The First Cloned Monkeys Provoked More Shrugs Than Shocks

Zhong Zhong and Hua Hua, the two cloned macaques.
A few months ago, it was announced that not one, but two healthy long-tailed macaque monkeys were cloned—a first for primates of any kind. The cells were sourced from aborted monkey fetuses and the DNA transferred into eggs whose nuclei had been removed, the same method that was used in 1996 to clone "Dolly the Sheep." Two live births, females named Zhong Zhong and Hua Hua, resulted from 60 surrogate mothers. Inefficient, it's true. But over time, the methods are likely to be improved.
The scientist who supervised the project predicts that cloning, along with gene editing, will result in "ideal primate models" for studying disease mechanisms and drug screening.
Dr. Gerald Schatten, a famous would-be monkey cloner, authored a controversial paper in 2003 describing the formidable challenges to cloning monkeys and humans, speculating that the feat might never be accomplished. Now, some 15 years later, that prediction, insofar as it relates to monkeys, has blown away.
Zhong Zhong and Hua Hua were created at the Chinese Academy of Science's Institute of Neuroscience in Shanghai. The Institute founded in 1999 boasts 32 laboratories, expanding to 50 labs in 2020. It maintains two non-human primate research facilities.
The founder and director, Dr. Mu-ming Poo, supervised the project. Poo is an extremely accomplished senior researcher at the pinnacle of his field, a distinguished professor emeritus in Biology at UC Berkeley. In 2016, he was awarded the prestigious $500,000 Gruber Neuroscience Prize. At that time, Poo's experiments were described by a colleague as being "innovative and very often ingenious."
Poo maintains the reputation of studying some of the most important questions in cellular neuroscience.
But is society ready to accept cloned primates for medical research without the attendant hysteria about fears of cloned humans?
By Western standards, use of non-human primates in research focuses on the welfare of the animal subjects. As PETA reminds us, there is a dreadful and sad history of mistreatment. Dr. Poo assures us that his cloned monkeys are treated ethically and that the Institute is compliant with the highest regulatory standards, as promulgated by the U.S. National Institutes of Health.
He presents the noblest justifications for the research. He predicts that cloning, along with gene editing, will result in "ideal primate models" for studying disease mechanisms and drug screening. He declares that this will eventually help to solve Parkinson's, Huntington's and Alzheimer's disease.
But is society ready to accept cloned primates for medical research without the attendant hysteria about fears of cloned humans? It appears so.
While much of the news coverage expressed this predictable worry, my overall impression is that the societal response was muted. Where was the expected outrage? Then again, we've come a long way since Dolly the Sheep in terms of both the science and the cultural acceptance of cloning. Perhaps my unique vantage point can provide perspective on how much attitudes have evolved.
Perhaps my unique vantage point can provide perspective on how much attitudes have evolved.
I sometimes joke that I am the world's only human cloning lawyer—a great gig but there are still no clients.
I first crashed into the cloning scene in 2002 when I sued the so-called human cloning company "Clonaid" and asked in court to have a temporary guardian appointed for the alleged first human clone "Baby Eve." The claim needed to be tested, and mine was the first case ever aiming to protect the rights of a human clone. My legal basis was child welfare law, protecting minors from abuse, negligence, and exploitation.
The case had me on back-to-back global television broadcasts around the world; there was live news and "breathless" coverage at the courthouse emblazoned in headlines in every language on the planet. Cloning was, after all, perceived as a species-altering event: asexual reproduction. The controversy dominated world headlines for month until Clonaid's claim was busted as the "fakest" of fake news.
Fresh off the cloning case, the scientific community reached out to me, seeing me as the defender of legitimate science, an opponent of cloning human babies but a proponent of using cloning techniques to accelerate ethical regenerative medicine and embryonic stem cell research in general.
The years 2003 to 2006 were the era of the "stem cell wars" and a dominant issue was human cloning. Social conservative lawmakers around the world were seeking bans or criminalization not only of cloning babies but also the cloning of cells to match the donor's genetics. Scientists were being threatened with fines and imprisonment. Human cloning was being challenged in the United Nations with the United States backing a global treaty to ban and morally condemn all cloning -- including the technique that was crucial for research.
