Who Qualifies as an “Expert” And How Can We Decide Who Is Trustworthy?

Discerning a real expert from a charlatan is crucial during the COVID-19 pandemic and beyond.
This article is part of the magazine, "The Future of Science In America: The Election Issue," co-published by LeapsMag, the Aspen Institute Science & Society Program, and GOOD.
Expertise is a slippery concept. Who has it, who claims it, and who attributes or yields it to whom is a culturally specific, sociological process. During the COVID-19 pandemic, we have witnessed a remarkable emergence of legitimate and not-so-legitimate scientists publicly claiming or being attributed to have academic expertise in precisely my field: infectious disease epidemiology. From any vantage point, it is clear that charlatans abound out there, garnering TV coverage and hundreds of thousands of Twitter followers based on loud opinions despite flimsy credentials. What is more interesting as an insider is the gradient of expertise beyond these obvious fakers.
A person's expertise is not a fixed attribute; it is a hierarchical trait defined relative to others. Despite my protestations, I am the go-to expert on every aspect of the pandemic to my family. To a reporter, I might do my best to answer a question about the immune response to SARS-CoV-2, noting that I'm not an immunologist. Among other academic scientists, my expertise is more well-defined as a subfield of epidemiology, and within that as a particular area within infectious disease epidemiology. There's a fractal quality to it; as you zoom in on a particular subject, a differentiation of expertise emerges among scientists who, from farther out, appear to be interchangeable.
We all have our scientific domain and are less knowledgeable outside it, of course, and we are often asked to comment on a broad range of topics. But many scientists without a track record in the field have become favorites among university administrators, senior faculty in unrelated fields, policymakers, and science journalists, using institutional prestige or social connections to promote themselves. This phenomenon leads to a distorted representation of science—and of academic scientists—in the public realm.
Trustworthy experts will direct you to others in their field who know more about particular topics, and will tend to be honest about what is and what isn't "in their lane."
Predictably, white male voices have been disproportionately amplified, and men are certainly over-represented in the category of those who use their connections to inappropriately claim expertise. Generally speaking, we are missing women, racial minorities, and global perspectives. This is not only important because it misrepresents who scientists are and reinforces outdated stereotypes that place white men in the Global North at the top of a credibility hierarchy. It also matters because it can promote bad science, and it passes over scientists who can lend nuance to the scientific discourse and give global perspectives on this quintessentially global crisis.
Also at work, in my opinion, are two biases within academia: the conflation of institutional prestige with individual expertise, and the bizarre hierarchy among scientists that attributes greater credibility to those in quantitative fields like physics. Regardless of mathematical expertise or institutional affiliation, lack of experience working with epidemiological data can lead to over-confidence in the deceptively simple mathematical models that we use to understand epidemics, as well as the inappropriate use of uncertain data to inform them. Prominent and vocal scientists from different quantitative fields have misapplied the methods of infectious disease epidemiology during the COVID-19 pandemic so far, creating enormous confusion among policymakers and the public. Early forecasts that predicted the epidemic would be over by now, for example, led to a sense that epidemiological models were all unreliable.
Meanwhile, legitimate scientific uncertainties and differences of opinion, as well as fundamentally different epidemic dynamics arising in diverse global contexts and in different demographic groups, appear in the press as an indistinguishable part of this general chaos. This leads many people to question whether the field has anything worthwhile to contribute, and muddies the facts about COVID-19 policies for reducing transmission that most experts agree on, like wearing masks and avoiding large indoor gatherings.
So how do we distinguish an expert from a charlatan? I believe a willingness to say "I don't know" and to openly describe uncertainties, nuances, and limitations of science are all good signs. Thoughtful engagement with questions and new ideas is also an indication of expertise, as opposed to arrogant bluster or a bullish insistence on a particular policy strategy regardless of context (which is almost always an attempt to hide a lack of depth of understanding). Trustworthy experts will direct you to others in their field who know more about particular topics, and will tend to be honest about what is and what isn't "in their lane." For example, some expertise is quite specific to a given subfield: epidemiologists who study non-infectious conditions or nutrition, for example, use different methods from those of infectious disease experts, because they generally don't need to account for the exponential growth that is inherent to a contagion process.
Academic scientists have a specific, technical contribution to make in containing the COVID-19 pandemic and in communicating research findings as they emerge. But the liminal space between scientists and the public is subject to the same undercurrents of sexism, racism, and opportunism that society and the academy have always suffered from. Although none of the proxies for expertise described above are fool-proof, they are at least indicative of integrity and humility—two traits the world is in dire need of at this moment in history.
