The Biggest Challenge for a COVID-19 Vaccine

As scientists race to develop a safe and effective vaccine, companies and governments must figure out how to distribute affordable doses all over the world as fast as possible.
Although no one has conducted a survey on the topic, it's safe to say that a single hope unites much of humanity at the present moment: the prospect of a vaccine for COVID-19, which has infected more than 9 million people worldwide, killed nearly 500,000, and sent the global economy into a tailspin since it first appeared in China last December.
"We've never delivered something to every corner of the world before."
Scientists are racing to make that vision a reality. As of this writing, 11 vaccine candidates are in clinical trials and over 100 others are in preclinical development, in a dozen countries. Pointing to new technology and compressed testing protocols, experts predict a winner could emerge in 12 to 18 months—a fraction of the four years it took to develop the previous record-holder, the mumps vaccine, in the 1960s. Teams at Oxford University and Boston-based Moderna Therapeutics say they could have a product ready even sooner, if the formulas they're testing prove safe and effective. A just-announced White House initiative, Operation Warp Speed, aims to fast-track multiple candidates, with the goal of delivering 100 million doses in November and another 200 million by January 2021.
These timetables could prove wildly over-optimistic. But even if the best-case scenario comes true, and a viable COVID-19 vaccine emerges this fall, a gargantuan challenge remains: getting the shot to everyone who needs it. Epidemiologists figure that at least 70 percent of Earth's population—or 5.6 billion people—would have to be inoculated to achieve "herd immunity," in which each person who catches the disease passes it to less than one other individual. "In order to stop the pandemic, we need to make the vaccine available to almost every person on the planet," Microsoft co-founder Bill Gates blogged in April, as his foundation pledged $300 million to the effort. "We've never delivered something to every corner of the world before."
The difficulties are partly logistical, partly political, and largely a combination of the two. Overcoming those obstacles will require unprecedented cooperation among national governments, international organizations, and profit-minded corporations—in an era when nationalist rivalries are rampant and global leadership is up for grabs.
That may be tougher than developing the vaccine itself.
Logistical Conundrums
Manufacturing and distributing billions of vaccine doses would be a daunting task even in the most harmonious of times. Take the packaging problem. The vaccines under development range from old-school (based on inactivated or weakened viruses) to cutting-edge (using snippets of RNA or DNA to train the immune system to attack the invader). Some may work better than others for different patient groups—the young versus the elderly, for example. All, however, must be stored in vials and administered with syringes.
Among the handful of U.S. companies that manufacture such products, many must import the special glass tubing for vials, as well as the polypropylene for syringe barrels and the rubber or silicone for stoppers and plungers. These materials are commonly sourced from China and India, where lockdowns and export bans restrict supply. Rick Bright, the ousted director of the federal Biomedical Advanced Research and Development Authority (BARDA), claims he was ignored when he warned the Trump Administration that a medical-glass shortage was looming before the coronavirus crisis hit; securing enough to vaccinate 300 million Americans, he told Congress in May, could take up to two years.
Getting the vaccine to poorer countries presents further hurdles. To begin with, there's refrigeration. Inactivated or live vaccines must be kept between 2 and 8 degrees Centigrade (or 35 to 46 degrees Fahrenheit); RNA vaccines typically require much colder temperatures—as low as -80 degrees. This makes storage and transport challenging in parts of the world that lack reliable electricity. DNA vaccines don't need cold storage, but (like RNA vaccines) they remain experimental. They've never been approved to treat any human disease.
Tracking vaccine distribution is another conundrum for low- to-middle-income countries. "Supply chain management is really about information," explains Rebecca Weintraub, assistant professor of global health and social medicine at Harvard Medical School and director of the Better Evidence project at Harvard's Ariadne Labs. "It's about leveraging data to determine demand, predict behavior, and understand the flow of the product itself." Systems for collecting and analyzing such data can be hard to find in poorer regions, she notes. What's more, many people in those areas lack any type of ID card, making it difficult to know who has or hasn't received a vaccine.
Weintraub and two coauthors published an article in April in the Harvard Business Review, suggesting solutions to these and other developing-world problems: solar direct-drive refrigerators, app-based data-capture systems, biometric digital IDs. But such measures—not to mention purchasing adequate supplies of vaccine—would require massive funding.
And that's where the logistical begins to overlap with the political.
