This Special Music Helped Preemie Babies’ Brains Develop

Listening to music helped preterm babies' brains develop, according to the results of a new Swiss study.
Move over, Baby Einstein: New research from Switzerland shows that listening to soothing music in the first weeks of life helps encourage brain development in preterm babies.
For the study, the scientists recruited a harpist and a new-age musician to compose three pieces of music.
The Lowdown
Children who are born prematurely, between 24 and 32 weeks of pregnancy, are far more likely to survive today than they used to be—but because their brains are less developed at birth, they're still at high risk for learning difficulties and emotional disorders later in life.
Researchers in Geneva thought that the unfamiliar and stressful noises in neonatal intensive care units might be partially responsible. After all, a hospital ward filled with alarms, other infants crying, and adults bustling in and out is far more disruptive than the quiet in-utero environment the babies are used to. They decided to test whether listening to pleasant music could have a positive, counterbalancing effect on the babies' brain development.
Led by Dr. Petra Hüppi at the University of Geneva, the scientists recruited Swiss harpist and new-age musician Andreas Vollenweider (who has collaborated with the likes of Carly Simon, Bryan Adams, and Bobby McFerrin). Vollenweider developed three pieces of music specifically for the NICU babies, which were played for them five times per week. Each track was used for specific purposes: To help the baby wake up; to stimulate a baby who was already awake; and to help the baby fall back asleep.
When they reached an age equivalent to a full-term baby, the infants underwent an MRI. The researchers focused on connections within the salience network, which determines how relevant information is, and then processes and acts on it—crucial components of healthy social behavior and emotional regulation. The neural networks of preemies who had listened to Vollenweider's pieces were stronger than preterm babies who had not received the intervention, and were instead much more similar to full-term babies.
Next Up
The first infants in the study are now 6 years old—the age when cognitive problems usually become diagnosable. Researchers plan to follow up with more cognitive and socio-emotional assessments, to determine whether the effects of the music intervention have lasted.
The first infants in the study are now 6 years old—the age when cognitive problems usually become diagnosable.
The scientists note in their paper that, while they saw strong results in the babies' primary auditory cortex and thalamus connections—suggesting that they had developed an ability to recognize and respond to familiar music—there was less reaction in the regions responsible for socioemotional processing. They hypothesize that more time spent listening to music during a NICU stay could improve those connections as well; but another study would be needed to know for sure.
Open Questions
Because this initial study had a fairly small sample size (only 20 preterm infants underwent the musical intervention, with another 19 studied as a control group), and they all listened to the same music for the same amount of time, it's still undetermined whether variations in the type and frequency of music would make a difference. Are Vollenweider's harps, bells, and punji the runaway favorite, or would other styles of music help, too? (Would "Baby Shark" help … or hurt?) There's also a chance that other types of repetitive sounds, like parents speaking or singing to their children, might have similar effects.
But the biggest question is still the one that the scientists plan to tackle next: Whether the intervention lasts as the children grow up. If it does, that's great news for any family with a preemie — and for the baby-sized headphone industry.
Aubrey de Grey at the World Stem Cell Summit in Miami on January 25, 2018.
Aging is not a mystery, says famed researcher Dr. Aubrey de Grey, perhaps the world's foremost advocate of the provocative view that medical technology will one day allow humans to control the aging process and live healthily into our hundreds—or even thousands.
"The cultural attitudes toward all of this are going to be completely turned upside down by sufficiently promising results in the lab, in mice."
He likens aging to a car wearing down over time; as the body operates normally, it accumulates damage which can be tolerated for a while, but eventually sends us into steep decline. The most promising way to escape this biological reality, he says, is to repair the damage as needed with precise scientific tools.
The bad news is that doing this groundbreaking research takes a long time and a lot of money, which has not always been readily available, in part due to a cultural phenomenon he terms "the pro-aging trance." Cultural attitudes have long been fatalistic about the inevitability of aging; many people balk at the seemingly implausible prospect of indefinite longevity.
