Polio to COVID-19: Why Has Vaccine Confidence Eroded Over the Last 70 Years?

On left, people excitedly line up for Salk's polio vaccine in 1957; on right, Joe Biden gets one of the COVID vaccines on December 21, 2020.
On the morning of April 12, 1955, newsrooms across the United States inked headlines onto newsprint: the Salk Polio vaccine was "safe, effective, and potent." This was long-awaited news. Americans had limped through decades of fear, unaware of what caused polio or how to cure it, faced with the disease's terrifying, visible power to paralyze and kill, particularly children.
The announcement of the polio vaccine was celebrated with noisy jubilation: church bells rang, factory whistles sounded, people wept in the streets. Within weeks, mass inoculation began as the nation put its faith in a vaccine that would end polio.
Today, most of us are blissfully ignorant of child polio deaths, making it easier to believe that we have not personally benefited from the development of vaccines. According to Dr. Steven Pinker, cognitive psychologist and author of the bestselling book Enlightenment Now, we've become blasé to the gifts of science. "The default expectation is not that disease is part of life and science is a godsend, but that health is the default, and any disease is some outrage," he says.
We're now in the early stages of another vaccine rollout, one we hope will end the ravages of the COVID-19 pandemic. And yet, the Pfizer, Moderna, and AstraZeneca vaccines are met with far greater hesitancy and skepticism than the polio vaccine was in the 50s.
In 2021, concerns over the speed and safety of vaccine development and technology plague this heroic global effort, but the roots of vaccine hesitancy run far deeper. Vaccine hesitancy has always existed in the U.S., even in the polio era, motivated in part by fears around "living virus" in a bad batch of vaccines produced by Cutter Laboratories in 1955. But in the last half century, we've witnessed seismic cultural shifts—loss of public trust, a rise in misinformation, heightened racial and socioeconomic inequality, and political polarization have all intensified vaccine-related fears and resistance. Making sense of how we got here may help us understand how to move forward.
The Rise and Fall of Public Trust
When the polio vaccine was released in 1955, "we were nearing an all-time high point in public trust," says Matt Baum, Harvard Kennedy School professor and lead author of several reports measuring public trust and vaccine confidence. Baum explains that the U.S. was experiencing a post-war boom following the Allied triumph in WWII, a popular Roosevelt presidency, and the rapid innovation that elevated the country to an international superpower.
The 1950s witnessed the emergence of nuclear technology, a space program, and unprecedented medical breakthroughs, adds Emily Brunson, Texas State University anthropologist and co-chair of the Working Group on Readying Populations for COVID-19 Vaccine. "Antibiotics were a game changer," she states. While before, people got sick with pneumonia for a month, suddenly they had access to pills that accelerated recovery.
During this period, science seemed to hold all the answers; people embraced the idea that we could "come to know the world with an absolute truth," Brunson explains. Doctors were portrayed as unquestioned gods, so Americans were primed to trust experts who told them the polio vaccine was safe.
"The emotional tone of the news has gone downward since the 1940s, and journalists consider it a professional responsibility to cover the negative."
That blind acceptance eroded in the 1960s and 70s as people came to understand that science can be inherently political. "Getting to an absolute truth works out great for white men, but these things affect people socially in radically different ways," Brunson says. As the culture began questioning the white, patriarchal biases of science, doctors lost their god-like status and experts were pushed off their pedestals. This trend continues with greater intensity today, as President Trump has led a campaign against experts and waged a war on science that began long before the pandemic.
The Shift in How We Consume Information
In the 1950s, the media created an informational consensus. The fundamental ideas the public consumed about the state of the world were unified. "People argued about the best solutions, but didn't fundamentally disagree on the factual baseline," says Baum. Indeed, the messaging around the polio vaccine was centralized and consistent, led by President Roosevelt's successful March of Dimes crusade. People of lower socioeconomic status with limited access to this information were less likely to have confidence in the vaccine, but most people consumed media that assured them of the vaccine's safety and mobilized them to receive it.