Global Access Versus "Vaccine Nationalism"
An array of institutions have already begun laying the groundwork for achieving worldwide, equitable access to COVID-19 vaccines. In February, the World Bank and the Norway-based Coalition for Epidemic Preparedness Innovations (CEPI) cohosted a global consultation on funding vaccine development and manufacturing. In late April, the World Health Organization (WHO), in collaboration with dozens of governments, nonprofits, and industry leaders, launched a program called the Access to COVID-19 Tools Accelerator to expedite such efforts.
Soon afterward, the European Union, along with six countries and the Bill and Melinda Gates Foundation, held a Coronavirus Global Response telethon that raised $8 billion to support Gavi, the Vaccine Alliance—a public-private partnership that subsidizes immunization in low-income countries. The United States and Russia, however, chose not to participate.
This snub by the world's remaining superpower and one of its principal challengers worried many observers. "I am concerned about what I call vaccine nationalism," CEPI executive director Richard Hatchett told the Los Angeles Times. "That's the tension between obligations elected leaders will feel to protect the lives of their citizens" versus the imperative for global sharing.
Some signs point to a possible rerun of the hoarding that accompanied the 2009 H1N1 influenza pandemic, when wealthy nations bought up virtually all vaccine supplies—denying them to poorer countries, and sometimes to one another. Operation Warp Speed has declared an "America First" policy for any vaccine arising from its efforts. Pharma giant Sanofi recently suggested that it would take a similar approach, since the U.S. was first to fund the company's COVID-19 research. (Sanofi's CEO backtracked after officials in France, where the firm is headquartered, protested.) The Oxford group, which is partnering with British-based drug maker AstraZeneca, intends to prioritize Great Britain.
Yet momentum is building for more generous strategies as well. In May, over 100 current and former world leaders, along with prominent economists and public health experts, issued an open letter calling for a "people's vaccine" for COVID-19, which would be patent-free, distributed globally, and available to all countries free of charge. At the WHO's annual World Health Assembly, all 194 member states accepted a resolution urging that vaccines for the disease be made available as a "global public good"—though the U.S. dissociated itself from a clause proposing a patent pool to keep costs down, which it argued might disincentivize "innovators who will be essential to the solutions the whole world needs."
Gavi, for its part, plans to launch a mechanism designed to encourage those innovators while promoting accessibility: an advance market commitment, in which countries pledge to purchase a vaccine, with no money down. Future contributions will be based on the value of the product to their health systems and their ability to pay.
"It's essential to realize that a threat anywhere is a threat everywhere."
A few private-sector players are stepping up, too. U.S.-based Johnson & Johnson, which has received nearly half a billion dollars from the federal government for COVID-19 vaccine research, has promised to provide up to 900 million doses on a not-for-profit basis, if its trials pan out. Other companies have agreed to produce vaccines on a "cost-plus" basis, with a smaller-than-usual profit margin.
How Sharing Can Pay Off
No one knows how all this will work out if and when a vaccine becomes available. (Another wild card: Trump has announced that he is cutting U.S. ties to the WHO over its alleged favoritism toward China, which could hobble the agency's ability to coordinate distribution -- though uncertainty remains about the process of withdrawal and reversing course may still be possible.) To public health experts, however, it's clear that ensuring accessibility is not just a matter of altruism.
"A historic example is smallpox," Rebecca Weintraub observes. "When it kept getting reintroduced into high-income countries from low-income countries, the rich countries realized it was worth investing in the vaccine for countries that couldn't afford it." After a two-decade campaign led by the WHO, the last case of this ancient scourge was diagnosed in 1977.
Conversely, vaccine nationalism doesn't just hurt poor countries. During the H1N1 pandemic, which killed an estimated 284,000 people worldwide, production problems led to shortages in the United States. But Australia stopped a domestic manufacturer from exporting doses to the U.S until all Aussies had been immunized.
Such considerations, Weintraub believes, might help convince even the most reluctant rich-country leaders that an accessible vaccine—if deployed in an epidemiologically targeted way—would serve both the greater good and the national interest. "I suspect the pressures put on our politicians to act globally will be significant," she says.
Other analysts share her guarded optimism. Kelly Moore, who teaches health policy at Vanderbilt University Medical Center, oversaw Tennessee's immunization programs for more than a decade, and later became a member of the Sabin-Aspen Vaccine Science & Policy Group—a panel of international experts that in 2019 released a report titled "Accelerating the Development of a Universal Influenza Vaccine." The 117-page document provided a road map toward a long-sought goal: creating a flu shot that doesn't need to be reformulated each year to target changing viral strains.