[Editor's Note: To read other articles in this special magazine issue, visit the beautifully designed e-reader version.]
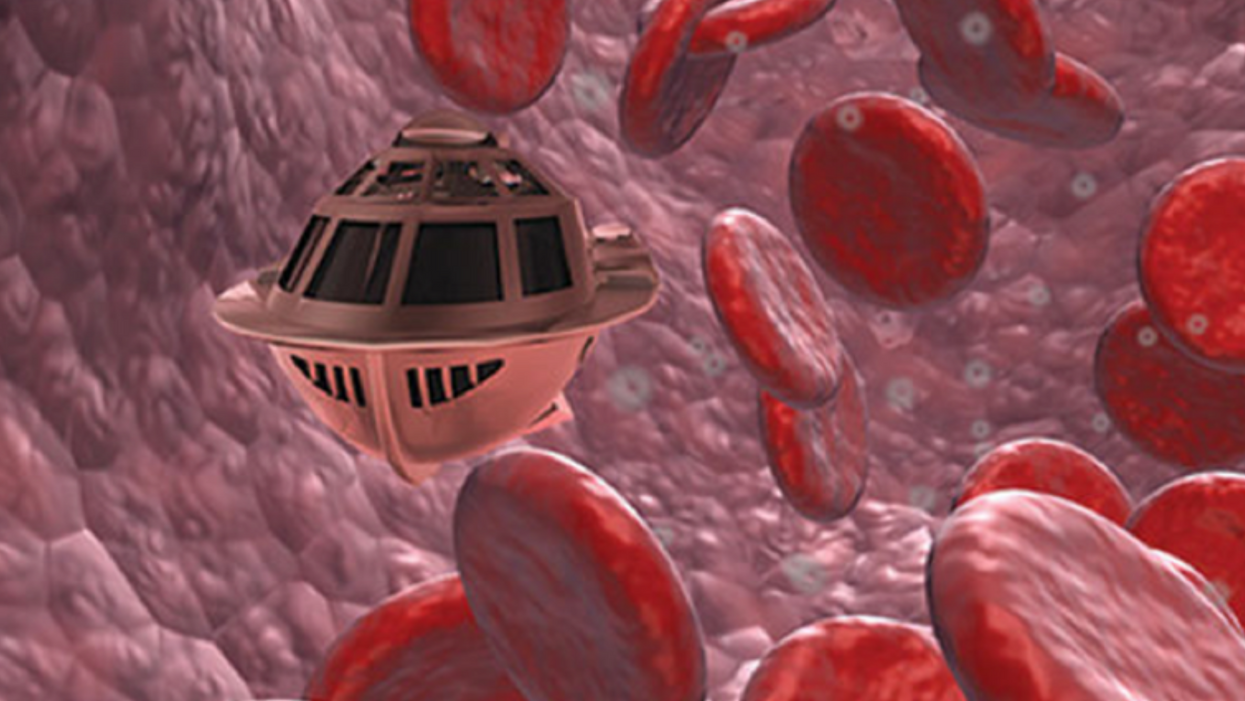
Tiny, Injectable Robots Could Be the Future of Brain Treatments
A movie still from the 1966 film "Fantastic Voyage"
In the 1966 movie "Fantastic Voyage," actress Raquel Welch and her submarine were shrunk to the size of a cell in order to eliminate a blood clot in a scientist's brain. Now, 55 years later, the scenario is becoming closer to reality.
California-based startup Bionaut Labs has developed a nanobot about the size of a grain of rice that's designed to transport medication to the exact location in the body where it's needed. If you think about it, the conventional way to deliver medicine makes little sense: A painkiller affects the entire body instead of just the arm that's hurting, and chemotherapy is flushed through all the veins instead of precisely targeting the tumor.
"Chemotherapy is delivered systemically," Bionaut-founder and CEO Michael Shpigelmacher says. "Often only a small percentage arrives at the location where it is actually needed."
But what if it was possible to send a tiny robot through the body to attack a tumor or deliver a drug at exactly the right location?
Several startups and academic institutes worldwide are working to develop such a solution but Bionaut Labs seems the furthest along in advancing its invention. "You can think of the Bionaut as a tiny screw that moves through the veins as if steered by an invisible screwdriver until it arrives at the tumor," Shpigelmacher explains. Via Zoom, he shares the screen of an X-ray machine in his Culver City lab to demonstrate how the half-transparent, yellowish device winds its way along the spine in the body. The nanobot contains a tiny but powerful magnet. The "invisible screwdriver" is an external magnetic field that rotates that magnet inside the device and gets it to move and change directions.