Today, the information we consume is no longer centralized—in fact, just the opposite. "When you take that away, it's hard for people to know what to trust and what not to trust," Baum explains. We've witnessed an increase in polarization and the technology that makes it easier to give people what they want to hear, reinforcing the human tendencies to vilify the other side and reinforce our preexisting ideas. When information is engineered to further an agenda, each choice and risk calculation made while navigating the COVID-19 pandemic is deeply politicized.
This polarization maps onto a rise in socioeconomic inequality and economic uncertainty. These factors, associated with a sense of lost control, prime people to embrace misinformation, explains Baum, especially when the situation is difficult to comprehend. "The beauty of conspiratorial thinking is that it provides answers to all these questions," he says. Today's insidious fragmentation of news media accelerates the circulation of mis- and disinformation, reaching more people faster, regardless of veracity or motivation. In the case of vaccines, skepticism around their origin, safety, and motivation is intensified.
Alongside the rise in polarization, Pinker says "the emotional tone of the news has gone downward since the 1940s, and journalists consider it a professional responsibility to cover the negative." Relentless focus on everything that goes wrong further erodes public trust and paints a picture of the world getting worse. "Life saved is not a news story," says Pinker, but perhaps it should be, he continues. "If people were more aware of how much better life was generally, they might be more receptive to improvements that will continue to make life better. These improvements don't happen by themselves."
The Future Depends on Vaccine Confidence
So far, the U.S. has been unable to mitigate the catastrophic effects of the pandemic through social distancing, testing, and contact tracing. President Trump has downplayed the effects and threat of the virus, censored experts and scientists, given up on containing the spread, and mobilized his base to protest masks. The Trump Administration failed to devise a national plan, so our national plan has defaulted to hoping for the "miracle" of a vaccine. And they are "something of a miracle," Pinker says, describing vaccines as "the most benevolent invention in the history of our species." In record-breaking time, three vaccines have arrived. But their impact will be weakened unless we achieve mass vaccination. As Brunson notes, "The technology isn't the fix; it's people taking the technology."
Significant challenges remain, including facilitating widespread access and supporting on-the-ground efforts to allay concerns and build trust with specific populations with historic reasons for distrust, says Brunson. Baum predicts continuing delays as well as deaths from other causes that will be linked to the vaccine.
Still, there's every reason for hope. The new administration "has its eyes wide open to these challenges. These are the kind of problems that are amenable to policy solutions if we have the will," Baum says. He forecasts widespread vaccination by late summer and a bounce back from the economic damage, a "Good News Story" that will bolster vaccine acceptance in the future. And Pinker reminds us that science, medicine, and public health have greatly extended our lives in the last few decades, a trend that can only continue if we're willing to roll up our sleeves.
A movie still from the 1966 film "Fantastic Voyage"
In the 1966 movie "Fantastic Voyage," actress Raquel Welch and her submarine were shrunk to the size of a cell in order to eliminate a blood clot in a scientist's brain. Now, 55 years later, the scenario is becoming closer to reality.
California-based startup Bionaut Labs has developed a nanobot about the size of a grain of rice that's designed to transport medication to the exact location in the body where it's needed. If you think about it, the conventional way to deliver medicine makes little sense: A painkiller affects the entire body instead of just the arm that's hurting, and chemotherapy is flushed through all the veins instead of precisely targeting the tumor.
"Chemotherapy is delivered systemically," Bionaut-founder and CEO Michael Shpigelmacher says. "Often only a small percentage arrives at the location where it is actually needed."
But what if it was possible to send a tiny robot through the body to attack a tumor or deliver a drug at exactly the right location?