But the good news for de Grey—and those who are cheering him on—is that his view is becoming less radical these days. Both the academic and private sectors are racing to tackle aging; his own SENS Research Foundation, for one, has spun out into five different companies. Defeating aging, he says, "is not just a future industry; it's an industry now that will be both profitable and extremely good for your health."
De Grey sat down with Editor-in-Chief Kira Peikoff at the World Stem Cell Summit in Miami to give LeapsMag the latest scoop on his work. Here is an edited and condensed version of our conversation.
Since your book Ending Aging was published a decade ago, scientific breakthroughs in stem cell research, genome editing, and other fields have taken the world by storm. Which of these have most affected your research?
They have all affected it a lot in one way, and hardly at all in another way. They have speeded it up--facilitated short cuts, ways to get where we're already trying to go. What they have not done is identified any fundamental changes to the overall strategy. In the book, we described the seven major types of damage, and particular ways of going about fixing each of them, and that hasn't changed.
"Repair at the microscopic level, one would be able to expect to do without surgery, just by injecting the right kind of stem cells."
Has any breakthrough specifically made the biggest impact?
It's not just the obvious things, like iPS (induced pluripotent stem cells) and CRISPR (a precise tool for editing genes). It's also the more esoteric things that applied specifically to certain of our areas, but most people don't really know about them. For example, the identification of how to control something called co-translational mitochondrial protein import.
How much of the future of anti-aging treatments will involve regeneration of old tissue, or wholesale growth of new organs?
The more large-scale ones, regenerating whole new organs, are probably only going to play a role in the short-term and will be phased out relatively rapidly, simply because, in order to be useful, one has to employ surgery, which is really invasive. We'll want to try to get around that, but it seems quite likely that in the very early stages, the techniques we have for repairing things at the molecular and cellular level in situ will be insufficiently comprehensive, and so we will need to do the more sledgehammer approach of building a whole new organ and sticking it in.
Every time you are in a position where you're replacing an organ, you have the option, in principle, of repairing the organ, without replacing it. And repair at the microscopic level, one would be able to expect to do without surgery, just by injecting the right kind of stem cells or whatever. That would be something one would expect to be able to apply to someone much closer to death's door and much more safely in general, and probably much more cheaply. One would expect that subsequent generations of these therapies would move in that direction.
Your foundation is working on an initiative requiring $50 million in funding—
Well, if we had $50 million per year in funding, we could go about three times faster than we are on $5 million per year.
And you're looking at a 2021 timeframe to start human trials?
That's approximate. Remember, because we accumulate in the body so many different types of damage, that means we have many different types of therapy to repair that damage. And of course, each of those types has to be developed independently. It's very much a divide and conquer therapy. The therapies interact with each other to some extent; the repair of one type of damage may slow down the creation of another type of damage, but still that's how it's going to be.
And some of these therapies are much easier to implement than others. The easier components of what we need to do are already in clinical trials—stem cell therapies especially, and immunotherapy against amyloid in the brain, for example. Even in phase III clinical trials in some cases. So when I talk about a timeframe like 2021, or early 20s shall we say, I'm really talking about the most difficult components.
What recent strides are you most excited about?
Looking back over the past couple of years, I'm particularly proud of the successes we've had in the very most difficult areas. If you go through the 7 components of SENS, there are two that have absolutely been stuck in a rut and have gotten nowhere for 15 to 20 years, and we basically fixed that in both cases. We published two years ago in Science magazine that essentially showed a way forward against the stiffening of the extracellular matrix, which is responsible for things like wrinkles and hypertension. And then a year ago, we published a real breakthrough paper with regard to placing copies of the mitochondria DNA in the nuclear DNA modified in such a way that they still work, which is an idea that had been around for 30 years; everyone had given up on it, some a long time ago, and we basically revived it.