"One lesson we learned was that it's crucial to deploy financial resources in a systematic way to support coordination among laboratories that would typically be competitors," Moore says. And that, she adds, is happening with COVID-19, despite nationalist frictions: scientists from Sanofi joining forces with those at rival GSK; researchers at other companies allying with teams at government laboratories; university labs worldwide sharing data across borders. "I have been greatly encouraged to see the amount of global collaboration involved in this enterprise. Partners are working together who would normally never be partners."
For Moore, whose 77-year-old mother survived a bout with the disease, the current pandemic has hit close to home. "It's essential to realize that a threat anywhere is a threat everywhere," she says. "Morally and ethically, we have a tremendous obligation to ensure that the most vulnerable have access to an affordable vaccine, irrespective of where they live."
[Editor's Note: This article was originally published on June 8th, 2020 as part of a standalone magazine called GOOD10: The Pandemic Issue. Produced as a partnership among LeapsMag, The Aspen Institute, and GOOD, the magazine is available for free online. For this reprinting of the article, we have updated the latest statistics on COVID-19 and related global news.]
CORRECTION: A sentence about DNA vaccines incorrectly stated that they require cold storage, like RNA vaccines. The error has been fixed.
A movie still from the 1966 film "Fantastic Voyage"
In the 1966 movie "Fantastic Voyage," actress Raquel Welch and her submarine were shrunk to the size of a cell in order to eliminate a blood clot in a scientist's brain. Now, 55 years later, the scenario is becoming closer to reality.
California-based startup Bionaut Labs has developed a nanobot about the size of a grain of rice that's designed to transport medication to the exact location in the body where it's needed. If you think about it, the conventional way to deliver medicine makes little sense: A painkiller affects the entire body instead of just the arm that's hurting, and chemotherapy is flushed through all the veins instead of precisely targeting the tumor.
"Chemotherapy is delivered systemically," Bionaut-founder and CEO Michael Shpigelmacher says. "Often only a small percentage arrives at the location where it is actually needed."
But what if it was possible to send a tiny robot through the body to attack a tumor or deliver a drug at exactly the right location?
Several startups and academic institutes worldwide are working to develop such a solution but Bionaut Labs seems the furthest along in advancing its invention. "You can think of the Bionaut as a tiny screw that moves through the veins as if steered by an invisible screwdriver until it arrives at the tumor," Shpigelmacher explains. Via Zoom, he shares the screen of an X-ray machine in his Culver City lab to demonstrate how the half-transparent, yellowish device winds its way along the spine in the body. The nanobot contains a tiny but powerful magnet. The "invisible screwdriver" is an external magnetic field that rotates that magnet inside the device and gets it to move and change directions.
The current model has a diameter of less than a millimeter. Shpigelmacher's engineers could build the miniature vehicle even smaller but the current size has the advantage of being big enough to see with bare eyes. It can also deliver more medicine than a tinier version. In the Zoom demonstration, the micorobot is injected into the spine, not unlike an epidural, and pulled along the spine through an outside magnet until the Bionaut reaches the brainstem. Depending which organ it needs to reach, it could be inserted elsewhere, for instance through a catheter.
"The hope is that we can develop a vehicle to transport medication deep into the body," says Max Planck scientist Tian Qiu.
Imagine moving a screw through a steak with a magnet — that's essentially how the device works. But of course, the Bionaut is considerably different from an ordinary screw: "At the right location, we give a magnetic signal, and it unloads its medicine package," Shpigelmacher says.
To start, Bionaut Labs wants to use its device to treat Parkinson's disease and brain stem gliomas, a type of cancer that largely affects children and teenagers. About 300 to 400 young people a year are diagnosed with this type of tumor. Radiation and brain surgery risk damaging sensitive brain tissue, and chemotherapy often doesn't work. Most children with these tumors live less than 18 months. A nanobot delivering targeted chemotherapy could be a gamechanger. "These patients really don't have any other hope," Shpigelmacher says.
Of course, the main challenge of the developing such a device is guaranteeing that it's safe. Because tissue is so sensitive, any mistake could risk disastrous results. In recent years, Bionaut has tested its technology in dozens of healthy sheep and pigs with no major adverse effects. Sheep make a good stand-in for humans because their brains and spines are similar to ours.

The Bionaut device is about the size of a grain of rice.
Bionaut Labs
"As the Bionaut moves through brain tissue, it creates a transient track that heals within a few weeks," Shpigelmacher says. The company is hoping to be the first to test a nanobot in humans. In December 2022, it announced that a recent round of funding drew $43.2 million, for a total of 63.2 million, enabling more research and, if all goes smoothly, human clinical trials by early next year.