Several startups and academic institutes worldwide are working to develop such a solution but Bionaut Labs seems the furthest along in advancing its invention. "You can think of the Bionaut as a tiny screw that moves through the veins as if steered by an invisible screwdriver until it arrives at the tumor," Shpigelmacher explains. Via Zoom, he shares the screen of an X-ray machine in his Culver City lab to demonstrate how the half-transparent, yellowish device winds its way along the spine in the body. The nanobot contains a tiny but powerful magnet. The "invisible screwdriver" is an external magnetic field that rotates that magnet inside the device and gets it to move and change directions.
The current model has a diameter of less than a millimeter. Shpigelmacher's engineers could build the miniature vehicle even smaller but the current size has the advantage of being big enough to see with bare eyes. It can also deliver more medicine than a tinier version. In the Zoom demonstration, the micorobot is injected into the spine, not unlike an epidural, and pulled along the spine through an outside magnet until the Bionaut reaches the brainstem. Depending which organ it needs to reach, it could be inserted elsewhere, for instance through a catheter.
"The hope is that we can develop a vehicle to transport medication deep into the body," says Max Planck scientist Tian Qiu.
Imagine moving a screw through a steak with a magnet — that's essentially how the device works. But of course, the Bionaut is considerably different from an ordinary screw: "At the right location, we give a magnetic signal, and it unloads its medicine package," Shpigelmacher says.
To start, Bionaut Labs wants to use its device to treat Parkinson's disease and brain stem gliomas, a type of cancer that largely affects children and teenagers. About 300 to 400 young people a year are diagnosed with this type of tumor. Radiation and brain surgery risk damaging sensitive brain tissue, and chemotherapy often doesn't work. Most children with these tumors live less than 18 months. A nanobot delivering targeted chemotherapy could be a gamechanger. "These patients really don't have any other hope," Shpigelmacher says.
Of course, the main challenge of the developing such a device is guaranteeing that it's safe. Because tissue is so sensitive, any mistake could risk disastrous results. In recent years, Bionaut has tested its technology in dozens of healthy sheep and pigs with no major adverse effects. Sheep make a good stand-in for humans because their brains and spines are similar to ours.

The Bionaut device is about the size of a grain of rice.
Bionaut Labs
"As the Bionaut moves through brain tissue, it creates a transient track that heals within a few weeks," Shpigelmacher says. The company is hoping to be the first to test a nanobot in humans. In December 2022, it announced that a recent round of funding drew $43.2 million, for a total of 63.2 million, enabling more research and, if all goes smoothly, human clinical trials by early next year.
Once the technique has been perfected, further applications could include addressing other kinds of brain disorders that are considered incurable now, such as Alzheimer's or Huntington's disease. "Microrobots could serve as a bridgehead, opening the gateway to the brain and facilitating precise access of deep brain structure – either to deliver medication, take cell samples or stimulate specific brain regions," Shpigelmacher says.
Robot-assisted hybrid surgery with artificial intelligence is already used in state-of-the-art surgery centers, and many medical experts believe that nanorobotics will be the instrument of the future. In 2016, three scientists were awarded the Nobel Prize in Chemistry for their development of "the world's smallest machines," nano "elevators" and minuscule motors. Since then, the scientific experiments have progressed to the point where applicable devices are moving closer to actually being implemented.
Bionaut's technology was initially developed by a research team lead by Peer Fischer, head of the independent Micro Nano and Molecular Systems Lab at the Max Planck Institute for Intelligent Systems in Stuttgart, Germany. Fischer is considered a pioneer in the research of nano systems, which he began at Harvard University more than a decade ago. He and his team are advising Bionaut Labs and have licensed their technology to the company.
"The hope is that we can develop a vehicle to transport medication deep into the body," says Max Planck scientist Tian Qiu, who leads the cooperation with Bionaut Labs. He agrees with Shpigelmacher that the Bionaut's size is perfect for transporting medication loads and is researching potential applications for even smaller nanorobots, especially in the eye, where the tissue is extremely sensitive. "Nanorobots can sneak through very fine tissue without causing damage."