Scientists and patients were touting the cloning technique as a major biomedical breakthrough because cells could be created as direct genetic matches from a specific donor.
At the same time, scientists and patients were touting the cloning technique as a major biomedical breakthrough because cells could be created as direct genetic matches from a specific donor.
So my organization organized a conference at UN headquarters to defend research cloning and all the big names in stem cell research were there. We organized petitions to the UN and faxed 35,000 signatures to the country mission. These ongoing public policy battles were exacerbated in part because of the growing fear that cloning babies was just around the corner.
Then in 2005, the first cloned dog stunned the world, an Afghan hound named Snuppy. I met him when I visited the laboratories of Professor Woo Suk Hwang in Korea. His minders let me hold his leash -- TIME magazine's scientific breakthrough of the year. He didn't lick me or even wag his tail; I figured he must not like lawyers.
Tragically, soon thereafter, I witnessed firsthand Dr. Hwang's fall from grace when his human stem cell cloning breakthroughs proved false. The massive scientific misconduct rocked the nation of Korea, stem cell science in general, and provoked terrible news coverage.
Nevertheless, by 2007, the proposed bans lost steam, overridden by the advent of a Japanese researcher's Nobel Prize winning formula for reprogramming human cells to create genetically matched cell lines, not requiring the destruction of human embryos.
After years of panic, none of the recent cloning headlines has caused much of a stir.
Five years later, when two American scientists accomplished therapeutic human cloned stem cell lines, their news was accepted without hysteria. Perhaps enough time had passed since Hwang and the drama was drained.
In the just past 30 days we have seen more cloning headlines. Another cultural icon, Barbara Streisand, revealed she owns two cloned Coton de Tulear puppies. The other weekend, the television news show "60 Minutes" devoted close to an hour on the cloned ponies used at the top level of professional polo. And in India, scientists just cloned the first Assamese buffalo.
And you know what? After years of panic, none of this has caused much of a stir. It's as if the future described by Alvin Toffler in "Future Shock" has arrived and we are just living with it. A couple of cloned monkeys barely move the needle.
Perhaps it is the advent of the Internet and the overall dilution of wonder and outrage. Or maybe the muted response is rooted in popular culture. From Orphan Black to the plotlines of dozens of shows and books, cloning is just old news. The hand-wringing discussions about "human dignity" and "slippery slopes" have taken a backseat to the AI apocalypse and Martian missions.
We humans are enduring plagues of dementia and Alzheimer's, and we will need more monkeys. I will take mine cloned, if it will speed progress.
Personally, I still believe that cloned children should not be an option. Child welfare laws might be the best deterrent.
The same does not hold for cloning monkey research subjects. Squeamishness aside, I think Zhong Zhong and Hua Hua will soon be joined by a legion of cloned macaques and probably marmosets.
We humans are enduring plagues of dementia and Alzheimer's, and we will need more monkeys. I will take mine cloned, if it will speed the mending of these consciousness-destroying afflictions.
Scientific revolutions once took centuries, then decades, and now seem to bombard us daily. The convergence of technologies has accelerated the future. To Zhong Zhong and Hua Hua, my best wishes with the hope that their sacrifices will contribute to the health of all primates -- not just humans.
