccines are expected to be more immediate (sore arm, redness at the site, fever, chills etc.), with no long-term side effects anticipated. A severe allergic response has been reported to occur in some generally within the first 15 minutes, is very rare, and everyone gets observed for that as part of standard vaccine administration. Even with the very uncommon complication of myocarditis (inflammation of the heart muscle) and pericarditis (inflammation of the lining of the heart) seen primarily in young men under the age of 30 following mRNA vaccines, these typically happen within days to 2 weeks and many return to work or school in days. In the 70-year history of pediatric (and adult vaccines), dangerous complications happen in the first two months. There have been millions of adolescents as young as 12 years and thousands in the initial trial of children aged 5-11 who have already received the vaccine and are well beyond the two-month period of observation. There is no biological reason to believe that younger children will have a different long-term side effect profile compared to adolescents or adults.
"Small Sample Size in Kids and the Trial Design"
Although the Pfizer trial in children aged 5-11 was relatively small, it was big enough to give us statistical confidence in assessing safety and efficacy outcomes. Scientists spend a lot of time determining the right sample size of a study during the design phase. On one hand, you want to conduct the study efficiently so that resources are used in a cost-effective way and that you get a timely answer, especially in a fast-moving pandemic. On the other hand, you want to make sure you have enough sample size so that you can answer the question confidently as to whether the intervention works and whether there are adverse effects. The more profound the effect size of the intervention (in this case the vaccine), the fewer the numbers of children needed in the trials.
Statistics help investigators determine whether the results seen would have appeared by chance or not. In this case, the effect was real and impressive. Over 3,000 children around the world have received the vaccines through the trials alone with no serious side effects detected. The first press release reported that the immune response in children aged 5-11 was similar (at one-third the vaccine dose) to the response in the comparator group aged 16-25 years old. Extrapolating clinical efficacy results from immune response measurements ("immunobridging" study) would already have been acceptable if this was the only data. This is a standard trial design for many pediatric vaccines. Vaccines are first tested in the lab, followed by animals then adults. Only when deemed safe in adults and various regulatory bodies have signed off, do the pediatric vaccine trials commence.
Because children's immune systems and bodies are in a constant state of development, the vaccines must be right-sized. Investigators typically conduct "age de-escalation" studies in various age groups. The lowest dose is first tried so see if that is effective, then the dose is increased gradually as needed. Immune response is the easiest, safest and most efficient way to test the efficacy of pediatric vaccines. This is a typical size and design of a childhood vaccine seeking regulatory approval. There is no reason to think that the clinical efficacy would be any different in children vs. adults for a given antibody response, given the experience already in the remainder of the population, including older children and adolescents. Although this was primarily designed as an "immunobridging" study, the initial immunologic response data was followed by real clinical outcomes in this population. Reporting on the outcomes of 2,268 children in the randomized controlled trial, the vaccine was 90.7% effective at preventing symptomatic infection.
"Fear of Myocarditis"
Myocarditis (inflammation of the heart muscle) and pericarditis (inflammation of the lining of the heart) have been associated with receipt of the mRNA vaccines, particularly among male adolescents and young adults, typically within a few days after receiving the second dose. But this is very rare. For every million vaccine recipients, you would expect 41 cases in males, and 4 cases in females aged 12-29 years-old. The risk in older age groups is substantially lower. It is important to recognize that the risk of myocarditis associated with COVID is substantially higher. Patients present with new chest pain, shortness of breath, or palpitations after receiving an mRNA vaccine (more common after the second dose). But outcomes are good if associated with the vaccine. Most respond well to treatment and resolve symptoms within a week. There have been no deaths associated with vaccine-associated myocarditis.
In contrast, COVID-associated myocarditis has been associated with more severe cases as well as other complications including chronic symptoms of long COVID. The risk of myocarditis is likely related to vaccine dose, so the fact that one-third the dose of the vaccine will be used in the 5-11 year-olds is expected to correspond to a lower risk of myocarditis. At the lower dose given to younger kids, there has been a lower incidence of adverse effects reported compared to older children and adults who received the full dose. In addition, baseline rates of myocarditis not associated with vaccination are much lower in children ages 5-11 years than in older children, so the same may hold true for vaccine-associated myocarditis cases. This is because myocarditis is associated with sex hormones (particularly testosterone) that surge during puberty. In support of this, the incidence of vaccine-associated myocarditis is lower in 12–15-year-old boys, compared to those who were older than 16 years old. There were no cases of myocarditis reported in the experience to date of 5–11-year-old children in the trials, although the trial was too small to pick up on such a rare effect.
"Optimal Dose Spacing Interval: Longer Than 3 Weeks?"