The current model has a diameter of less than a millimeter. Shpigelmacher's engineers could build the miniature vehicle even smaller but the current size has the advantage of being big enough to see with bare eyes. It can also deliver more medicine than a tinier version. In the Zoom demonstration, the micorobot is injected into the spine, not unlike an epidural, and pulled along the spine through an outside magnet until the Bionaut reaches the brainstem. Depending which organ it needs to reach, it could be inserted elsewhere, for instance through a catheter.
"The hope is that we can develop a vehicle to transport medication deep into the body."
Imagine moving a screw through a steak with a magnet — that's essentially how the device works. But of course, the Bionaut is considerably different from an ordinary screw: "At the right location, we give a magnetic signal, and it unloads its medicine package," Shpigelmacher says.
To start, Bionaut Labs wants to use its device to treat Parkinson's disease and brain stem gliomas, a type of cancer that largely affects children and teenagers. About 300 to 400 young people a year are diagnosed with this type of tumor. Radiation and brain surgery risk damaging sensitive brain tissue, and chemotherapy often doesn't work. Most children with these tumors live less than 18 months. A nanobot delivering targeted chemotherapy could be a gamechanger. "These patients really don't have any other hope," Shpigelmacher says.
Of course, the main challenge of the developing such a device is guaranteeing that it's safe. Because tissue is so sensitive, any mistake could risk disastrous results. Over the past four years, Bionaut has tested its technology in dozens of healthy sheep and pigs with no major adverse effects. Sheep make a good stand-in for humans because their brains and spines are similar to ours.

The Bionaut device is about the size of a grain of rice.
Bionaut Labs
"As the Bionaut moves through brain tissue, it creates a transient track that heals within a few weeks," Shpigelmacher says. The company is hoping to be the first to test a nanobot in humans. That could happen as early as 2023, Shpigelmacher says.
Once the technique has been perfected, further applications could include addressing other kinds of brain disorders that are considered incurable now, such as Alzheimer's or Huntington's disease. "Microrobots could serve as a bridgehead, opening the gateway to the brain and facilitating precise access of deep brain structure – either to deliver medication, take cell samples or stimulate specific brain regions," Shpigelmacher says.
Robot-assisted hybrid surgery with artificial intelligence is already used in state-of-the-art surgery centers, and many medical experts believe that nanorobotics will be the instrument of the future. In 2016, three scientists were awarded the Nobel Prize in Chemistry for their development of "the world's smallest machines," nano "elevators" and minuscule motors. Since then, the scientific experiments have progressed to the point where applicable devices are moving closer to actually being implemented.
Bionaut's technology was initially developed by a research team lead by Peer Fischer, head of the independent Micro Nano and Molecular Systems Lab at the Max Planck Institute for Intelligent Systems in Stuttgart, Germany. Fischer is considered a pioneer in the research of nano systems, which he began at Harvard University more than a decade ago. He and his team are advising Bionaut Labs and have licensed their technology to the company.
"The hope is that we can develop a vehicle to transport medication deep into the body," says Max Planck scientist Tian Qiu, who leads the cooperation with Bionaut Labs. He agrees with Shpigelmacher that the Bionaut's size is perfect for transporting medication loads and is researching potential applications for even smaller nanorobots, especially in the eye, where the tissue is extremely sensitive. "Nanorobots can sneak through very fine tissue without causing damage."
In "Fantastic Voyage," Raquel Welch's adventures inside the body of a dissident scientist let her swim through his veins into his brain, but her shrunken miniature submarine is attacked by antibodies; she has to flee through the nerves into the scientist's eye where she escapes into freedom on a tear drop. In reality, the exit in the lab is much more mundane. The Bionaut simply leaves the body through the same port where it entered. But apart from the dramatization, the "Fantastic Voyage" was almost prophetic, or, as Shpigelmacher says, "Science fiction becomes science reality."
Every weekend since January, pediatrician Cora Collette Breuner has volunteered to give the COVID-19 vaccine to individuals from age 12 to 96 in an underserved community in Washington state.
Even though the COVID-19 vaccines have been shown to be incredibly safe and effective, there's still quite a bit of hesitancy among parents to vaccinate their teenage children, says Breuner, an adolescent medicine specialist at Seattle Children's Hospital and a past chair of the American Academy of Pediatrics' Committee on Adolescence. "They have questions and they have questions," she says.
