How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
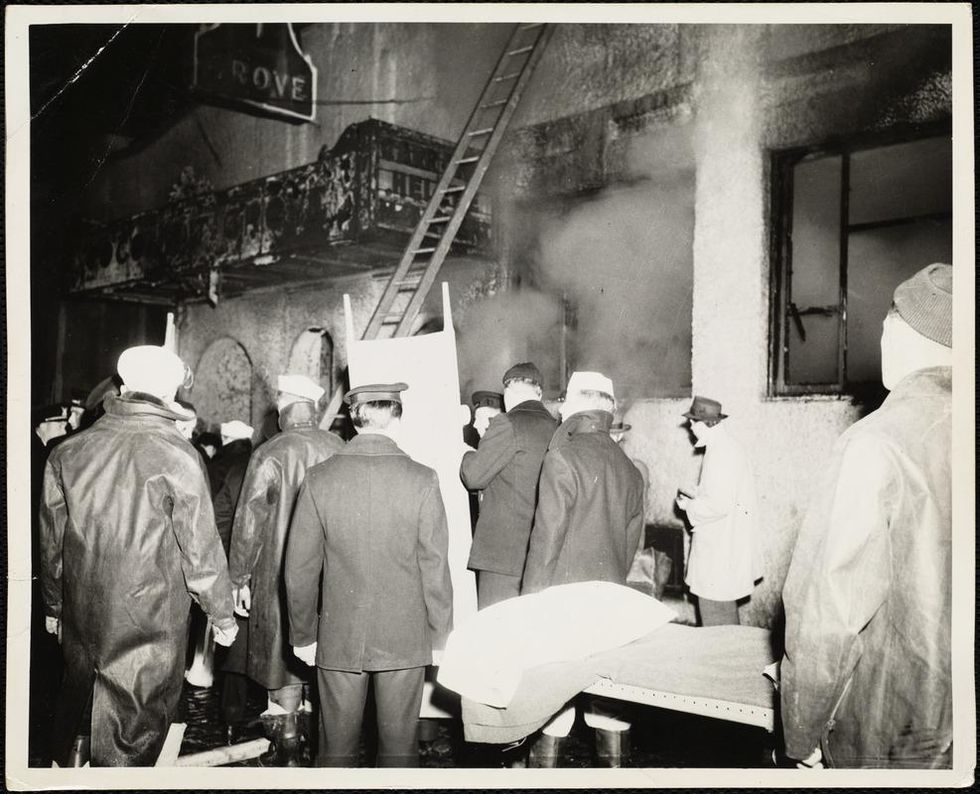
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
Some hospitals are pioneers in ditching plastic, turning green
In the U.S., hospitals generate an estimated 6,000 tons of waste per day. A few clinics are leading the way in transitioning to clean energy sources.
This is part 2 of a three part series on a new generation of doctors leading the charge to make the health care industry more sustainable - for the benefit of their patients and the planet. Read part 1 here and part 3 here.
After graduating from her studies as an engineer, Nora Stroetzel ticked off the top item on her bucket list and traveled the world for a year. She loved remote places like the Indonesian rain forest she reached only by hiking for several days on foot, mountain villages in the Himalayas, and diving at reefs that were only accessible by local fishing boats.
“But no matter how far from civilization I ventured, one thing was already there: plastic,” Stroetzel says. “Plastic that would stay there for centuries, on 12,000 foot peaks and on beaches several hundred miles from the nearest city.” She saw “wild orangutans that could be lured by rustling plastic and hermit crabs that used plastic lids as dwellings instead of shells.”
While traveling she started volunteering for beach cleanups and helped build a recycling station in Indonesia. But the pivotal moment for her came after she returned to her hometown Kiel in Germany. “At the dentist, they gave me a plastic cup to rinse my mouth. I used it for maybe ten seconds before it was tossed out,” Stroetzel says. “That made me really angry.”
She decided to research alternatives for plastic in the medical sector and learned that cups could be reused and easily disinfected. All dentists routinely disinfect their tools anyway and, Stroetzel reasoned, it wouldn’t be too hard to extend that practice to cups.
It's a good example for how often plastic is used unnecessarily in medical practice, she says. The health care sector is the fifth biggest source of pollution and trash in industrialized countries. In the U.S., hospitals generate an estimated 6,000 tons of waste per day, including an average of 400 grams of plastic per patient per day, and this sector produces 8.5 percent of greenhouse gas emissions nationwide.