In "Fantastic Voyage," Raquel Welch's adventures inside the body of a dissident scientist let her swim through his veins into his brain, but her shrunken miniature submarine is attacked by antibodies; she has to flee through the nerves into the scientist's eye where she escapes into freedom on a tear drop. In reality, the exit in the lab is much more mundane. The Bionaut simply leaves the body through the same port where it entered. But apart from the dramatization, the "Fantastic Voyage" was almost prophetic, or, as Shpigelmacher says, "Science fiction becomes science reality."
This article was first published by Leaps.org on April 12, 2021.
How the Human Brain Project Built a Mind of its Own
In 2013, the Human Brain Project set out to build a realistic computer model of the brain over ten years. Now, experts are reflecting on HBP's achievements with an eye toward the future.
In 2009, neuroscientist Henry Markram gave an ambitious TED talk. “Our mission is to build a detailed, realistic computer model of the human brain,” he said, naming three reasons for this unmatched feat of engineering. One was because understanding the human brain was essential to get along in society. Another was because experimenting on animal brains could only get scientists so far in understanding the human ones. Third, medicines for mental disorders weren’t good enough. “There are two billion people on the planet that are affected by mental disorders, and the drugs that are used today are largely empirical,” Markram said. “I think that we can come up with very concrete solutions on how to treat disorders.”
Markram's arguments were very persuasive. In 2013, the European Commission launched the Human Brain Project, or HBP, as part of its Future and Emerging Technologies program. Viewed as Europe’s chance to try to win the “brain race” between the U.S., China, Japan, and other countries, the project received about a billion euros in funding with the goal to simulate the entire human brain on a supercomputer, or in silico, by 2023.
Now, after 10 years of dedicated neuroscience research, the HBP is coming to an end. As its many critics warned, it did not manage to build an entire human brain in silico. Instead, it achieved a multifaceted array of different goals, some of them unexpected.
Scholars have found that the project did help advance neuroscience more than some detractors initially expected, specifically in the area of brain simulations and virtual models. Using an interdisciplinary approach of combining technology, such as AI and digital simulations, with neuroscience, the HBP worked to gain a deeper understanding of the human brain’s complicated structure and functions, which in some cases led to novel treatments for brain disorders. Lastly, through online platforms, the HBP spearheaded a previously unmatched level of global neuroscience collaborations.
Simulating a human brain stirs up controversy
Right from the start, the project was plagued with controversy and condemnation. One of its prominent critics was Yves Fregnac, a professor in cognitive science at the Polytechnic Institute of Paris and research director at the French National Centre for Scientific Research. Fregnac argued in numerous articles that the HBP was overfunded based on proposals with unrealistic goals. “This new way of over-selling scientific targets, deeply aligned with what modern society expects from mega-sciences in the broad sense (big investment, big return), has been observed on several occasions in different scientific sub-fields,” he wrote in one of his articles, “before invading the field of brain sciences and neuromarketing.”
"A human brain model can simulate an experiment a million times for many different conditions, but the actual human experiment can be performed only once or a few times," said Viktor Jirsa, a professor at Aix-Marseille University.
Responding to such critiques, the HBP worked to restructure the effort in its early days with new leadership, organization, and goals that were more flexible and attainable. “The HBP got a more versatile, pluralistic approach,” said Viktor Jirsa, a professor at Aix-Marseille University and one of the HBP lead scientists. He believes that these changes fixed at least some of HBP’s issues. “The project has been on a very productive and scientifically fruitful course since then.”
After restructuring, the HBP became a European hub on brain research, with hundreds of scientists joining its growing network. The HBP created projects focused on various brain topics, from consciousness to neurodegenerative diseases. HBP scientists worked on complex subjects, such as mapping out the brain, combining neuroscience and robotics, and experimenting with neuromorphic computing, a computational technique inspired by the human brain structure and function—to name just a few.