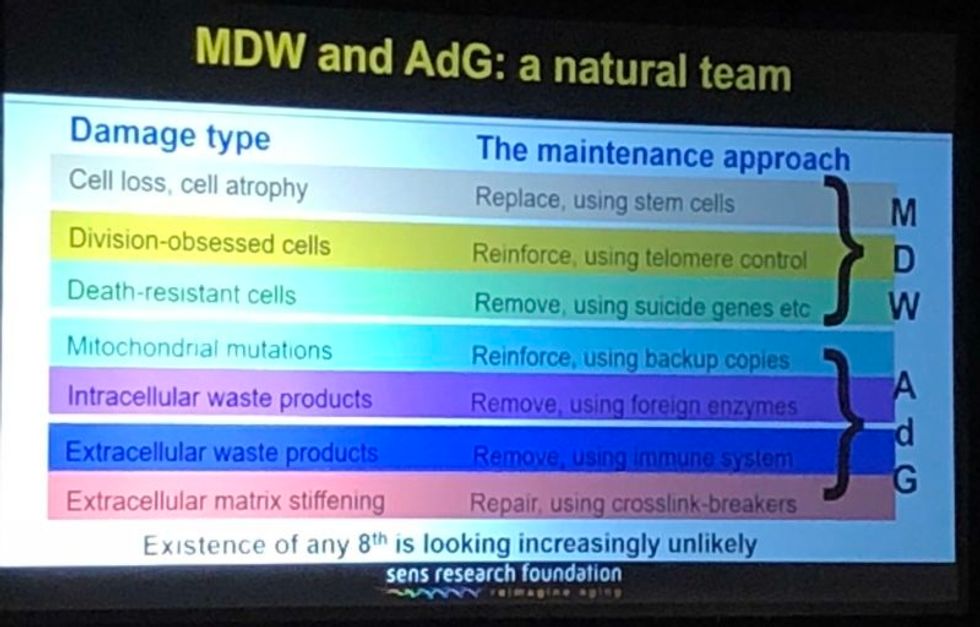
A slide presented by Aubrey de Grey, referencing his collaboration with Mike West at AgeX, showing the 7 types of damage that he believes must be repaired to end aging.
(Courtesy Kira Peikoff)
That's exciting. What do you think are the biggest barriers to defeating aging today: the technological challenges, the regulatory framework, the cost, or the cultural attitude of the "pro-aging" trance?
One can't really address those independently of each other. The technological side is one thing; it's hard, but we know where we're going, we've got a plan. The other ones are very intertwined with each other. A lot of people are inclined to say, the regulatory hurdle will be completely insurmountable, plus people don't recognize aging as a disease, so it's going to be a complete nonstarter. I think that's nonsense. And the reason is because the cultural attitudes toward all of this are going to be completely turned upside down before we have to worry about the regulatory hurdles. In other words, they're going to be turned upside down by sufficiently promising results in the lab, in mice. Once we get to be able to rejuvenate actually old mice really well so they live substantially longer than they otherwise would have done, in a healthy state, everyone's going to know about it and everyone's going to demand – it's not going to be possible to get re-elected unless you have a manifesto commitment to turn the FDA completely upside down and make sure this happens without any kind of regulatory obstacle.
I've been struggling away all these years trying to bring little bits of money in the door, and the reason I have is because of the skepticism as to regards whether this could actually work, combined with the pro-aging trance, which is a product of the skepticism – people not wanting to get their hopes up, so finding excuses about aging being a blessing in disguise, so they don't have to think about it. All of that will literally disintegrate pretty much overnight when we have the right kind of sufficiently impressive progress in the lab. Therefore, the availability of money will also [open up]. It's already cracking: we're already seeing the beginnings of the actual rejuvenation biotechnology industry that I've been talking about with a twinkle in my eye for some years.
"For humans, a 50-50 chance would be twenty years at this point, and there's a 10 percent chance that we won't get there for a hundred years."
Why do you think the culture is starting to shift?