There is a biologic basis for increasing the interval between vaccine doses in general. Priming the immune system with the first shot and then waiting gives the second shot a better chance of prompting a secondary immune reaction that results in a more durable response (with more T cell driven immune memory). One study from the U.K. showed that the antibody response in people over 80 was more than 3 times higher if they delayed the second dose to after 12 weeks for the Pfizer vaccine instead of the 3 weeks studied in trials. In a study of 503 British health care workers, there were twice as many neutralizing antibodies produced in a longer interval group (6-14 weeks) versus a shorter interval group (3-4 weeks) between doses. However, the safety and efficacy with longer intervals has not been evaluated in the pediatric or other COVID vaccine trials.
In the U.S., the C.D.C. reported that 88 percent of counties are at a "high" or "substantial" level of community transmission. Also, Europe is already experiencing a winter surge of infections that may predict more U.S. winter cases as international travel reopens. During a time of high community virus burden with a highly transmissible Delta variant, relying on one dose of vaccine for several more weeks until the second may leave many more susceptible to infection while waiting. One study from England showed that one dose of the Pfizer vaccine was only 33% protective against symptomatic Delta infection in contrast to 50% for the Alpha variant in adults. There has been no corollary information in children but we would expect less protection in general from one vaccine dose vs. two. This is a particularly important issue with the upcoming holiday season when an increased number of families will travel. Some countries such as the U.K. and Norway have proceeded with only offering older than 12 year-olds one dose of vaccine rather than two, but this was before the current European surge which may change the risk-benefit calculus. There are no plans to only offer one vaccine dose in the U.S. at this time. However a lower dose of the vaccine will likely be studied in the future for adolescents aged 12-15.
For parents worried about the potential risk of adverse effects of two doses of vaccines in their children, it is reasonable to wait 6-12 weeks for the second shot but it all depends on your risk-benefit calculus. There is biological plausibility to pursue this strategy. Although there is no pediatric-specific data to draw from, a longer interval may lengthen immune memory and potentially decrease the risk of myocarditis, particularly in boys. There may only be partial benefit in eliciting protective antibodies after one vaccine dose but only 2-4% of children are hospitalized with COVID once infected, with risk of severe illness increasing if they have comorbidities.
There are also some data indicating that 40% of children have already been exposed to infection naturally and may not need further protection after one shot. However, this percentage is likely a large overestimation given the way the data was collected. Using antibody tests to ascertain previous infection in children may be problematic for several reasons: uncertainty regarding duration of protection, variability in symptoms in children with most having very mild symptoms, and the lack of standardization of antibody tests in general. Overall, if the child has medical comorbidities such as diabetes, parents are planning to travel with their children, if local epidemiology shows increasing cases, and if there are elderly or immunocompromised individuals in the household, I would vaccinate children with two doses as per the original recommended schedule.
Bottom line: Given the time of the year and circulating Delta, I would probably stick with the recommended 3-week interval between doses for now for most children. But if parents choose a longer interval between the first and second dose for their children, I wouldn't worry too much about it. Better to be vaccinated - even if slowly, over time -- than not at all.
Food Poisoning Sickens Millions a Year. Now, a Surprising Weapon Is Helping Protect Against Contamination.
Phages, which are harmless viruses that destroy specific bacteria, are becoming useful tools to protect our food supply.
Every year, one in seven people in America comes down with a foodborne illness, typically caused by a bacterial pathogen, including E.Coli, listeria, salmonella, or campylobacter. That adds up to 48 million people, of which 120,000 are hospitalized and 3000 die, according to the Centers for Disease Control. And the variety of foods that can be contaminated with bacterial pathogens is growing too. In the 20th century, E.Coli and listeria lurked primarily within meat. Now they find their way into lettuce, spinach, and other leafy greens, causing periodic consumer scares and product recalls. Onions are the most recent suspected culprit of a nationwide salmonella outbreak.
Some of these incidents are almost inevitable because of how Mother Nature works, explains Divya Jaroni, associate professor of animal and food sciences at Oklahoma State University. These common foodborne pathogens come from the cattle's intestines when the animals shed them in their manure—and then they get washed into rivers and lakes, especially in heavy rains. When this water is later used to irrigate produce farms, the bugs end up on salad greens. Plus, many small farms do both—herd cattle and grow produce.
"Unfortunately for us, these pathogens are part of the microflora of the cows' intestinal tract," Jaroni says. "Some farmers may have an acre or two of cattle pastures, and an acre of a produce farm nearby, so it's easy for this water to contaminate the crops."
Food producers and packagers fight bacteria by potent chemicals, with chlorine being the go-to disinfectant. Cattle carcasses, for example, are typically washed by chlorine solutions as the animals' intestines are removed. Leafy greens are bathed in water with added chlorine solutions. However, because the same "bath" can be used for multiple veggie batches and chlorine evaporates over time, the later rounds may not kill all of the bacteria, sparing some. The natural and organic producers avoid chlorine, substituting it with lactic acid, a more holistic sanitizer, but even with all these efforts, some pathogens survive, sickening consumers and causing food recalls. As we farm more animals and grow more produce, while also striving to use fewer chemicals and more organic growing methods, it will be harder to control bacteria's spread.
"It took us a long time to convince the FDA phages were safe and efficient alternatives. But we had worked with them to gather all the data they needed, and the FDA was very supportive in the end."