Simulations advance knowledge and treatment options
In 2013, it seemed that bringing neuroscience into a digital age would be farfetched, but research within the HBP has made this achievable. The virtual maps and simulations various HBP teams create through brain imaging data make it easier for neuroscientists to understand brain developments and functions. The teams publish these models on the HBP’s EBRAINS online platform—one of the first to offer access to such data to neuroscientists worldwide via an open-source online site. “This digital infrastructure is backed by high-performance computers, with large datasets and various computational tools,” said Lucy Xiaolu Wang, an assistant professor in the Resource Economics Department at the University of Massachusetts Amherst, who studies the economics of the HBP. That means it can be used in place of many different types of human experimentation.
Jirsa’s team is one of many within the project that works on virtual brain models and brain simulations. Compiling patient data, Jirsa and his team can create digital simulations of different brain activities—and repeat these experiments many times, which isn’t often possible in surgeries on real brains. “A human brain model can simulate an experiment a million times for many different conditions,” Jirsa explained, “but the actual human experiment can be performed only once or a few times.” Using simulations also saves scientists and doctors time and money when looking at ways to diagnose and treat patients with brain disorders.
Compiling patient data, scientists can create digital simulations of different brain activities—and repeat these experiments many times.
The Human Brain Project
Simulations can help scientists get a full picture that otherwise is unattainable. “Another benefit is data completion,” added Jirsa, “in which incomplete data can be complemented by the model. In clinical settings, we can often measure only certain brain areas, but when linked to the brain model, we can enlarge the range of accessible brain regions and make better diagnostic predictions.”
With time, Jirsa’s team was able to move into patient-specific simulations. “We advanced from generic brain models to the ability to use a specific patient’s brain data, from measurements like MRI and others, to create individualized predictive models and simulations,” Jirsa explained. He and his team are working on this personalization technique to treat patients with epilepsy. According to the World Health Organization, about 50 million people worldwide suffer from epilepsy, a disorder that causes recurring seizures. While some epilepsy causes are known others remain an enigma, and many are hard to treat. For some patients whose epilepsy doesn’t respond to medications, removing part of the brain where seizures occur may be the only option. Understanding where in the patients’ brains seizures arise can give scientists a better idea of how to treat them and whether to use surgery versus medications.
“We apply such personalized models…to precisely identify where in a patient’s brain seizures emerge,” Jirsa explained. “This guides individual surgery decisions for patients for which surgery is the only treatment option.” He credits the HBP for the opportunity to develop this novel approach. “The personalization of our epilepsy models was only made possible by the Human Brain Project, in which all the necessary tools have been developed. Without the HBP, the technology would not be in clinical trials today.”
Personalized simulations can significantly advance treatments, predict the outcome of specific medical procedures and optimize them before actually treating patients. Jirsa is watching this happen firsthand in his ongoing research. “Our technology for creating personalized brain models is now used in a large clinical trial for epilepsy, funded by the French state, where we collaborate with clinicians in hospitals,” he explained. “We have also founded a spinoff company called VB Tech (Virtual Brain Technologies) to commercialize our personalized brain model technology and make it available to all patients.”
The Human Brain Project created a level of interconnectedness within the neuroscience research community that never existed before—a network not unlike the brain’s own.
Other experts believe it’s too soon to tell whether brain simulations could change epilepsy treatments. “The life cycle of developing treatments applicable to patients often runs over a decade,” Wang stated. “It is still too early to draw a clear link between HBP’s various project areas with patient care.” However, she admits that some studies built on the HBP-collected knowledge are already showing promise. “Researchers have used neuroscientific atlases and computational tools to develop activity-specific stimulation programs that enabled paraplegic patients to move again in a small-size clinical trial,” Wang said. Another intriguing study looked at simulations of Alzheimer’s in the brain to understand how it evolves over time.
Some challenges remain hard to overcome even with computer simulations. “The major challenge has always been the parameter explosion, which means that many different model parameters can lead to the same result,” Jirsa explained. An example of this parameter explosion could be two different types of neurodegenerative conditions, such as Parkinson’s and Huntington’s diseases. Both afflict the same area of the brain, the basal ganglia, which can affect movement, but are caused by two different underlying mechanisms. “We face the same situation in the living brain, in which a large range of diverse mechanisms can produce the same behavior,” Jirsa said. The simulations still have to overcome the same challenge.