There's no one thing yet. There will be that tipping point I mentioned, perhaps five years from now when we get a real breakthrough, decisive results in mice that make it simply impossible to carry on being fatalistic about all this. Prior to that, what we're already seeing is the impact of sheer old-school repeat advertising—me going out there, banging away and saying the same fucking thing again and again, and nobody saying anything that persuasively knocks me down. … And it's also the fact that we are making incremental amounts of progress, not just ourselves, but the scientific community generally. It has become incrementally more plausible that what I say might be true.
I'm sure you hate getting the timeline question, but if we're five years away from this breakthrough in mice, it's hard to resist asking—how far is that in terms of a human cure?
When I give any kind of timeframes, the only real care I have to take is to emphasize the variance. In this case I think we have got a 50-50 chance of getting to that tipping point in mice within five years from now, certainly it could be 10 or 15 years if we get unlucky. Similarly, for humans, a 50-50 chance would be twenty years at this point, and there's a 10 percent chance that we won't get there for a hundred years.
"I don't get people coming to me saying, well I don't think medicine for the elderly should be done because if it worked it would be a bad thing. People like to ignore this contradiction."
What would you tell skeptical people are the biggest benefits of a very long-lived population?
Any question about the longevity of people is the wrong question. Because the longevity that people fixate about so much will only ever occur as a side effect of health. However long ago you were born or however recently, if you're sick, you're likely to die fairly soon unless we can stop you being sick. Whereas if you're healthy, you're not. So if we do as well as we think we can do in terms of keeping people healthy and youthful however long ago they were born, then the side effect in terms of longevity and life expectancy is likely to be very large. But it's still a side effect, so the way that people actually ought to be—in fact have a requirement to be—thinking, is about whether they want people to be healthy.
Now I don't get people coming to me saying, well I don't think medicine for the elderly should be done because if it worked it would be a bad thing. People like to ignore this contradiction, they like to sweep it under the carpet and say, oh yeah, aging is totally a good thing.
People will never actually admit to the fact that what they are fundamentally saying is medicine for the elderly, if it actually works, would be bad, but still that is what they are saying.
Shifting gears a bit, I'm curious to find out which other radical visionaries in science and tech today you most admire?
Fair question. One is Mike West. I have the great privilege that I now work for him part-time with Age X. I have looked up to him very much for the past ten years, because what he did over the past 20 years starting with Geron is unimaginable today. He was working in an environment where I would not have dreamt of the possibility of getting any private money, any actual investment, in something that far out, that far ahead of its time, and he did it, again and again. It's insane what he managed to do.
What about someone like Elon Musk?
Sure, he's another one. He is totally impervious to the caution and criticism and conservatism that pervades humanity, and he's getting on making these bloody self-driving cars, space tourism, and so on, making them happen. He's thinking just the way I'm thinking really.
"You can just choose how frequently and how thoroughly you repair the damage. And you can make a different choice next time."
You famously said ten years ago that you think the first person to live to 1000 is already alive. Do you think that's still the case?
Definitely, yeah. I can't see how it could not be. Again, it's a probabilistic thing. I said there's at least a 10 percent chance that we won't get to what I call Longevity Escape Velocity for 100 years and if that's true, then the statement about 1000 years being alive already is not going to be the case. But for sure, I believe that the beneficiaries of what we may as well call SENS 1.0, the point where we get to LEV, those people are exceptionally unlikely ever to suffer from any kind of ill health correlated with their age. Because we will never fall below Longevity Escape Velocity once we attain it.
Could someone who was just born today expect—
I would say people in middle age now have a fair chance. Remember – a 50/50 chance of getting to LEV within 20 years, and when you get there, you don't just stay at biologically 70 or 80, you are rejuvenated back to biologically 30 or 40 and you stay there, so your risk of death each year is not related to how long ago you were born, it's the same as a young adult. Today, that's less than 1 in 1000 per year, and that number is going to go down as we get self-driving cars and all that, so actually 1000 is a very conservative number.