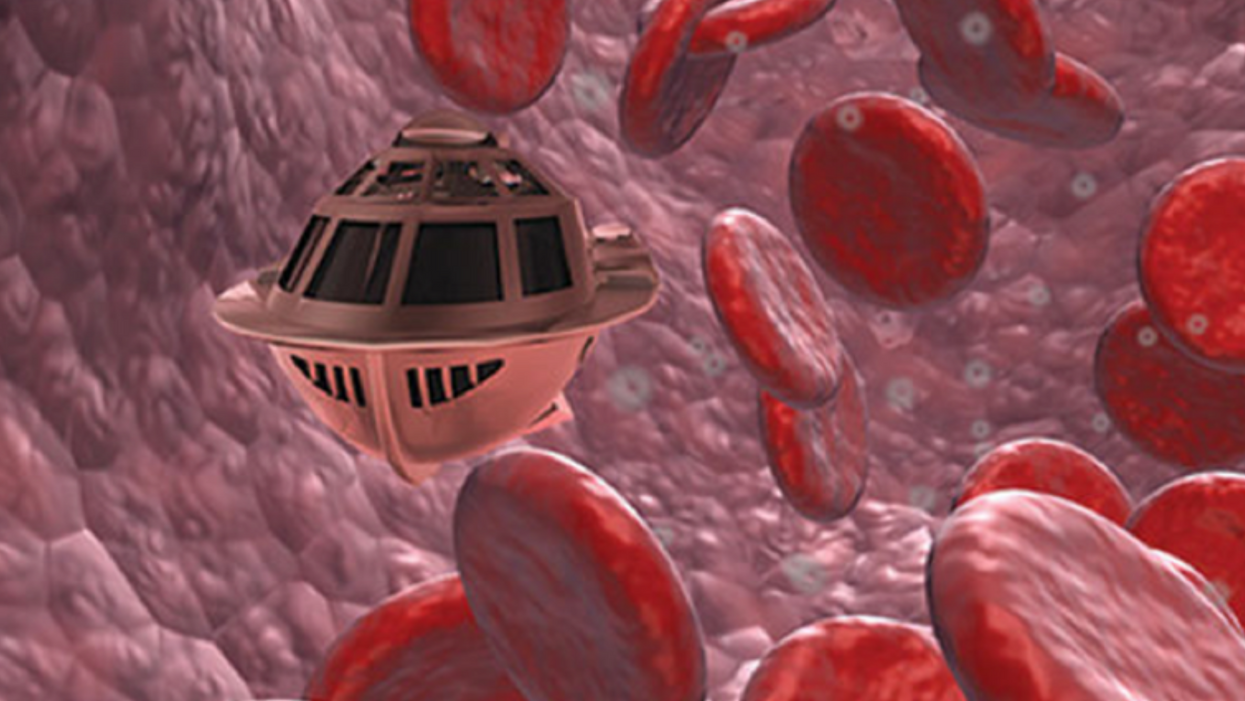
Tiny, Injectable Robots Could Be the Future of Brain Treatments
A movie still from the 1966 film "Fantastic Voyage"
In the 1966 movie "Fantastic Voyage," actress Raquel Welch and her submarine were shrunk to the size of a cell in order to eliminate a blood clot in a scientist's brain. Now, 55 years later, the scenario is becoming closer to reality.
California-based startup Bionaut Labs has developed a nanobot about the size of a grain of rice that's designed to transport medication to the exact location in the body where it's needed. If you think about it, the conventional way to deliver medicine makes little sense: A painkiller affects the entire body instead of just the arm that's hurting, and chemotherapy is flushed through all the veins instead of precisely targeting the tumor.
"Chemotherapy is delivered systemically," Bionaut-founder and CEO Michael Shpigelmacher says. "Often only a small percentage arrives at the location where it is actually needed."
But what if it was possible to send a tiny robot through the body to attack a tumor or deliver a drug at exactly the right location?
Several startups and academic institutes worldwide are working to develop such a solution but Bionaut Labs seems the furthest along in advancing its invention. "You can think of the Bionaut as a tiny screw that moves through the veins as if steered by an invisible screwdriver until it arrives at the tumor," Shpigelmacher explains. Via Zoom, he shares the screen of an X-ray machine in his Culver City lab to demonstrate how the half-transparent, yellowish device winds its way along the spine in the body. The nanobot contains a tiny but powerful magnet. The "invisible screwdriver" is an external magnetic field that rotates that magnet inside the device and gets it to move and change directions.
The current model has a diameter of less than a millimeter. Shpigelmacher's engineers could build the miniature vehicle even smaller but the current size has the advantage of being big enough to see with bare eyes. It can also deliver more medicine than a tinier version. In the Zoom demonstration, the micorobot is injected into the spine, not unlike an epidural, and pulled along the spine through an outside magnet until the Bionaut reaches the brainstem. Depending which organ it needs to reach, it could be inserted elsewhere, for instance through a catheter.
"The hope is that we can develop a vehicle to transport medication deep into the body."