Luckily, bacteria have their own killers. Called bacteriophages, or phages for short, they are viruses that prey on bacteria only. Under the electron microscope, they look like fantasy spaceships, with oblong bodies, spider-like legs and long tails. Much smaller than a bacterium, phages pierce the microbes' cells with their tails, sneak in and begin multiplying inside, eventually bursting the microbes open—and then proceed to infect more of them. The best part is that these phages are harmless to humans. Moreover, recent research finds that millions of phages dwell on us and in us—in our nose, throat, skin and gut, protecting us from bacterial infections as part of our healthy microbiome. A recent study suggested that we absorb about 30 billion phages into our bodies on a daily basis. Now, ingeniously, they are starting to be deployed as anti-microbial agents in the food industry.
A Maryland-based phage research company called Intralytix is doing just that. Founded by Alexander Sulakvelidze, a microbiologist and epidemiologist who came to the United States from Tbilisi, the capital of Georgia, Intralytix makes and sells five different FDA-approved phage cocktails that work against some of the most notorious food pathogens: ListShield for Listeria, SalmoFresh for Salmonella, ShigaShield for Shigella, another foodborne bug, and EcoShield for E.coli, including the infamous strain that caused the Jack in the Box outbreak in 1993 that killed four children and sickened 732 people across four states. Earlier this month, the FDA granted its approval to yet another Intralytix phage for managing Campylobacter contamination, named CampyShield. "We call it safety by nature," Sulakvelidze says.

Intralytix grows phages inside massive 1500-liter fermenters, feeding them bacterial "fodder."
Photo credit: Living Radiant Photography
Phage preparations are relatively straightforward to make. In nature, phages thrive in any body of water where bacteria live too, including rivers, lakes and bays. "I can dip a bucket into the Chesapeake Bay, and it will be full of all kinds of phages," Sulakvelidze says. "Sewage is another great place to look for specific phages of interest, because it's teeming with all sorts of bacteria—and therefore the viruses that prey on them." In lab settings, Intralytix grows phages inside massive 1500-liter fermenters, feeding them bacterial "fodder." Once phages multiply enough, they are harvested, dispensed into containers and shipped to food producers who have adopted this disinfecting practice into their preparation process. Typically, it's done by computer-controlled sprayer systems that disperse mist-like phage preparations onto the food.
Unlike chemicals like chlorine or antibiotics, which kill a wide spectrum of bacteria, phages are more specialized, each feeding on specific microbial species. A phage that targets salmonella will not prey on listeria and vice versa. So food producers may sometimes use a combo of different phage preparations. Intralytix is continuously researching and testing new phages. With a contract from the National Institutes of Health, Intralytix is expanding its automated high-throughput robot that tests which phages work best against which bacteria, speeding up the development of the new phage cocktails.
Phages have other "talents." In her recent study, Jaroni found that phages have the ability to destroy bacterial biofilms—colonies of microorganisms that tend to grow on surfaces of the food processing equipment, surrounding themselves with protective coating that even very harsh chemicals can't crack. "Phages are very clever," Jaroni says. "They produce enzymes that target the biofilms, and once they break through, they can reach the bacteria."
Convincing the FDA that phages were safe to use on food products was no easy feat, Sulakvelidze says. In his home country of Georgia, phages have been used as antimicrobial remedies for over a century, but the FDA was leery of using viruses as food safety agents. "It took us a long time to convince the FDA phages were safe and efficient alternatives," Sulakvelidze says. "But we had worked with them to gather all the data they needed, and the FDA was very supportive in the end." The agency had granted Intralytix its first approval in 2006, and over the past 10 years, the company's sales increased by over 15-fold. "We currently sell to about 40 companies and are in discussions with several other large food producers," Sulakvelidze says. One indicator that the industry now understands and appreciates the science of phages was that his company was ranked as Top Food Safety Provider in 2021 by Food and Beverage Technology Review, he adds. Notably, phage sprays are kosher, halal and organic-certified.
Intralytix's phage cocktails to safeguard food from bacteria are approved for consumers in addition to food producers, but currently the company sells to food producers only. Selling retail requires different packaging like easy-to-use spray bottles and different marketing that would inform people about phages' antimicrobial qualities. But ultimately, giving people the ability to remove pathogens from their food with probiotic phage sprays is the goal, Sulakvelidze says.
It's not the company's only goal. Now Intralytix is going a step further, investigating phages' probiotic and therapeutic abilities. Because phages are highly specialized in the bacteria they target, they can be used to treat infections caused by specific pathogens while leaving the beneficial species of our microbiome intact. In an ongoing clinical trial with Mount Sinai, Intralytix is now investigating a potential phage treatment against a certain type of E. coli for patients with Crohn's disease, and is about to start another clinical trial for treating bacterial dysentery.
"Now that we have proved that phages are safe and effective against foodborne bacteria," Sulakvelidze says, "we are going to demonstrate their potential in therapeutic applications."
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