Breuner patiently answers them all. Even then, parents—who have the final say in whether their child gets the vaccine—may be reluctant to sign off on it.
In 41 states, parents must consent for minors under age 18 to receive a COVID-19 vaccine. One state—Nebraska—requires parental consent for individuals under age 19, according to the Kaiser Family Foundation. Healthcare workers can't legally give teens COVID-19 vaccines otherwise. In a May report, the nonprofit healthcare organization highlights that from a legal perspective, "the landscape may be shifting slightly as more jurisdictions seek to encourage vaccination of young people."
Meanwhile, as the Delta variant creates a new surge in cases, some ethicists and pediatricians argue that state laws should be amended or loosened to allow minors to consent to COVID-19 vaccination on their own, without the need for parental permission.
"COVID-19 has killed millions of people around the world and disrupted the global economy," says pediatrician John Lantos. "It's a global catastrophe that requires special rules."
There are compelling arguments in favor of letting minors consent on their own, says Robyn Shapiro, a health care lawyer and a bioethicist in the Milwaukee area. "By that, I mean they're either old enough or they're evaluated in such a way that they have sufficient understanding of what they're agreeing to."
Shapiro and other ethicists argue that teens are perfectly capable of giving "informed consent"—a key principle in ethics that means fully understanding the benefits and risks of a medical intervention. To give informed consent, a person must be able to process that information in line with their own values. Only then can they make an autonomous choice and sign a consent form, Shapiro says.
Most states already have laws permitting minors to consent to testing and treatments related to sexually transmitted diseases, birth control, behavioral health, and substance abuse. It wouldn't be that much of a stretch to add COVID-19 vaccination to the list, Shapiro says. New Jersey and New York have introduced bills to let teens as young as 14 to consent to getting the COVID-19 vaccine and Minnesota has proposed a bill to allow children as young as 12 to give consent.
With any medical test or intervention, doctors often wrestle with how to best involve teens in conversations about their own health care, says John Lantos, a pediatrician and director of the Bioethics Center at Children's Mercy Kansas City.
"Most bioethicists would say that [teens] should be included to the degree that they have decision-making capacity," he says. "In most cases, that means including them in discussions with their parents in trying to achieve consensus about what the best choice may be."
COVID-19 vaccination also presents a unique circumstance, Lantos notes. It raises the question: Should teens have greater decisional authority because it's a public health emergency? In his opinion, the answer is yes. "COVID-19 has killed millions of people around the world and disrupted the global economy," says pediatrician Lantos. "It's a global catastrophe that requires special rules."
In North Carolina, state legislators are moving to do the opposite. State law currently allows those under 18 to make vaccination decisions on their own, but on Aug. 5, North Carolina's General Assembly approved a Republican-sponsored bill requiring parental consent for 12- to 17-year-olds to get a COVID-19 vaccine.
Kyle Brothers, a pediatrician in Louisville, Kentucky, says it's "ethically justifiable" for states to permit adolescents, especially those on the verge of adulthood, to consent to COVID-19 vaccination and other straightforward medical care.
In many cases, 16- and 17-year-old adolescents are capable of making well-informed decisions, says Brothers, a member of the American Academy of Pediatrics' Section on Bioethics. "The problem is, the law tends not to have that level of nuance," he adds. "We know in the real world that maturing and developing the ability to make decisions is a continuous process, but the law sets a bright line at age 18."
Lacking parental consent, some defiant teens are researching avenues to get vaccinated without their mom's or dad's knowledge. They may have turned to VaxTeen.org, a site operated by a Los Angeles teenager that provides information on consent laws by state.
If parents are wavering on the decision to give consent, Breuner recommends that they speak with a trusted healthcare provider about their specific concerns. These kinds of dialogues often can clarify lingering worries and may help drive up consent rates for teen vaccination.
Vaccine-hesitant parents should hear out their teens who wish to be vaccinated. Teenagers have their own opinions and belief systems, and parents should respect their child's choice to be vaccinated if they wish, considering the minimal risk of harm and the significant benefit to society as a whole.
George J. Annas, professor and director at the Center for Health Law, Ethics & Human Rights at Boston University, says parents have a legal obligation to provide their children with necessary medical treatment, or they could be found guilty of child neglect. The circumstances vary, but in the face of unrelenting COVID-19, he says parents have an ethical duty to consent to teens' vaccination because "the disease is rampant and children are dying."