“Sustainable alternatives exist,” Stroetzel says, “but you have to painstakingly look for them; they are often not offered by the big manufacturers, and all of this takes way too much time [that] medical staff simply does not have during their hectic days.”
When Stroetzel spoke with medical staff in Germany, she found they were often frustrated by all of this waste, especially as they took care to avoid single-use plastic at home. Doctors in other countries share this frustration. In a recent poll, nine out of ten doctors in Germany said they’re aware of the urgency to find sustainable solutions in the health industry but don’t know how to achieve this goal.
After a year of researching more sustainable alternatives, Stroetzel founded a social enterprise startup called POP, short for Practice Without Plastic, together with IT expert Nicolai Niethe, to offer well-researched solutions. “Sustainable alternatives exist,” she says, “but you have to painstakingly look for them; they are often not offered by the big manufacturers, and all of this takes way too much time [that] medical staff simply does not have during their hectic days.”
In addition to reusable dentist cups, other good options for the heath care sector include washable N95 face masks and gloves made from nitrile, which waste less water and energy in their production. But Stroetzel admits that truly making a medical facility more sustainable is a complex task. “This includes negotiating with manufacturers who often package medical materials in double and triple layers of extra plastic.”
While initiatives such as Stroetzel’s provide much needed information, other experts reason that a wholesale rethinking of healthcare is needed. Voluntary action won’t be enough, and government should set the right example. Kari Nadeau, a Stanford physician who has spent 30 years researching the effects of environmental pollution on the immune system, and Kenneth Kizer, the former undersecretary for health in the U.S. Department of Veterans Affairs, wrote in JAMA last year that the medical industry and federal agencies that provide health care should be required to measure and make public their carbon footprints. “Government health systems do not disclose these data (and very rarely do private health care organizations), unlike more than 90% of the Standard & Poor’s top 500 companies and many nongovernment entities," they explained. "This could constitute a substantial step toward better equipping health professionals to confront climate change and other planetary health problems.”
Compared to the U.K., the U.S. healthcare industry lags behind in terms of measuring and managing its carbon footprint, and hospitals are the second highest energy user of any sector in the U.S.
Kizer and Nadeau look to the U.K. National Health Service (NHS), which created a Sustainable Development Unit in 2008 and began that year to conduct assessments of the NHS’s carbon footprint. The NHS also identified its biggest culprits: Of the 2019 footprint, with emissions totaling 25 megatons of carbon dioxide equivalent, 62 percent came from the supply chain, 24 percent from the direct delivery of care, 10 percent from staff commute and patient and visitor travel, and 4 percent from private health and care services commissioned by the NHS. From 1990 to 2019, the NHS has reduced its emission of carbon dioxide equivalents by 26 percent, mostly due to the switch to renewable energy for heat and power. Meanwhile, the NHS has encouraged health clinics in the U.K. to install wind generators or photovoltaics that convert light to electricity -- relatively quick ways to decarbonize buildings in the health sector.
Compared to the U.K., the U.S. healthcare industry lags behind in terms of measuring and managing its carbon footprint, and hospitals are the second highest energy user of any sector in the U.S. “We are already seeing patients with symptoms from climate change, such as worsened respiratory symptoms from increased wildfires and poor air quality in California,” write Thomas B. Newman, a pediatrist at the University of California, San Francisco, and UCSF clinical research coordinator Daisy Valdivieso. “Because of the enormous health threat posed by climate change, health professionals should mobilize support for climate mitigation and adaptation efforts.” They believe “the most direct place to start is to approach the low-lying fruit: reducing healthcare waste and overuse.”
In addition to resulting in waste, the plastic in hospitals ultimately harms patients, who may be even more vulnerable to the effects due to their health conditions. Microplastics have been detected in most humans, and on average, a human ingests five grams of microplastic per week. Newman and Valdivieso refer to the American Board of Internal Medicine's Choosing Wisely program as one of many initiatives that identify and publicize options for “safely doing less” as a strategy to reduce unnecessary healthcare practices, and in turn, reduce cost, resource use, and ultimately reduce medical harm.