Imagine moving a screw through a steak with a magnet — that's essentially how the device works. But of course, the Bionaut is considerably different from an ordinary screw: "At the right location, we give a magnetic signal, and it unloads its medicine package," Shpigelmacher says.
To start, Bionaut Labs wants to use its device to treat Parkinson's disease and brain stem gliomas, a type of cancer that largely affects children and teenagers. About 300 to 400 young people a year are diagnosed with this type of tumor. Radiation and brain surgery risk damaging sensitive brain tissue, and chemotherapy often doesn't work. Most children with these tumors live less than 18 months. A nanobot delivering targeted chemotherapy could be a gamechanger. "These patients really don't have any other hope," Shpigelmacher says.
Of course, the main challenge of the developing such a device is guaranteeing that it's safe. Because tissue is so sensitive, any mistake could risk disastrous results. Over the past four years, Bionaut has tested its technology in dozens of healthy sheep and pigs with no major adverse effects. Sheep make a good stand-in for humans because their brains and spines are similar to ours.

The Bionaut device is about the size of a grain of rice.
Bionaut Labs
"As the Bionaut moves through brain tissue, it creates a transient track that heals within a few weeks," Shpigelmacher says. The company is hoping to be the first to test a nanobot in humans. That could happen as early as 2023, Shpigelmacher says.
Once the technique has been perfected, further applications could include addressing other kinds of brain disorders that are considered incurable now, such as Alzheimer's or Huntington's disease. "Microrobots could serve as a bridgehead, opening the gateway to the brain and facilitating precise access of deep brain structure – either to deliver medication, take cell samples or stimulate specific brain regions," Shpigelmacher says.
Robot-assisted hybrid surgery with artificial intelligence is already used in state-of-the-art surgery centers, and many medical experts believe that nanorobotics will be the instrument of the future. In 2016, three scientists were awarded the Nobel Prize in Chemistry for their development of "the world's smallest machines," nano "elevators" and minuscule motors. Since then, the scientific experiments have progressed to the point where applicable devices are moving closer to actually being implemented.
Bionaut's technology was initially developed by a research team lead by Peer Fischer, head of the independent Micro Nano and Molecular Systems Lab at the Max Planck Institute for Intelligent Systems in Stuttgart, Germany. Fischer is considered a pioneer in the research of nano systems, which he began at Harvard University more than a decade ago. He and his team are advising Bionaut Labs and have licensed their technology to the company.
"The hope is that we can develop a vehicle to transport medication deep into the body," says Max Planck scientist Tian Qiu, who leads the cooperation with Bionaut Labs. He agrees with Shpigelmacher that the Bionaut's size is perfect for transporting medication loads and is researching potential applications for even smaller nanorobots, especially in the eye, where the tissue is extremely sensitive. "Nanorobots can sneak through very fine tissue without causing damage."
In "Fantastic Voyage," Raquel Welch's adventures inside the body of a dissident scientist let her swim through his veins into his brain, but her shrunken miniature submarine is attacked by antibodies; she has to flee through the nerves into the scientist's eye where she escapes into freedom on a tear drop. In reality, the exit in the lab is much more mundane. The Bionaut simply leaves the body through the same port where it entered. But apart from the dramatization, the "Fantastic Voyage" was almost prophetic, or, as Shpigelmacher says, "Science fiction becomes science reality."
Every weekend since January, pediatrician Cora Collette Breuner has volunteered to give the COVID-19 vaccine to individuals from age 12 to 96 in an underserved community in Washington state.
Even though the COVID-19 vaccines have been shown to be incredibly safe and effective, there's still quite a bit of hesitancy among parents to vaccinate their teenage children, says Breuner, an adolescent medicine specialist at Seattle Children's Hospital and a past chair of the American Academy of Pediatrics' Committee on Adolescence. "They have questions and they have questions," she says.
Breuner patiently answers them all. Even then, parents—who have the final say in whether their child gets the vaccine—may be reluctant to sign off on it.
