More Families Are Using Nanny Cams to Watch Elderly Loved Ones, Raising Ethical Questions

Jackie Costanzo and her 93-year-old mom, Louise, are happy to have an extra way to stay connected with the camera, which is normally placed on a television stand facing her mom's bed.
After Jackie Costanzo's mother broke her right hip in a fall, she needed more hands-on care in her assisted-living apartment near Sacramento, California. A social worker from her health plan suggested installing a video camera to help ensure those services were provided.
Without the camera, Costanzo wouldn't have a way to confirm that caregivers had followed through with serving meals, changing clothes, and fulfilling other care needs.
When Costanzo placed the device in May 2018, she informed the administrator and staff, and at first, there were no objections. The facility posted a sign on the apartment's front door, alerting anyone who entered of recording in progress.
But this past spring, a new management company came across the sign and threatened to issue a 30-day eviction notice to her 93-year-old mother, Louise Munch, who has dementia, for violating a policy that prohibits cameras in residents' rooms. With encouragement from California Advocates for Nursing Home Reform, Costanzo researched the state's regulations but couldn't find anything to support or deny camera use. She refused to remove the recording device and prevailed.
"In essence, my mom was 'grandfathered in' because she moved in under a management company that did not specify that residents could not have cameras," says Costanzo, 73, a retired elementary schoolteacher who lives a three-hour drive away, in Silicon Valley, and visits one day every two weeks. Without the camera, Costanzo, who is her mother's only surviving child, wouldn't have a way to confirm that caregivers had followed through with serving meals, changing clothes, and fulfilling other care needs.
As technological innovations enable next of kin to remain apprised of the elderly's daily care in long-term care facilities, surveillance cameras bring legal and privacy issues to the forefront of a complex ethical debate. Families place them overtly or covertly—disguised in a makeshift clock radio, for instance—when they suspect or fear abuse or neglect, so they can maintain a watchful eye, perhaps deterring egregious behavior. But the cameras also capture intimate caregiving tasks, such as bathing and toileting, as well as dressing and undressing, which may undermine the dignity of residents.
So far, laws or guidelines in eight states—Illinois, Maryland, New Mexico, Oklahoma, Texas, Utah, Virginia, and Washington—have granted families the rights to install cameras in a resident's room. In addition, about 15 other states have proposed legislation. Some states, such as Pennsylvania, have put forth regulatory compliance guidance, according to a column published in the July/August 2018 issue of Annals of Long-Term Care.
The increasing prevalence of this legislation has placed it on the radar of long-term care providers. It also suggests a trend to clarify responsible camera use in monitoring services while respecting privacy, says Victor Lane Rose, the column's editor and director of aging services at ECRI Institute, a health care nonprofit near Philadelphia, Pennsylvania.
In most cases, a resident's family installs a camera or instigates a request in hopes of sparing their loved one from the harms of abuse, says James Wright, a family physician who serves as the ethics committee's vice chair of the Society for Post-Acute and Long-Term Care Medicine in Columbia, Maryland. A camera also allows the family to check in on the resident from afar and remain on alert for a potential fall or agitated state, he says.
"It's rare that a facility will have 24-hour presence in a patient's room. You won't have a nurse in there all the time," says Wright, who is also medical director of two long-term care centers and one assisted-living facility around Richmond, Virginia. Particularly "with dementia, the family often wonders" if their loved one is safe.
While offering families peace of mind, he notes that video cameras can also help exonerate caregivers accused of abuse or theft. Hearing aids, which typically cost between $2,000 and $3,000 each, often go missing. By reviewing a video together, families and administrators may find clues to a device's disappearance. Conversely, Wright empathizes with the main counterargument against camera use, which is the belief that "invasion of privacy is also invasion of human dignity."
In respecting modesty, ethical questions abound over whether a camera should be turned off when a patient is in the midst of receiving personal care, such as dressing and undressing or using bedpans. Other ethical issues revolve around who may access the recordings, says Lori Smetanka, executive director of the National Consumer Voice for Quality Long-Term Care in Washington, D.C.
Video cameras, she contends, are only one tool in shielding residents from abuse. They are "not substitutes for personal involvement," she says. "People need to be very vigilant visiting their family members, and facilities have a responsibility to ensure that residents are free of abuse."
Lack of accountability perpetuates abuse in long-term care settings and stems in large part from systemic underfunding.
Educating employees in abuse prevention becomes paramount, and families should ask about staff training before placing their loved one in a long-term care facility, Smetanka says. Prior to installing a camera, she recommends consulting an attorney who is familiar with this issue.