Once the technique has been perfected, further applications could include addressing other kinds of brain disorders that are considered incurable now, such as Alzheimer's or Huntington's disease. "Microrobots could serve as a bridgehead, opening the gateway to the brain and facilitating precise access of deep brain structure – either to deliver medication, take cell samples or stimulate specific brain regions," Shpigelmacher says.
Robot-assisted hybrid surgery with artificial intelligence is already used in state-of-the-art surgery centers, and many medical experts believe that nanorobotics will be the instrument of the future. In 2016, three scientists were awarded the Nobel Prize in Chemistry for their development of "the world's smallest machines," nano "elevators" and minuscule motors. Since then, the scientific experiments have progressed to the point where applicable devices are moving closer to actually being implemented.
Bionaut's technology was initially developed by a research team lead by Peer Fischer, head of the independent Micro Nano and Molecular Systems Lab at the Max Planck Institute for Intelligent Systems in Stuttgart, Germany. Fischer is considered a pioneer in the research of nano systems, which he began at Harvard University more than a decade ago. He and his team are advising Bionaut Labs and have licensed their technology to the company.
"The hope is that we can develop a vehicle to transport medication deep into the body," says Max Planck scientist Tian Qiu, who leads the cooperation with Bionaut Labs. He agrees with Shpigelmacher that the Bionaut's size is perfect for transporting medication loads and is researching potential applications for even smaller nanorobots, especially in the eye, where the tissue is extremely sensitive. "Nanorobots can sneak through very fine tissue without causing damage."
In "Fantastic Voyage," Raquel Welch's adventures inside the body of a dissident scientist let her swim through his veins into his brain, but her shrunken miniature submarine is attacked by antibodies; she has to flee through the nerves into the scientist's eye where she escapes into freedom on a tear drop. In reality, the exit in the lab is much more mundane. The Bionaut simply leaves the body through the same port where it entered. But apart from the dramatization, the "Fantastic Voyage" was almost prophetic, or, as Shpigelmacher says, "Science fiction becomes science reality."
This article was first published by Leaps.org on April 12, 2021.
How the Human Brain Project Built a Mind of its Own
In 2013, the Human Brain Project set out to build a realistic computer model of the brain over ten years. Now, experts are reflecting on HBP's achievements with an eye toward the future.
In 2009, neuroscientist Henry Markram gave an ambitious TED talk. “Our mission is to build a detailed, realistic computer model of the human brain,” he said, naming three reasons for this unmatched feat of engineering. One was because understanding the human brain was essential to get along in society. Another was because experimenting on animal brains could only get scientists so far in understanding the human ones. Third, medicines for mental disorders weren’t good enough. “There are two billion people on the planet that are affected by mental disorders, and the drugs that are used today are largely empirical,” Markram said. “I think that we can come up with very concrete solutions on how to treat disorders.”
Markram's arguments were very persuasive. In 2013, the European Commission launched the Human Brain Project, or HBP, as part of its Future and Emerging Technologies program. Viewed as Europe’s chance to try to win the “brain race” between the U.S., China, Japan, and other countries, the project received about a billion euros in funding with the goal to simulate the entire human brain on a supercomputer, or in silico, by 2023.
Now, after 10 years of dedicated neuroscience research, the HBP is coming to an end. As its many critics warned, it did not manage to build an entire human brain in silico. Instead, it achieved a multifaceted array of different goals, some of them unexpected.
Scholars have found that the project did help advance neuroscience more than some detractors initially expected, specifically in the area of brain simulations and virtual models. Using an interdisciplinary approach of combining technology, such as AI and digital simulations, with neuroscience, the HBP worked to gain a deeper understanding of the human brain’s complicated structure and functions, which in some cases led to novel treatments for brain disorders. Lastly, through online platforms, the HBP spearheaded a previously unmatched level of global neuroscience collaborations.
Simulating a human brain stirs up controversy
Right from the start, the project was plagued with controversy and condemnation. One of its prominent critics was Yves Fregnac, a professor in cognitive science at the Polytechnic Institute of Paris and research director at the French National Centre for Scientific Research. Fregnac argued in numerous articles that the HBP was overfunded based on proposals with unrealistic goals. “This new way of over-selling scientific targets, deeply aligned with what modern society expects from mega-sciences in the broad sense (big investment, big return), has been observed on several occasions in different scientific sub-fields,” he wrote in one of his articles, “before invading the field of brain sciences and neuromarketing.”