A few U.S. clinics are pioneers in transitioning to clean energy sources. In Wisconsin, the nonprofit Gundersen Health network became the first hospital to cut its reliance on petroleum by switching to locally produced green energy in 2015, and it saved $1.2 million per year in the process. Kaiser Permanente eliminated its 800,000 ton carbon footprint through energy efficiency and purchasing carbon offsets, reaching a balance between carbon emissions and removing carbon from the atmosphere in 2020, the first U.S. health system to do so.
Cleveland Clinic has pledged to join Kaiser in becoming carbon neutral by 2027. Realizing that 80 percent of its 2008 carbon emissions came from electricity consumption, the Clinic started switching to renewable energy and installing solar panels, and it has invested in researching recyclable products and packaging. The Clinic’s sustainability report outlines several strategies for producing less waste, such as reusing cases for sterilizing instruments, cutting back on materials that can’t be recycled, and putting pressure on vendors to reduce product packaging.
The Charité Berlin, Europe’s biggest university hospital, has also announced its goal to become carbon neutral. Its sustainability managers have begun to identify the biggest carbon culprits in its operations. “We’ve already reduced CO2 emissions by 21 percent since 2016,” says Simon Batt-Nauerz, the director of infrastructure and sustainability.
The hospital still emits 100,000 tons of CO2 every year, as much as a city with 10,000 residents, but it’s making progress through ride share and bicycle programs for its staff of 20,000 employees, who can get their bikes repaired for free in one of the Charité-operated bike workshops. Another program targets doctors’ and nurses’ scrubs, which cause more than 200 tons of CO2 during manufacturing and cleaning. The staff is currently testing lighter, more sustainable scrubs made from recycled cellulose that is grown regionally and requires 80 percent less land use and 30 percent less water.

The Charité hospital in Berlin still emits 100,000 tons of CO2 every year, but it’s making progress through ride share and bicycle programs for its staff of 20,000 employees.
Wiebke Peitz | Specific to Charité
Anesthesiologist Susanne Koch spearheads sustainability efforts in anesthesiology at the Charité. She says that up to a third of hospital waste comes from surgery rooms. To reduce medical waste, she recommends what she calls the 5 Rs: Reduce, Reuse, Recycle, Rethink, Research. “In medicine, people don’t question the use of plastic because of safety concerns,” she says. “Nobody wants to be sued because something is reused. However, it is possible to reduce plastic and other materials safely.”
For instance, she says, typical surgery kits are single-use and contain more supplies than are actually needed, and the entire kit is routinely thrown out after the surgery. “Up to 20 percent of materials in a surgery room aren’t used but will be discarded,” Koch says. One solution could be smaller kits, she explains, and another would be to recycle the plastic. Another example is breathing tubes. “When they became scarce during the pandemic, studies showed that they can be used seven days instead of 24 hours without increased bacteria load when we change the filters regularly,” Koch says, and wonders, “What else can we reuse?”
In the Netherlands, TU Delft researchers Tim Horeman and Bart van Straten designed a method to melt down the blue polypropylene wrapping paper that keeps medical instruments sterile, so that the material can be turned it into new medical devices. Currently, more than a million kilos of the blue paper are used in Dutch hospitals every year. A growing number of Dutch hospitals are adopting this approach.
Another common practice that’s ripe for improvement is the use of a certain plastic, called PVC, in hospital equipment such as blood bags, tubes and masks. Because of its toxic components, PVC is almost never recycled in the U.S., but University of Michigan researchers Danielle Fagnani and Anne McNeil have discovered a chemical process that can break it down into material that could be incorporated back into production. This could be a step toward a circular economy “that accounts for resource inputs and emissions throughout a product’s life cycle, including extraction of raw materials, manufacturing, transport, use and reuse, and disposal,” as medical experts have proposed. “It’s a failure of humanity to have created these amazing materials which have improved our lives in many ways, but at the same time to be so shortsighted that we didn’t think about what to do with the waste,” McNeil said in a press release.
Susanne Koch puts it more succinctly: “What’s the point if we save patients while killing the planet?”
The Friday Five: A surprising health benefit for people who have kids
In this week's Friday Five, your kids may be stressing you out, but research suggests they're actually protecting a key aspect of your health. Plus, a new device unlocks the heart's secrets, super-ager gene transplants and more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- Kids stressing you out? They could be protecting your health.
- A new device unlocks the heart's secrets
- Super-ager gene transplants
- Surgeons could 3D print your organs before operations
- A skull cap looks into the brain like an fMRI