But thoughts of a camera often don't occur to families until an adverse event affects their loved one, says Toby Edelman, a senior policy attorney at the Center for Medicare Advocacy, a nonprofit organization with headquarters in Washington, D.C., and Connecticut.
"These cameras can show exactly what's going on," she explains, noting that prosecutors have used the recordings in litigation. "When residents have injuries of unknown origin" and they can't verbalize what happened to them, "the cameras may document that yes, the resident was actually hit by somebody."
With a resident's safety and security being "the most important consideration," the American Health Care Association in Washington, D.C., which represents long-term and post-acute care providers, supports allowing states, clinicians, and patients to decide about camera use on a local level, says David Gifford, senior vice president of quality and regulatory affairs and chief medical officer.
"We've seen some success with tools such as permissive legislation, where residents and their loved ones have the ability to determine whether a camera is right for them while working with the center openly and ensuring the confidentiality of other residents," says Gifford, who practiced as a geriatrician. "It is important to note, however, that surveillance cameras are still only one element of the quality matrix. We can never hope to truly improve quality care by catching bad actors after the fact."
Lack of accountability perpetuates abuse in long-term care settings and stems in large part from systemic underfunding. Low wages and morale are tied to high turnover, and cameras don't address this overarching problem, says Clara Berridge, an assistant professor of social work at the University of Washington in Seattle, who has co-authored articles on surveillance devices in elder care.
Employees often don't perceive a nursing assistant position as a long-term career trajectory and may not feel vested in the workplace. Training in the recognition and reporting of abuse becomes ineffective when workers quit shortly thereafter. Many must juggle multiple jobs to make ends meet. Staffing shortages are endemic, leading to inadequate oversight of residents and voicing of abuse complaints, she says.
In Berridge's assessment, cameras may do more harm than good. Respondents to a survey she conducted of nursing homes and assisted-living facilities in the United States found that recording devices tend to fuel workers' anxiety amid a culture that further demoralizes and dehumanizes the care they provide.
Consent becomes particularly thorny in shared rooms, which are more common than not in nursing homes. States that permit in-room cameras mandate that roommates or their legal representative be made aware. Even if the camera is directed away from their bed, it will still capture conversations as well as movements that enter its scope. "Surveillance isn't the best way to protect adults in need of support," Berridge says. "Public investment in quality care is."
"The camera is invaluable. But there's no law that says you can have it automatically, so that's wrong."
In the one-bedroom assisted-living apartment where Costanzo's mother lives alone, consent from another resident wasn't needed. Without a roommate, the camera is much less intrusive, although Costanzo wishes she had put one in the living room, not just the bedroom, for more security.
Her safety concerns escalated when she read about a Texas serial killer who smothered victims after gaining access to senior care facilities by "masquerading as a maintenance man." She points to such horrifying incidents, although exceedingly rare, as further justification for permitting cameras to help guard the vulnerable against abuse in long-term care settings. And she hopes to advocate for an applicable law in California.
"The camera is invaluable," says Costanzo, who pays for monthly Wi-Fi service so she can see and interact with her mother, who turns 94 in October, any time of day or night. "But there's no law that says you can have it automatically, so that's wrong."
DNA- and RNA-based electronic implants may revolutionize healthcare
The test tubes contain tiny DNA/enzyme-based circuits, which comprise TRUMPET, a new type of electronic device, smaller than a cell.
Implantable electronic devices can significantly improve patients’ quality of life. A pacemaker can encourage the heart to beat more regularly. A neural implant, usually placed at the back of the skull, can help brain function and encourage higher neural activity. Current research on neural implants finds them helpful to patients with Parkinson’s disease, vision loss, hearing loss, and other nerve damage problems. Several of these implants, such as Elon Musk’s Neuralink, have already been approved by the FDA for human use.
Yet, pacemakers, neural implants, and other such electronic devices are not without problems. They require constant electricity, limited through batteries that need replacements. They also cause scarring. “The problem with doing this with electronics is that scar tissue forms,” explains Kate Adamala, an assistant professor of cell biology at the University of Minnesota Twin Cities. “Anytime you have something hard interacting with something soft [like muscle, skin, or tissue], the soft thing will scar. That's why there are no long-term neural implants right now.” To overcome these challenges, scientists are turning to biocomputing processes that use organic materials like DNA and RNA. Other promised benefits include “diagnostics and possibly therapeutic action, operating as nanorobots in living organisms,” writes Evgeny Katz, a professor of bioelectronics at Clarkson University, in his book DNA- And RNA-Based Computing Systems.