"A human brain model can simulate an experiment a million times for many different conditions, but the actual human experiment can be performed only once or a few times," said Viktor Jirsa, a professor at Aix-Marseille University.
Responding to such critiques, the HBP worked to restructure the effort in its early days with new leadership, organization, and goals that were more flexible and attainable. “The HBP got a more versatile, pluralistic approach,” said Viktor Jirsa, a professor at Aix-Marseille University and one of the HBP lead scientists. He believes that these changes fixed at least some of HBP’s issues. “The project has been on a very productive and scientifically fruitful course since then.”
After restructuring, the HBP became a European hub on brain research, with hundreds of scientists joining its growing network. The HBP created projects focused on various brain topics, from consciousness to neurodegenerative diseases. HBP scientists worked on complex subjects, such as mapping out the brain, combining neuroscience and robotics, and experimenting with neuromorphic computing, a computational technique inspired by the human brain structure and function—to name just a few.
Simulations advance knowledge and treatment options
In 2013, it seemed that bringing neuroscience into a digital age would be farfetched, but research within the HBP has made this achievable. The virtual maps and simulations various HBP teams create through brain imaging data make it easier for neuroscientists to understand brain developments and functions. The teams publish these models on the HBP’s EBRAINS online platform—one of the first to offer access to such data to neuroscientists worldwide via an open-source online site. “This digital infrastructure is backed by high-performance computers, with large datasets and various computational tools,” said Lucy Xiaolu Wang, an assistant professor in the Resource Economics Department at the University of Massachusetts Amherst, who studies the economics of the HBP. That means it can be used in place of many different types of human experimentation.
Jirsa’s team is one of many within the project that works on virtual brain models and brain simulations. Compiling patient data, Jirsa and his team can create digital simulations of different brain activities—and repeat these experiments many times, which isn’t often possible in surgeries on real brains. “A human brain model can simulate an experiment a million times for many different conditions,” Jirsa explained, “but the actual human experiment can be performed only once or a few times.” Using simulations also saves scientists and doctors time and money when looking at ways to diagnose and treat patients with brain disorders.
Compiling patient data, scientists can create digital simulations of different brain activities—and repeat these experiments many times.
The Human Brain Project
Simulations can help scientists get a full picture that otherwise is unattainable. “Another benefit is data completion,” added Jirsa, “in which incomplete data can be complemented by the model. In clinical settings, we can often measure only certain brain areas, but when linked to the brain model, we can enlarge the range of accessible brain regions and make better diagnostic predictions.”
With time, Jirsa’s team was able to move into patient-specific simulations. “We advanced from generic brain models to the ability to use a specific patient’s brain data, from measurements like MRI and others, to create individualized predictive models and simulations,” Jirsa explained. He and his team are working on this personalization technique to treat patients with epilepsy. According to the World Health Organization, about 50 million people worldwide suffer from epilepsy, a disorder that causes recurring seizures. While some epilepsy causes are known others remain an enigma, and many are hard to treat. For some patients whose epilepsy doesn’t respond to medications, removing part of the brain where seizures occur may be the only option. Understanding where in the patients’ brains seizures arise can give scientists a better idea of how to treat them and whether to use surgery versus medications.
“We apply such personalized models…to precisely identify where in a patient’s brain seizures emerge,” Jirsa explained. “This guides individual surgery decisions for patients for which surgery is the only treatment option.” He credits the HBP for the opportunity to develop this novel approach. “The personalization of our epilepsy models was only made possible by the Human Brain Project, in which all the necessary tools have been developed. Without the HBP, the technology would not be in clinical trials today.”
Personalized simulations can significantly advance treatments, predict the outcome of specific medical procedures and optimize them before actually treating patients. Jirsa is watching this happen firsthand in his ongoing research. “Our technology for creating personalized brain models is now used in a large clinical trial for epilepsy, funded by the French state, where we collaborate with clinicians in hospitals,” he explained. “We have also founded a spinoff company called VB Tech (Virtual Brain Technologies) to commercialize our personalized brain model technology and make it available to all patients.”
The Human Brain Project created a level of interconnectedness within the neuroscience research community that never existed before—a network not unlike the brain’s own.
Other experts believe it’s too soon to tell whether brain simulations could change epilepsy treatments. “The life cycle of developing treatments applicable to patients often runs over a decade,” Wang stated. “It is still too early to draw a clear link between HBP’s various project areas with patient care.” However, she admits that some studies built on the HBP-collected knowledge are already showing promise. “Researchers have used neuroscientific atlases and computational tools to develop activity-specific stimulation programs that enabled paraplegic patients to move again in a small-size clinical trial,” Wang said. Another intriguing study looked at simulations of Alzheimer’s in the brain to understand how it evolves over time.