So you would be able to choose what age you wanted to go back to?
Oh sure, of course, it's just like a car. What you're doing is you're repairing damage, and the damage is still being created by the body's metabolism, so you can just choose how frequently and how thoroughly you repair the damage. And you can make a different choice next time.
What would be your perfect age?
I have no idea. That's something I don't have an opinion about, because I could change it whenever I like.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Why Blindness Will Be the First Disorder Cured by Futuristic Treatments
A blind man with a cane goes for a walk at sunset. (© Prazis/Fotolia)
Stem cells and gene therapy were supposed to revolutionize biomedicine around the turn of the millennium and provide relief for desperate patients with incurable diseases. But for many, progress has been frustratingly slow. We still cannot, for example, regenerate damaged organs like a salamander regrows its tail, and genome engineering is more complicated than cutting and pasting letters in a word document.
"There are a number of things that make [the eye] ideal for new experimental therapies which are not true necessarily in other organs."
For blind people, however, the future of medicine is one step closer to reality. In December, the FDA approved the first gene therapy for an inherited disease—a mutation in the gene RPE65 that causes a rare form of blindness. Several clinical trials also show promise for treating various forms of retinal degeneration using stem cells.
"It's not surprising that the first gene therapy that was approved by the FDA was a therapy in the eye," says Bruce Conklin, a senior investigator at the San Francisco-based Gladstone Institutes, a nonprofit life science research organization, and a professor in the Medical Genetics and Molecular Pharmacology department at the University of California, San Francisco. "There are a number of things that make it ideal for new experimental therapies which are not true necessarily in other organs."
Physicians can easily see into the eye to check if a procedure worked or if it's causing problems. "The imaging technology within the eye is really unprecedented. You can't do this in someone's spinal cord or someone's brain cells or immune system," says Conklin, who is also deputy director of the Innovative Genomics Institute.
There's also a built-in control: researchers can test an intervention on one eye first. What's more, if something goes wrong, the risk of mortality is low, especially when compared to experimenting on the heart or brain. Most types of blindness are currently incurable, so the risk-to-reward ratio for patients is high. If a problem arises with the treatment their eyesight could get worse, but if they do nothing their vision will likely decline anyway. And if the treatment works, they may be able to see for the first time in years.
Gene Therapy
An additional appeal for testing gene therapy in the eye is the low risk for off-target effects, in which genome edits could result in unintended changes to other genes or in other cell types. There are a number of genes that are solely expressed in the eye and not in any other part of the body. Manipulating those genes will only affect cells in the eye, so concerns about the impact on other organs are minimal.
Ninety-three percent of patients who received the injection had improved vision just one month after treatment.
RPE65 is one such gene. It creates an enzyme that helps the eye convert light into an electrical signal that travels back to the brain. Patients with the mutation don't produce the enzyme, so visual signals are not processed. However, the retinal cells in the eye remain healthy for years; if you can restore the missing enzyme you can restore vision.
The newly approved therapy, developed by Spark Therapeutics, uses a modified virus to deliver RPE65 into the eye. A retinal surgeon injects the virus, which has been specially engineered to remove its disease-causing genes and instead carry the correct RPE65 gene, into the retina. There, it is sucked up by retinal pigment epithelial (RPE) cells. The RPE cells are a particularly good target for injection because their job is to eat up and recycle rogue particles. Once inside the cell, the virus slips into the nucleus and releases the DNA. The RPE65 gene then goes to work, using the cell's normal machinery to produce the needed enzyme.
In the most recent clinical trial, 93 percent of patients who received the injection—who range in age from 4 to 44—had improved vision just one month after treatment. So far, the benefits have lasted at least two years.
"It's an exciting time for this class of diseases, where these people have really not had treatments," says Spark president and co-founder, Katherine High. "[Gene therapy] affords the possibility of treatment for diseases that heretofore other classes of therapeutics really have not been able to help."