While a computer gives these inputs in binary code or "bits," such as a 0 or 1, biocomputing uses DNA strands as inputs, whether double or single-stranded, and often uses fluorescent RNA as an output.
Adamala’s research focuses on developing such biocomputing systems using DNA, RNA, proteins, and lipids. Using these molecules in the biocomputing systems allows the latter to be biocompatible with the human body, resulting in a natural healing process. In a recent Nature Communications study, Adamala and her team created a new biocomputing platform called TRUMPET (Transcriptional RNA Universal Multi-Purpose GatE PlaTform) which acts like a DNA-powered computer chip. “These biological systems can heal if you design them correctly,” adds Adamala. “So you can imagine a computer that will eventually heal itself.”
The basics of biocomputing
Biocomputing and regular computing have many similarities. Like regular computing, biocomputing works by running information through a series of gates, usually logic gates. A logic gate works as a fork in the road for an electronic circuit. The input will travel one way or another, giving two different outputs. An example logic gate is the AND gate, which has two inputs (A and B) and two different results. If both A and B are 1, the AND gate output will be 1. If only A is 1 and B is 0, the output will be 0 and vice versa. If both A and B are 0, the result will be 0. While a computer gives these inputs in binary code or "bits," such as a 0 or 1, biocomputing uses DNA strands as inputs, whether double or single-stranded, and often uses fluorescent RNA as an output. In this case, the DNA enters the logic gate as a single or double strand.
If the DNA is double-stranded, the system “digests” the DNA or destroys it, which results in non-fluorescence or “0” output. Conversely, if the DNA is single-stranded, it won’t be digested and instead will be copied by several enzymes in the biocomputing system, resulting in fluorescent RNA or a “1” output. And the output for this type of binary system can be expanded beyond fluorescence or not. For example, a “1” output might be the production of the enzyme insulin, while a “0” may be that no insulin is produced. “This kind of synergy between biology and computation is the essence of biocomputing,” says Stephanie Forrest, a professor and the director of the Biodesign Center for Biocomputing, Security and Society at Arizona State University.
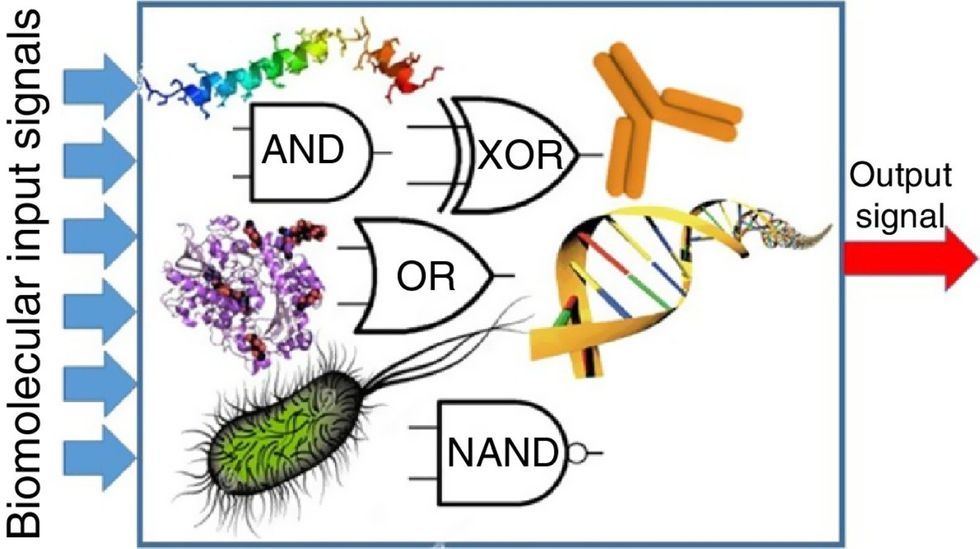
Biocomputing circles are made of DNA, RNA, proteins and even bacteria.
Evgeny Katz
The TRUMPET’s promise
Depending on whether the biocomputing system is placed directly inside a cell within the human body, or run in a test-tube, different environmental factors play a role. When an output is produced inside a cell, the cell's natural processes can amplify this output (for example, a specific protein or DNA strand), creating a solid signal. However, these cells can also be very leaky. “You want the cells to do the thing you ask them to do before they finish whatever their businesses, which is to grow, replicate, metabolize,” Adamala explains. “However, often the gate may be triggered without the right inputs, creating a false positive signal. So that's why natural logic gates are often leaky." While biocomputing outside a cell in a test tube can allow for tighter control over the logic gates, the outputs or signals cannot be amplified by a cell and are less potent.