Some challenges remain hard to overcome even with computer simulations. “The major challenge has always been the parameter explosion, which means that many different model parameters can lead to the same result,” Jirsa explained. An example of this parameter explosion could be two different types of neurodegenerative conditions, such as Parkinson’s and Huntington’s diseases. Both afflict the same area of the brain, the basal ganglia, which can affect movement, but are caused by two different underlying mechanisms. “We face the same situation in the living brain, in which a large range of diverse mechanisms can produce the same behavior,” Jirsa said. The simulations still have to overcome the same challenge.
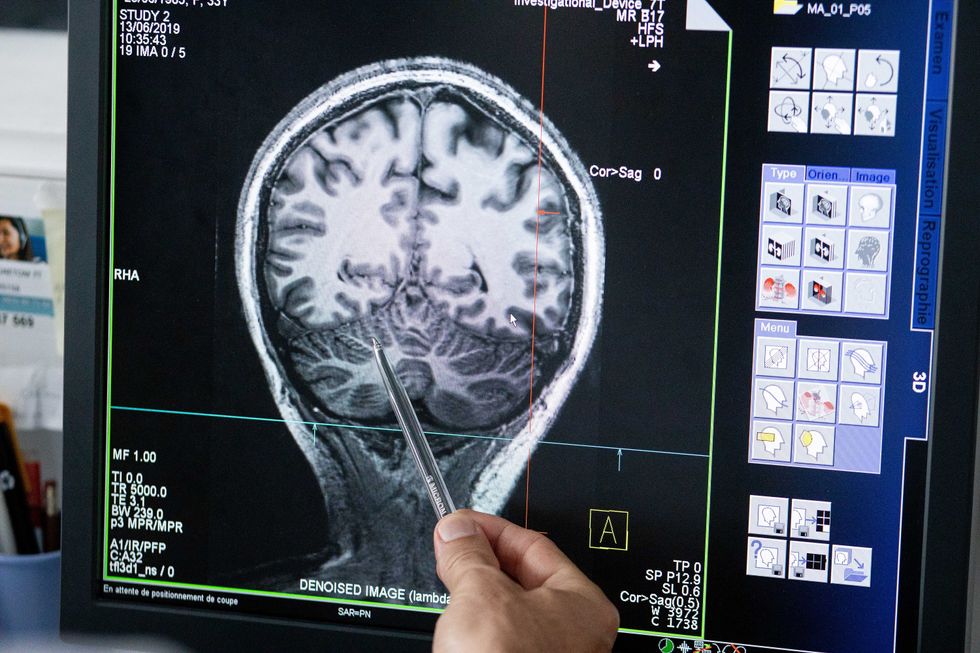
Understanding where in the patients’ brains seizures arise can give scientists a better idea of how to treat them and whether to use surgery versus medications.
The Human Brain Project
A network not unlike the brain’s own
Though the HBP will be closing this year, its legacy continues in various studies, spin-off companies, and its online platform, EBRAINS. “The HBP is one of the earliest brain initiatives in the world, and the 10-year long-term goal has united many researchers to collaborate on brain sciences with advanced computational tools,” Wang said. “Beyond the many research articles and projects collaborated on during the HBP, the online neuroscience research infrastructure EBRAINS will be left as a legacy even after the project ends.”
Those who worked within the HBP see the end of this project as the next step in neuroscience research. “Neuroscience has come closer to very meaningful applications through the systematic link with new digital technologies and collaborative work,” Jirsa stated. “In that way, the project really had a pioneering role.” It also created a level of interconnectedness within the neuroscience research community that never existed before—a network not unlike the brain’s own. “Interconnectedness is an important advance and prerequisite for progress,” Jirsa said. “The neuroscience community has in the past been rather fragmented and this has dramatically changed in recent years thanks to the Human Brain Project.”
According to its website, by 2023 HBP’s network counted over 500 scientists from over 123 institutions and 16 different countries, creating one of the largest multi-national research groups in the world. Even though the project hasn’t produced the in-silico brain as Markram envisioned it, the HBP created a communal mind with immense potential. “It has challenged us to think beyond the boundaries of our own laboratories,” Jirsa said, “and enabled us to go much further together than we could have ever conceived going by ourselves.”