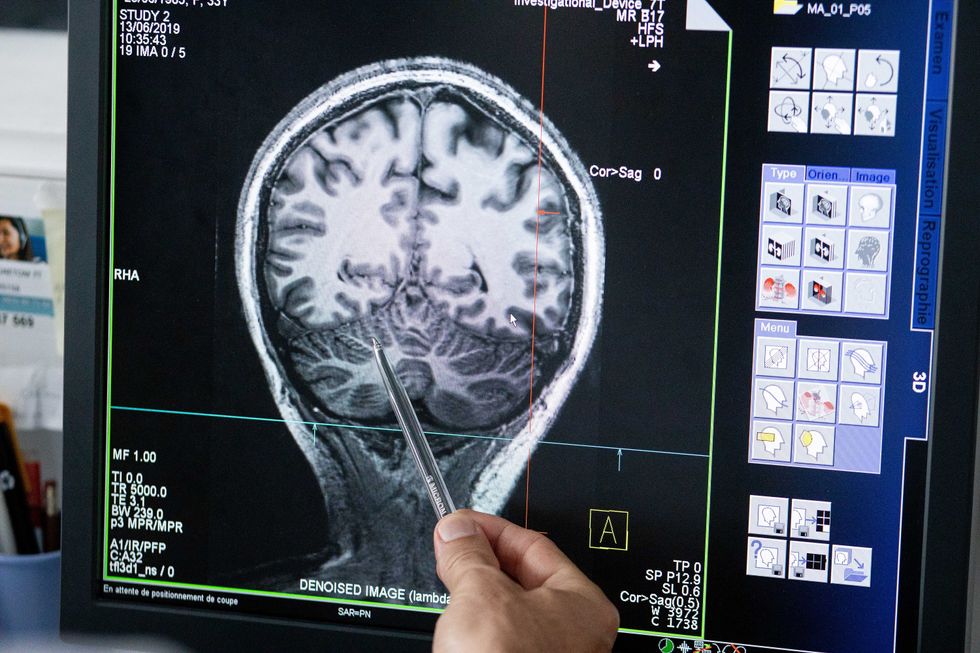
Understanding where in the patients’ brains seizures arise can give scientists a better idea of how to treat them and whether to use surgery versus medications.
The Human Brain Project
A network not unlike the brain’s own
Though the HBP will be closing this year, its legacy continues in various studies, spin-off companies, and its online platform, EBRAINS. “The HBP is one of the earliest brain initiatives in the world, and the 10-year long-term goal has united many researchers to collaborate on brain sciences with advanced computational tools,” Wang said. “Beyond the many research articles and projects collaborated on during the HBP, the online neuroscience research infrastructure EBRAINS will be left as a legacy even after the project ends.”
Those who worked within the HBP see the end of this project as the next step in neuroscience research. “Neuroscience has come closer to very meaningful applications through the systematic link with new digital technologies and collaborative work,” Jirsa stated. “In that way, the project really had a pioneering role.” It also created a level of interconnectedness within the neuroscience research community that never existed before—a network not unlike the brain’s own. “Interconnectedness is an important advance and prerequisite for progress,” Jirsa said. “The neuroscience community has in the past been rather fragmented and this has dramatically changed in recent years thanks to the Human Brain Project.”
According to its website, by 2023 HBP’s network counted over 500 scientists from over 123 institutions and 16 different countries, creating one of the largest multi-national research groups in the world. Even though the project hasn’t produced the in-silico brain as Markram envisioned it, the HBP created a communal mind with immense potential. “It has challenged us to think beyond the boundaries of our own laboratories,” Jirsa said, “and enabled us to go much further together than we could have ever conceived going by ourselves.”