TRUMPET, which is smaller than a cell, taps into both cellular and non-cellular biocomputing benefits. “At its core, it is a nonliving logic gate system,” Adamala states, “It's a DNA-based logic gate system. But because we use enzymes, and the readout is enzymatic [where an enzyme replicates the fluorescent RNA], we end up with signal amplification." This readout means that the output from the TRUMPET system, a fluorescent RNA strand, can be replicated by nearby enzymes in the platform, making the light signal stronger. "So it combines the best of both worlds,” Adamala adds.
These organic-based systems could detect cancer cells or low insulin levels inside a patient’s body.
The TRUMPET biocomputing process is relatively straightforward. “If the DNA [input] shows up as single-stranded, it will not be digested [by the logic gate], and you get this nice fluorescent output as the RNA is made from the single-stranded DNA, and that's a 1,” Adamala explains. "And if the DNA input is double-stranded, it gets digested by the enzymes in the logic gate, and there is no RNA created from the DNA, so there is no fluorescence, and the output is 0." On the story's leading image above, if the tube is "lit" with a purple color, that is a binary 1 signal for computing. If it's "off" it is a 0.
While still in research, TRUMPET and other biocomputing systems promise significant benefits to personalized healthcare and medicine. These organic-based systems could detect cancer cells or low insulin levels inside a patient’s body. The study’s lead author and graduate student Judee Sharon is already beginning to research TRUMPET's ability for earlier cancer diagnoses. Because the inputs for TRUMPET are single or double-stranded DNA, any mutated or cancerous DNA could theoretically be detected from the platform through the biocomputing process. Theoretically, devices like TRUMPET could be used to detect cancer and other diseases earlier.
Adamala sees TRUMPET not only as a detection system but also as a potential cancer drug delivery system. “Ideally, you would like the drug only to turn on when it senses the presence of a cancer cell. And that's how we use the logic gates, which work in response to inputs like cancerous DNA. Then the output can be the production of a small molecule or the release of a small molecule that can then go and kill what needs killing, in this case, a cancer cell. So we would like to develop applications that use this technology to control the logic gate response of a drug’s delivery to a cell.”
Although platforms like TRUMPET are making progress, a lot more work must be done before they can be used commercially. “The process of translating mechanisms and architecture from biology to computing and vice versa is still an art rather than a science,” says Forrest. “It requires deep computer science and biology knowledge,” she adds. “Some people have compared interdisciplinary science to fusion restaurants—not all combinations are successful, but when they are, the results are remarkable.”
Crickets are low on fat, high on protein, and can be farmed sustainably. They are also crunchy.
In today’s podcast episode, Leaps.org Deputy Editor Lina Zeldovich speaks about the health and ecological benefits of farming crickets for human consumption with Bicky Nguyen, who joins Lina from Vietnam. Bicky and her business partner Nam Dang operate an insect farm named CricketOne. Motivated by the idea of sustainable and healthy protein production, they started their unconventional endeavor a few years ago, despite numerous naysayers who didn’t believe that humans would ever consider munching on bugs.
Yet, making creepy crawlers part of our diet offers many health and planetary advantages. Food production needs to match the rise in global population, estimated to reach 10 billion by 2050. One challenge is that some of our current practices are inefficient, polluting and wasteful. According to nonprofit EarthSave.org, it takes 2,500 gallons of water, 12 pounds of grain, 35 pounds of topsoil and the energy equivalent of one gallon of gasoline to produce one pound of feedlot beef, although exact statistics vary between sources.
Meanwhile, insects are easy to grow, high on protein and low on fat. When roasted with salt, they make crunchy snacks. When chopped up, they transform into delicious pâtes, says Bicky, who invents her own cricket recipes and serves them at industry and public events. Maybe that’s why some research predicts that edible insects market may grow to almost $10 billion by 2030. Tune in for a delectable chat on this alternative and sustainable protein.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Further reading:
More info on Bicky Nguyen
https://yseali.fulbright.edu.vn/en/faculty/bicky-n...
The environmental footprint of beef production
https://www.earthsave.org/environment.htm
https://www.watercalculator.org/news/articles/beef-king-big-water-footprints/
https://www.frontiersin.org/articles/10.3389/fsufs.2019.00005/full
https://ourworldindata.org/carbon-footprint-food-methane
Insect farming as a source of sustainable protein
https://www.insectgourmet.com/insect-farming-growing-bugs-for-protein/
https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/insect-farming
Cricket flour is taking the world by storm
https://www.cricketflours.com/
https://talk-commerce.com/blog/what-brands-use-cricket-flour-and-why/

Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