In 41 states, parents must consent for minors under age 18 to receive a COVID-19 vaccine. One state—Nebraska—requires parental consent for individuals under age 19, according to the Kaiser Family Foundation. Healthcare workers can't legally give teens COVID-19 vaccines otherwise. In a May report, the nonprofit healthcare organization highlights that from a legal perspective, "the landscape may be shifting slightly as more jurisdictions seek to encourage vaccination of young people."
Meanwhile, as the Delta variant creates a new surge in cases, some ethicists and pediatricians argue that state laws should be amended or loosened to allow minors to consent to COVID-19 vaccination on their own, without the need for parental permission.
"COVID-19 has killed millions of people around the world and disrupted the global economy," says pediatrician John Lantos. "It's a global catastrophe that requires special rules."
There are compelling arguments in favor of letting minors consent on their own, says Robyn Shapiro, a health care lawyer and a bioethicist in the Milwaukee area. "By that, I mean they're either old enough or they're evaluated in such a way that they have sufficient understanding of what they're agreeing to."
Shapiro and other ethicists argue that teens are perfectly capable of giving "informed consent"—a key principle in ethics that means fully understanding the benefits and risks of a medical intervention. To give informed consent, a person must be able to process that information in line with their own values. Only then can they make an autonomous choice and sign a consent form, Shapiro says.
Most states already have laws permitting minors to consent to testing and treatments related to sexually transmitted diseases, birth control, behavioral health, and substance abuse. It wouldn't be that much of a stretch to add COVID-19 vaccination to the list, Shapiro says. New Jersey and New York have introduced bills to let teens as young as 14 to consent to getting the COVID-19 vaccine and Minnesota has proposed a bill to allow children as young as 12 to give consent.
With any medical test or intervention, doctors often wrestle with how to best involve teens in conversations about their own health care, says John Lantos, a pediatrician and director of the Bioethics Center at Children's Mercy Kansas City.
"Most bioethicists would say that [teens] should be included to the degree that they have decision-making capacity," he says. "In most cases, that means including them in discussions with their parents in trying to achieve consensus about what the best choice may be."
COVID-19 vaccination also presents a unique circumstance, Lantos notes. It raises the question: Should teens have greater decisional authority because it's a public health emergency? In his opinion, the answer is yes. "COVID-19 has killed millions of people around the world and disrupted the global economy," says pediatrician Lantos. "It's a global catastrophe that requires special rules."
In North Carolina, state legislators are moving to do the opposite. State law currently allows those under 18 to make vaccination decisions on their own, but on Aug. 5, North Carolina's General Assembly approved a Republican-sponsored bill requiring parental consent for 12- to 17-year-olds to get a COVID-19 vaccine.
Kyle Brothers, a pediatrician in Louisville, Kentucky, says it's "ethically justifiable" for states to permit adolescents, especially those on the verge of adulthood, to consent to COVID-19 vaccination and other straightforward medical care.
In many cases, 16- and 17-year-old adolescents are capable of making well-informed decisions, says Brothers, a member of the American Academy of Pediatrics' Section on Bioethics. "The problem is, the law tends not to have that level of nuance," he adds. "We know in the real world that maturing and developing the ability to make decisions is a continuous process, but the law sets a bright line at age 18."
Lacking parental consent, some defiant teens are researching avenues to get vaccinated without their mom's or dad's knowledge. They may have turned to VaxTeen.org, a site operated by a Los Angeles teenager that provides information on consent laws by state.
If parents are wavering on the decision to give consent, Breuner recommends that they speak with a trusted healthcare provider about their specific concerns. These kinds of dialogues often can clarify lingering worries and may help drive up consent rates for teen vaccination.
Vaccine-hesitant parents should hear out their teens who wish to be vaccinated. Teenagers have their own opinions and belief systems, and parents should respect their child's choice to be vaccinated if they wish, considering the minimal risk of harm and the significant benefit to society as a whole.
George J. Annas, professor and director at the Center for Health Law, Ethics & Human Rights at Boston University, says parents have a legal obligation to provide their children with necessary medical treatment, or they could be found guilty of child neglect. The circumstances vary, but in the face of unrelenting COVID-19, he says parents have an ethical duty to consent to teens' vaccination because "the disease is rampant and children are dying."