Stem Cells
Another benefit of the eye is its immune privilege. In order to let light in, the eye must remain transparent. As a result, its immune system is dampened so that it won't become inflamed if outside particles get in. This means the eye is much less likely to reject cell transplants, so patients do not need to take immunosuppressant drugs.
One study generating buzz is a clinical trial in Japan that is the first and, so far, only test of induced pluripotent stem cells in the eye.
Henry Klassen, an assistant professor at UC Irvine, is taking advantage of the eye's immune privilege to transplant retinal progenitor cells into the eye to treat retinitis pigmentosa, an inherited disease affecting about 1 in 4000 people that eventually causes the retina to degenerate. The disease can stem from dozens of different genetic mutations, but the result is the same: RPE cells die off over the course of a few decades, leaving the patient blind by middle age. It is currently incurable.
Retinal progenitor cells are baby retinal cells that develop naturally from stem cells and will turn into one of several types of adult retinal cells. When transplanted into a patient's eye, the progenitor cells don't replace the lost retinal cells, but they do secrete proteins and enzymes essential for eye health.
"At the stage we get the retinal tissue it's immature," says Klassen. "They still have some flexibility in terms of which mature cells they can turn into. It's that inherent flexibility that gives them a lot of power when they're put in the context of a diseased retina."
Klassen's spin-off company, jCyte, sponsored the clinical trial with support from the California Institute for Regenerative Medicine. The results from the initial study haven't been published yet, but Klassen says he considers it a success. JCyte is now embarking on a phase two trial to assess improvements in vision after the treatment, which will wrap up in 2021.
Another study generating buzz is a clinical trial in Japan that is the first and, so far, only test of induced pluripotent stem cells (iPSC) in the eye. iPSC are created by reprogramming a patient's own skin cells into stem cells, circumventing any controversy around embryonic stem cell sources. In the trial, led by Masayo Takahashi at RIKEN, the scientists transplant retinal pigment epithelial cells created from iPSC into the retinas of patients with age-related macular degeneration. The first woman to receive the treatment is doing well, and her vision is stable. However, the second patient suffered a swollen retina as a result of the surgery. Despite this recent setback, Takahashi said last week that the trial would continue.
Botched Jobs
Although recent studies have provided patients with renewed hope, the field has not been without mishap. Most notably, an article in the New England Journal of Medicine last March described three patients who experienced severe side effects after receiving stem cell injections from a Florida clinic to treat age-related macular degeneration. Following the initial article, other reports came out about similar botched treatments. Lawsuits have been filed against US Stem Cell, the clinic that conducted the procedure, and the FDA sent them a warning letter with a long list of infractions.
"One red flag is that the clinics charge patients to take part in the treatment—something extremely unusual for legitimate clinical trials."
Ajay Kuriyan, an ophthalmologist and retinal specialist at the University of Rochester who wrote the paper, says that because details about the Florida trial are scarce, it's hard to say why the treatment caused the adverse reaction. His guess is that the stem cells were poorly prepared and not up to clinical standards.
Klassen agrees that small clinics like US Stem Cell do not offer the same caliber of therapy as larger clinical trials. "It's not the same cells and it's not the same technique and it's not the same supervision and it's not under FDA auspices. It's just not the same thing," he says. "Unfortunately, to the patient it might sound the same, and that's the tragedy for me."
For patients who are interested in joining a trial, Kuriyan listed a few things to watch out for. "One red flag is that the clinics charge patients to take part in the treatment—something extremely unusual for legitimate clinical trials," he says. "Another big red flag is doing the procedure in both eyes" at the same time. Third, if the only treatment offered is cell therapy. "These clinics tend to be sort of stand-alone clinics, and that's not very common for an actual big research study of this scale."
Despite the recent scandal, Klassen hopes that the success of his trial and others will continue to push the field forward. "It just takes so many decades to move this stuff along, even when you're trying to simplify it as much as possible," he says. "With all the heavy lifting that's been done, I hope the world's got the patience to get this through."

